A 55-year-old man presented to our outpatient clinic reporting a six-month history of exertional dyspnea and intermittent atypical chest pain. His medical history included essential hypertension. The baseline electrocardiogram and echocardiogram were normal. The patient underwent treadmill exercise stress testing under the Bruce protocol. During stage 3, the patient developed 1.5-mm horizontal ST depression in V3-V6 and the inferior leads. The test was interrupted at 9 min due to fatigue, with no chest pain.
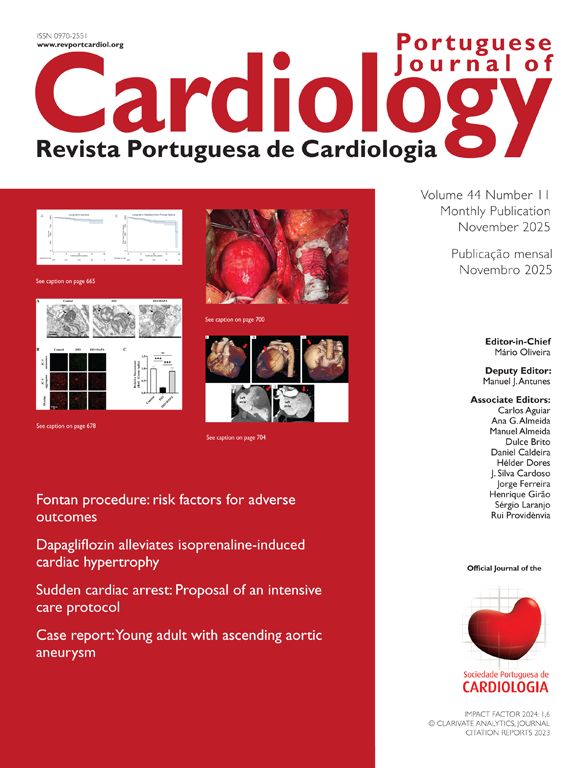
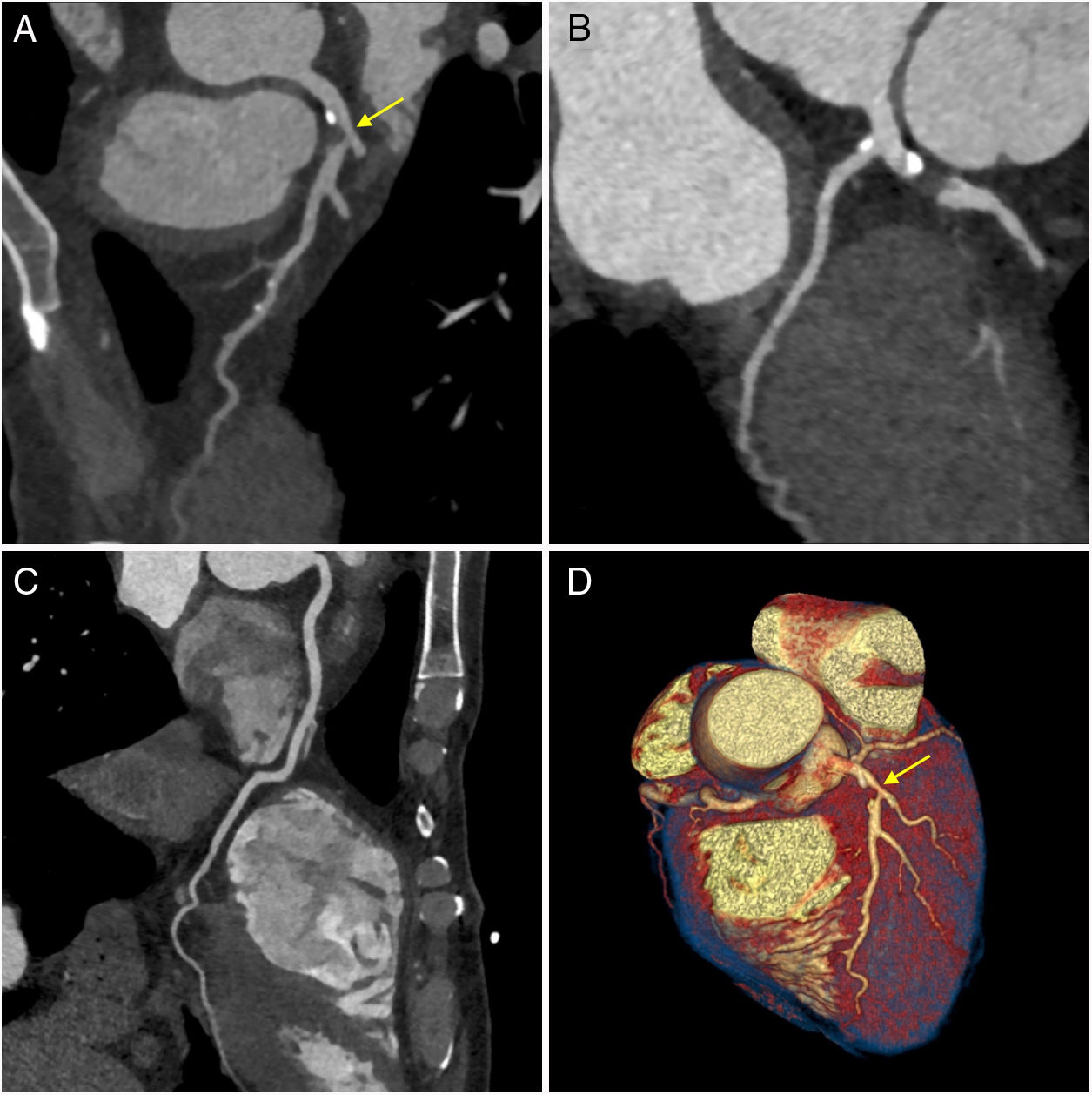
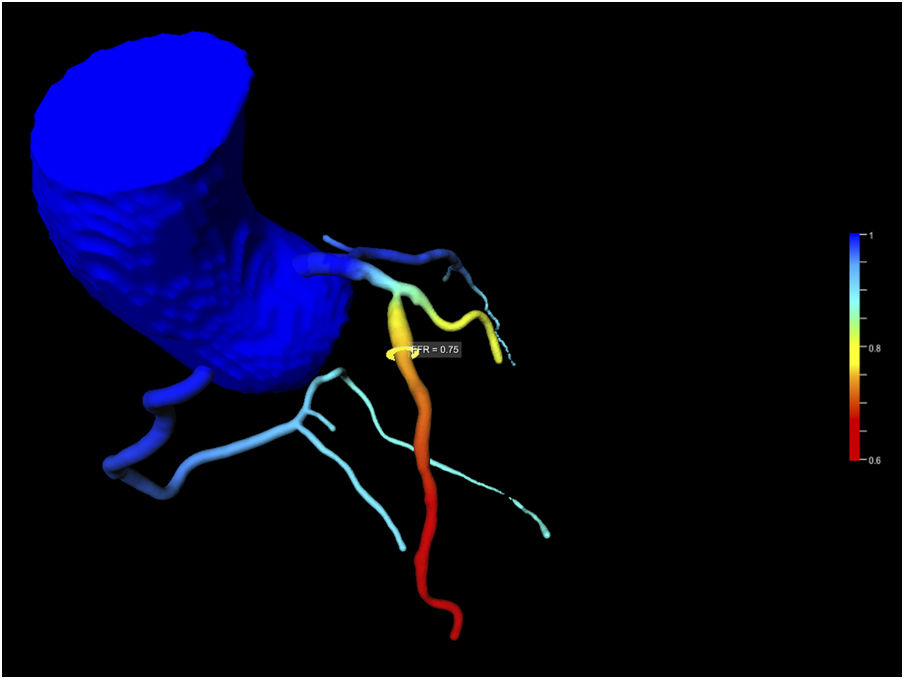
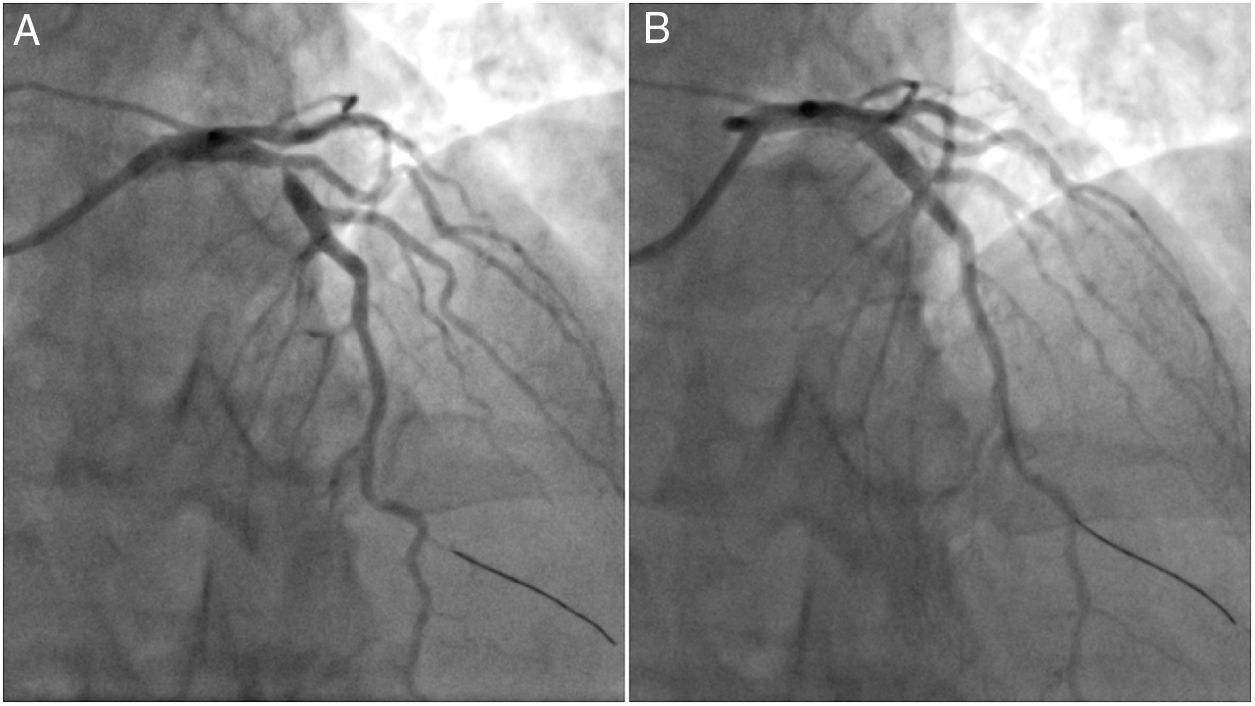
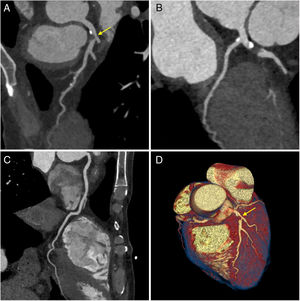
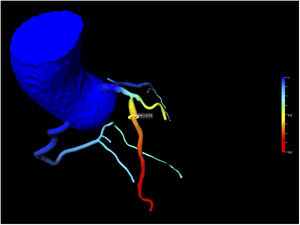
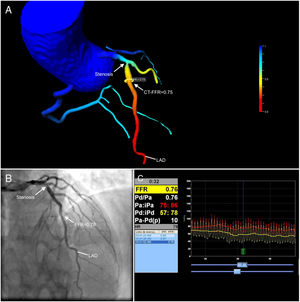
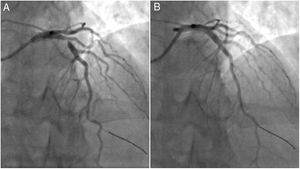
