Abnormalities on the resting electrocardiogram (ECG) are predictors of mortality and cardiovascular events among asymptomatic adults. The aim of this study was to estimate the prevalence of ECG abnormalities in adults and their association with cardiovascular risk factors.
MethodsWe performed a cross-sectional analysis of ECGs in adults aged 19–59 years, living in Tubarão, Santa Catarina, Brazil. Data were collected between November 2011 and July 2012. Electrocardiographic findings were classified according to the guidelines of the Brazilian Society of Cardiology on analyzing and issuing electrocardiographic reports, and were divided into major abnormalities, minor abnormalities and no changes, as in previous studies. Pearson's chi-square test and ANOVA were used to analyze the association of ECG parameters with traditional cardiovascular risk factors.
ResultsA total of 361 participants were studied. Mean age was 40.4±12.2 years; 232 (64.3%) were women. Minor abnormalities were found in 16.9% and major abnormalities in 3.3%. Among the risk factors examined, gender, smoking, alcohol consumption, systemic hypertension, diabetes, and high Framingham risk score were significantly associated with major and minor ECG changes.
ConclusionsThe prevalence of electrocardiographic changes was 20.2% in the population surveyed, the majority being minor. Both major and minor electrocardiographic abnormalities showed significant associations with risk of coronary artery disease, and may predict cardiovascular risk in asymptomatic adults.
Anormalidades em um eletrocardiograma (ECG) de repouso são fatores preditores de mortalidade e eventos cardiovasculares entre adultos assintomáticos. Estimar a prevalência de anormalidades eletrocardiográficas em adultos e possível associação com fatores de risco.
MétodosEstudo transversal que avaliou adultos com idade entre 19-59 anos, provenientes do município de Tubarão (SC). A colheita dos dados ocorreu entre novembro de 2011 a julho de 2012. Os laudos eletrocardiográficos foram classificados de acordo com a diretriz da Sociedade Brasileira de Cardiologia sobre Análise e Emissão de Laudos Eletrocardiográficos e divididos em anormalidades maiores, anormalidades menores e sem alterações, conforme estudos anteriores. Para a associação do ECG com os tradicionais fatores de risco cardiovasculares foi utilizado o método qui-quadrado de Pearson ou ANOVA.
ResultadosForam estudados 361 participantes, a média de idade foi de 40,4 (DP=12,2) anos e 232 (64,3%) eram mulheres. Verificou-se 16,9% de anormalidades menores e 3,3% de anormalidades maiores. Dentre os fatores de risco estudados, sexo, tabagismo, alcoolismo, hipertensão arterial sistémica, diabetes mellitus, e maior score de risco de Framingham (ERF) estiveram associados significativamente às alterações maiores e menores do ECG.
ConclusõesHouve prevalência de 20,2% de alterações eletrocardiográficas na população estudada, sendo a maioria de anormalidades menores. As anormalidades eletrocardiográficas maiores e menores tiveram associações significativas com fatores de risco de doença arterial coronária, podendo este exame predizer risco cardiovascular em populações adultas assintomáticas.
Cardiovascular disease (CVD) is associated with high rates of morbidity and mortality in developed countries, and has been the leading cause of mortality in Brazil since the 1960s. In 2008 CVD accounted for 31.8% of mortality in the country as a whole and 38% of deaths recorded in the municipality of Tubarão, Santa Catarina.1
CVD is responsible for high health costs and affects a large proportion of the working population. Its economic impact in Brazil is demonstrated by the following figures: it accounts for 65% of deaths in adults aged 30–69 years, 14% of hospital admissions in this age-group (1150000 hospitalizations/year) and 40% of early retirements.2 The causes of CVD are multifactorial and its prevention depends on control of cardiovascular risk factors, including smoking, obesity, dyslipidemia, systemic hypertension, sedentary life styles and diabetes.3–5
Abnormalities on the resting electrocardiogram (ECG) are an independent predictor of the development of coronary artery disease (CAD) and are associated with increased mortality and cardiovascular risk.6–10 Abnormal Q waves on the ECG may indicate a silent or unrecognized myocardial infarction. In the Framingham study, a quarter of non-fatal infarctions were only detected through ECG changes.11–13
Against this background, besides patient history and clinical examination, the ECG is also useful in cardiovascular epidemiology, due to its low cost, accessibility, safety, and ability to predict cardiovascular risk.8,10
The aim of this study was to estimate the prevalence of major and minor ECG abnormalities and their association with the main risk factors for CAD in the adult population of Tubarão, Santa Catarina.
MethodsThe study was approved by the Ethics and Research Committee of the University of Southern Santa Catarina (UNISUL). It was sponsored by the Foundation for Research and Innovation of the State of Santa Catarina (FAPESC), and is part of the Tubarão Adult Health Study (ESATU), in a partnership between the Center for Clinical Research of Hospital Nossa Senhora da Conceição, UNISUL and the Municipal Health Secretariat.
