A 70-year-old female with hypertension and symptomatic persistent atrial fibrillation (PersAF), of >3 months in duration and a CHA2DS2-VASc score of four, with early recurrence after external direct current (DC) cardioversion, underwent a successfully combined cryoballoon-based pulmonary vein isolation (PVI) plus left atrial appendage (LAA) isolation.
She had had a history of previous recurrent palpitations of short duration (<6 hours) since the previous year. At that time, the transthoracic echocardiogram (TTE) showed moderate dilation of the left atrium (LA), and a left ventricle ejection fraction (LVEF) >50%, without valvular abnormalities.
She presented at our department after four months of PersAF, showing fatigue and experiencing daily palpitations despite medication with edoxaban 60 mg, bisoprolol 5 mg, amiodarone 200 mg and candesartan 32 mg. The TTE showed marked LA dilation (52 ml/m2) and a LVEF of 35% and global hypokinesis. DC cardioversion was performed, but atrial fibrillation reappeared within one week. The patient was then scheduled for catheter ablation.
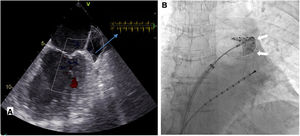
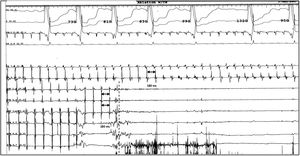
The cardiac computed tomography provided information for the anatomical mapping of the four pulmonary veins (PV) and excluded intracardiac thrombus. Immediate preprocedural transesophageal echocardiography found low velocity flow within the LAA, and LAA smoke, without thrombus formation (Figure 1A). DC cardioversion was attempted in the laboratory before PVI, without conversion to sinus rhythm (SR). PVI was then performed using a cryoballoon catheter (Arctic Front Advance; Medtronic) and a dedicated inner-lumen mapping catheter (Achieve Advance 2; Medtronic). During the procedure, an activated clotting time level around >300 s was reached following heparin administration. Elimination of all PV potentials was obtained (240 s per vein; ranging from -43°C (right inferior PV) to -52°C (left superior PV). Due to three failed DC cardioversion attempts after PVI, and evidence of a short cycle length on the LAA electrograms (180 ms), LAA was targeted and electrical isolation obtained with a 180s cryo-application (time-to-isolation: 90 seconds; -48°C) (Figure 1B and Figure 2). After LAA isolation, 100 j successfully converted PersAF into SR. PVI and LAA isolation were confirmed by entrance-and exit-block. The procedure time was 75 minutes, with 13 minutes (434 μGy) of fluoroscopy.
A. Transesophageal echocardiography imaging of the left atrial appendage in atrial fibrillation before ablation. Blood flow velocities (on the right top) showed low peak emptying velocities (<40 cm/s). B. Fluoroscopic image showing contrast injection with complete occlusion of the left atrial appendage (white arrows) by the inflated cryoballoon. Advance Achieve 2 circular catheter is placed inside the left atrial appendage (left anterior oblique view).
Complete disappearance of left atrial appendage signals during cryoballoon single shot isolation of left atrial appendage recorded by inner lumen circular mapping catheter.
CS: coronary sinus electrograms (from distal to proximal poles); ACH: left atrial appendage electrograms (from distal do proximal poles). Artifacts are due to freezing of ACH 6.7 poles during cryoenergy application.
At the 16 week follow-up, the patient remained asymptomatic, in stable SR, under edoxaban 60 mg, low amiodarone dosage, bisoprolol and candesartan. The seven-day external event-recorder showed SR, with frequent isolated supraventricular ectopic beats, without AF. LVEF improved to 50%, with moderate LA dilation (41 ml/m2), without right atrial dilation.
This case report is in line with recent literature,1–3 suggesting that electrical LAA isolation in addition to PVI can increase clinical success of PersAF ablation, and shows, as demonstrated by other authors,4 that single-shot cryoballoon application seems to be feasible and safe to obtain LAA isolation, although there is a strong recommendation to maintain lifelong oral anticoagulation therapy. Whether this novel purposed approach plays a role in the efficacy of PersAF ablation must be determined in future studies.
Conflicts of interestThe authors have no conflicts of interest to declare.