Due to intermediate risk findings on the treadmill test, coronary computed tomography angiography (CCTA) was requested for further assessment. The coronary calcium score was 105.2 Agatston units and an intermediate stenosis was identified in the proximal left anterior descending artery (LAD) due to non-calcified plaque (Figure 1A and D, arrow). Because the physiologic significance of the lesion was unclear, computed tomography-derived fractional flow reserve (CT-FFR) was determined using a workstation-based software prototype (cFFR, Siemens AG Healthcare, Forchheim, Germany). The value of CT-FFR just beyond the proximal LAD stenosis was 0.75 (Figure 2). The patient was referred for invasive coronary angiography (ICA) which confirmed a 75% stenosis in the proximal LAD (Figure 3B and Supplementary Video S1). Invasive FFR assessed in the LAD showed a similar result (0.76) to that observed on CCTA (Figures 3A and 3C). The patient successfully underwent percutaneous coronary intervention with a drug-eluting stent (Figure 4) and was asymptomatic after the procedure. This case illustrates the value of CT-FFR as a gatekeeper prior to ICA, to appropriately select patients and vessels for revascularization.
Coronary computed tomography angiography images. Curved multiplanar reformats of the left anterior descending artery (LAD) (A), left circumflex artery (B) and right coronary artery (C); three-dimensional volume rendering image of the heart (D). Note the presence of significant stenosis in the proximal LAD due to non-calcified plaque (arrows).
Correlation between invasive coronary angiography and coronary computed tomography (CT) angiography. (A) CT-derived fractional flow reserve (FFR) imaging showing an intermediate stenosis in the proximal left anterior descending artery (LAD) with a computed FFR of 0.75; (B) invasive coronary angiography confirming a 75% stenosis in the proximal LAD; (C) the measured value of invasive FFR was 0.76, which showed a good agreement with the CT-derived value (A).
The authors have no conflicts of interest to declare.