We performed an epidemiological, cross-sectional, population-based study between November 2011 and June 2012 in adults aged 19–59 years of both sexes living in the municipality of Tubarão, Santa Catarina, Brazil. Pregnant women, individuals unable to travel to the data collection point, and those unable to freely decide on their participation were excluded, as were those who did not undergo ECG or laboratory testing.
To calculate the sample size, we used an estimate of 36% of ECG abnormalities8 with a level of significance of 5% and a margin of error of 1%, which resulted in a minimum sample of 353 individuals for a 95% confidence interval, based on an adult population in Tubarão of 62537 (2010 census).
The participants were selected through simple random sampling based on house numbers in each of the 250 micro areas of the municipality registered in 27 family health units. Each micro area has a community health worker who carries out regular home visits, and the service is estimated to cover 90% of the resident population. The randomly selected house numbers were 4, 36, 27, 10 and 32. Community health workers visited the first house selected (number 4) in their area and invited the resident to participate in the study in accordance with the inclusion and exclusion criteria. If there were no adults at home or if they refused to participate in the study, the health workers proceeded to the next selected house (number 10) until each had recruited one or two participants per micro area.
Data collection took place on Saturday mornings in outpatient consultations arranged with the participants in branches of Hospital Nossa Senhora da Conceição. Participating individuals were requested to fast for 12 hours and to abstain from alcohol in the 72 hours prior to the consultation.
After their informed consent was obtained, the participants were interviewed, with the following data being recorded: sociodemographic (age, gender and level of education, as indicated by number of years of schooling), behavioral (sedentarism, alcohol consumption and smoking) and clinical (history of CVD and medications). Individuals who had smoked at least 100 cigarettes in their lives were considered smokers.14 The CAGE questionnaire was applied in those who stated they drank alcohol.15 The short-form International Physical Activity Questionnaire was used to assess the level of exercise.16,17
Height and weight were measured to determine body mass index (BMI), individuals with BMI ≥30 kg/m2 being considered obese; 10 ml of peripheral venous blood was collected for assessment of total, HDL and LDL cholesterol (HDL-C and LDL-C), triglycerides (TG), blood glucose and creatinine.
A diagnosis of dyslipidemia was based on changes in one or more of the four parameters measured: isolated hypercholesterolemia (LDL-C ≥160 mg/dl); isolated hypertriglyceridemia (TG ≥150 mg/dl); mixed hyperlipidemia (LDL-C ≥160 mg/dl and TG ≥150 mg/dl); and low HDL-C (<40 mg/dl in men and <50 mg/dl in women), either isolated or associated with increased LDL-C or TG.3
Systemic hypertension was assessed in accordance with the 2010 guidelines of the Brazilian Society of Cardiology, with three blood pressure (BP) measurements being taken at one-minute intervals,18 using an Omron HEM-742INT automatic sphygmomanometer. Patients were classified as hypertensive if they presented mean systolic or diastolic BP ≥140 or ≥90 mmHg, respectively, or were under antihypertensive therapy. Patients with a previous diagnosis of diabetes or taking hypoglycemic medication and those with fasting glucose >126 mg/dl were considered diabetic. The participants were categorized according to their Framingham risk score as low (<10%), intermediate (10%–20%) or high risk (>20%).19
The ECG was performed using a C10+ digital electrocardiograph, with the patient at rest in dorsal decubitus. The recordings were sent to a cardiologist, who established the diagnoses in accordance with the guidelines of the Brazilian Society of Cardiology on analyzing and issuing electrocardiographic reports.20 The results were divided into major and minor abnormalities or no changes, as in previous studies.6–10
Abnormalities of ventricular repolarization were defined as significant changes in the polarity, duration or morphology of the J point, ST segment, T wave or U wave in the absence of alterations that met the definition of ischemic waves or other specific diagnostic features such as chamber overload or intraventricular block. Increased corrected QT interval was considered separately from the above alterations. Subepicardial ischemia was diagnosed in the presence of negative, symmetrical and sharp T waves.20
OpenEpi software, version 2.3.1, was used to calculate the sample size. The data were entered into EpiData, version 3.1 (EpiData Association, Odense, Denmark) and SPSS for Windows, version 19 (Chicago, IL, USA) was used for the statistical analysis. Descriptive statistics with frequencies and measures of central tendency and dispersion were used to summarize the data. Pearson's chi-square test and one-way ANOVA were used to analyze the association between the variables under study, with a 95% confidence interval.
ResultsA total of 361 participants were studied. Mean age was 40.4±12.2 years, 232 (64.3%) were women and 312 (86.4%) were white.
Minor abnormalities were found in 61 individuals (16.9%), major abnormalities in 12 (3.3%), and 288 (79.8%) had no abnormalities. Table 1 shows the ECG changes observed among the participants.
Changes found in electrocardiographic reports (n=73).
| Minor abnormalities | n=61 |
|---|---|
| Alterations in ventricular repolarization | 21 |
| Right bundle branch conduction disturbances | 13 |
| Sinus bradycardia | 8 |
| Left anterior fascicular block | 7 |
| Early repolarization | 4 |
| Left axis deviation | 3 |
| Junctional rhythm | 2 |
| Isolated monomorphic ventricular extrasystoles | 2 |
| First-degree atrioventricular block | 1 |
| Major abnormalities | n=12 |
|---|---|
| Inferior subepicardial ischemia | 2 |
| Short PR and delta wave suggestive of WPW syndrome | 1 |
| Inferior infarction scar | 2 |
| Anteroseptal infarction scar | 2 |
| Septal infarction scar | 1 |
| Early repolarization in V1 and V6, possible biatrial overload | 1 |
| Anterior superior fascicular block, right bundle branch block | 1 |
| Anteroseptal subepicardial ischemia | 1 |
| Infarction scar and inferior subepicardial ischemia | 1 |
WPW: Wolff-Parkinson-White.
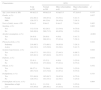
Table 2 shows the sociodemographic and clinical characteristics of the study population according to ECG results.
Sociodemographic and clinical characteristics according to electrocardiographic results.
| Characteristics | ECG | ||||
|---|---|---|---|---|---|
| Total n=361 | Normal n=288 | Minor abnormalities n=61 | Major abnormalities n=12 | p* | |
| Age, years (mean ± SD) | 40.4±12.3 | 40.0±12.0 | 41.0±13.5 | 47.2±10.3 | 0.133 |
| Gender, n (%) | 0.037 | ||||
| Female | 232 (64.3) | 194 (67.4) | 33 (54.1) | 5 (41.7) | |
| Male | 129 (35.7) | 94 (32.6) | 28 (45.9) | 7 (58.3) | |
| Years of study, mean ± SD | 8.8±4.3 | 9.0±4.3 | 8.4±4.2 | 7.6±3.4 | 0.403 |
| Smoking, n (%) | 0.002 | ||||
| Yes | 112 (31.0) | 82 (28.5) | 21 (34.4) | 9 (75.0) | |
| No | 249 (69.0) | 206 (71.5) | 40 (65.6) | 3 (25.0) | |
| Alcohol consumption, n (%) | <0.001 | ||||
| Yes | 29 (8.0) | 20 (6.9) | 4 (6.6) | 5 (41.7) | |
| No | 332 (92.0) | 268 (93.1) | 57 (93.4) | 7 (58.3) | |
| Physical activity, n (%) | 0.842 | ||||
| Sedentary | 219 (60.7) | 173 (60.1) | 39 (63.9) | 7 (58.3) | |
| Active | 142 (39.3) | 115 (39.9) | 22 (36.1) | 5 (41.7) | |
| Systemic hypertension, n (%) | 0.044 | ||||
| Yes | 136 (37.7) | 101 (35.1) | 27 (44.3) | 8 (66.7) | |
| No | 225 (62.3) | 187 (64.9) | 34 (55.7) | 4 (33.3) | |
| Diabetes, n (%) | 0.019 | ||||
| Yes | 22 (6.1) | 15 (5.2) | 4 (6.6) | 3 (25.0) | |
| No | 339 (93.9) | 273 (94.8) | 57 (93.4) | 9 (75.0) | |
| Obesity, n (%) | 0.552 | ||||
| Yes | 98 (27.1) | 75 (26.0) | 20 (32.8) | 3 (25.0) | |
| No | 263 (72.9) | 213 (74.0) | 41 (67.2) | 9 (75.0) | |
| Dyslipidemia, n (%) | 0.753 | ||||
| Yes | 233 (64.9) | 185 (64.7) | 39 (63.9) | 9 (75.0) | |
| No | 126 (35.1) | 101 (35.3) | 22 (36.1) | 3 (25.0) | |
| Framingham risk score, n (%) | 0.004 | ||||
| Intermediate or high | 18 (5.1) | 11 (3.9) | 4 (6.6) | 3 (25.0) | |
| Low | 335 (94.9) | 269 (96.1) | 57 (93.4) | 9 (75.0) | |
ECG: electrocardiogram; SD: standard deviation.
The results show that major and minor abnormalities were mainly associated with female gender, smoking, alcohol consumption, hypertension and diabetes, as well as intermediate or high Framingham risk score.
DiscussionIn our study minor ECG abnormalities were more prevalent than major ones (16.9% vs. 3.3%, respectively). These percentages are lower than in population studies in the US8–10; an American study of 14749 women aged 40–55 years found 27.8% had minor abnormalities and 6.3% major abnormalities.10 Another American study, involving 2192 individuals aged 70–79 years, found 13% had minor abnormalities and 23% major abnormalities. The different prevalences can be explained by age differences, since the present study assessed individuals aged 18–59, with a mean age of 40.4 years.
Women presented a higher prevalence of minor abnormalities, while men had a higher prevalence of major abnormalities. A study of adult outpatients in basic health care units in São Paulo, Brazil, also found a higher proportion of ECG changes among men.21
Smokers and former smokers showed a positive correlation with the presence of ECG abnormalities, as demonstrated in other studies.10,22,23 Oliveira et al. showed that adults aged 45 or under who smoked more than 25 cigarettes/day had a higher risk of myocardial infarction than those who had never smoked.24
In our study 37.7% of the population were hypertensive, while other Brazilian studies have reported prevalences between 20% and 45%.25–28 Hypertension is the risk factor most commonly associated with ECG alterations, mainly ST-T abnormalities.8,9 Greenland et al. showed that the risk of CAD rises from 38% to 67% at five years if the abnormalities persist.9
Only 5% of our study population were in the intermediate or high risk groups according to their Framingham score, and 38.9% of these had minor or major ECG abnormalities. A US study found ECG abnormalities in 54.7% of patients with high Framingham risk scores, which demonstrates that the score is a good predictor of cardiovascular risk in adults.8
Among diabetic individuals in our study, 31.8% had major or minor ECG abnormalities. Brollo et al. assessed 1042 Japanese-Brazilians and found no statistically significant difference in infarction scar area on ECG between diabetic and non-diabetic individuals. However, among those born in Brazil there was a tendency for ECG abnormalities to be found and infarction scars were present in 7.5% of those with diabetes, a finding that corroborates the results of the study.29
In the present study there was an association between alcohol consumption and ECG abnormalities, although other studies have found no such association.7,8,10 This discrepancy may be due to the difficulty in quantifying alcohol consumption. We used the CAGE questionnaire, which is a practical and validated method of screening for alcohol abuse in population studies, but its simplicity means it is unsuitable for assessing the degree of alcoholism.15
There was no association in our study between dyslipidemia and ECG abnormalities, although this has been demonstrated in other studies in various countries.8,10,30 A US study reported that 25.7% of individuals with ECG alterations and 24.7% of those with no alterations had high LDL-C, with no statistically significant difference.31 However, Denes et al. found a correlation with ECG abnormalities in women treated for dyslipidemia.10
One limitation of the study is that the sample population was not designed to enable analysis of subgroups, which would have allowed assessment of risk factors for CAD and specific ECG abnormalities. Furthermore, we have compared our results with studies that used different methods for interpreting and classifying ECGs; for example, in one US study ECG abnormalities were classified according to the Minnesota code.8,32 Finally, the records were analyzed by a single cardiologist, and there was therefore no assessment of intra- or interobserver agreement. Previous studies have shown variations in interpretation between individuals, which may affect the accuracy of ECG reports.33
Nevertheless, there are few Brazilian studies on the prevalence of ECG abnormalities in the general population, and the study thus makes an important contribution to public health; the ECG is a simple and widely available exam and is extremely valuable in screening for cardiac abnormalities, thus enabling early detection and intervention to prevent a fatal outcome.
ConclusionsOf the 361 adults studied, 61 (16.9%) had minor and 12 (3.3%) had major ECG changes.
The results showed that female gender, smoking, alcohol consumption, hypertension, diabetes and intermediate or high Framingham risk score were positively associated with ECG abnormalities, and some of these factors are modifiable.
The safety, low cost and wide availability of electrocardiography makes it useful for predicting cardiovascular risk in the general population.
Ethical responsibilitiesProtection of people and animalsThe authors state that the procedures followed were in accordance with regulations established by the heads of the Clinical and Research Ethics Commission and according to the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare having received written consent from patients and/or subjects mentioned in the article. The corresponding author must be in possession of this document.
FinancingThis study was funded by the Foundation for Research and Innovation of the State of Santa Catarina (FAPESC).
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank FAPESC for making this study possible, as well as the Santa Catarina Laboratory and the Center for Clinical Research of Hospital Nossa Senhora da Conceição.
Please cite this article as: Sebold FJG, Schuelter-Trevisol F, Nakashima L, Possamai Della Júnior A, Pereira MR, Trevisol DJ. Alterações eletrocardiográficas na população adulta de cidade do sul do Brasil: estudo populacional. Rev Port Cardiol. 2015;34:745–751.