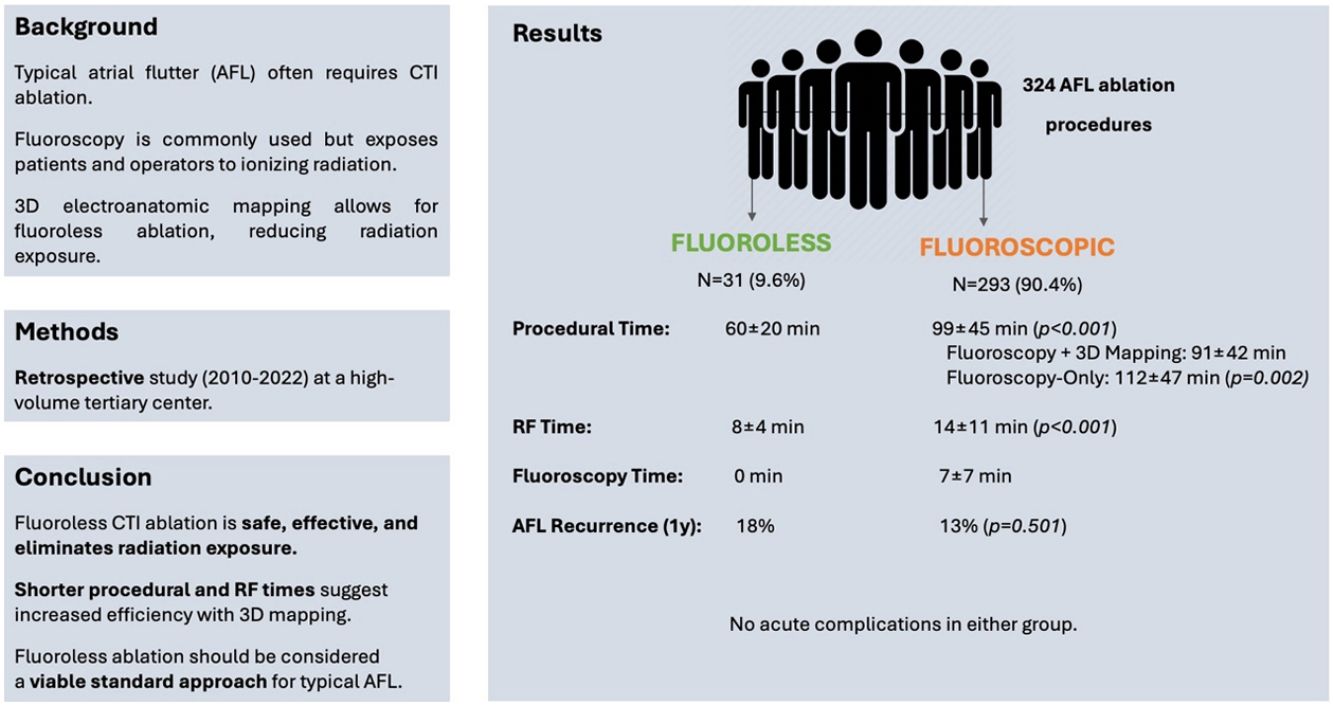
Cavotricuspid isthmus (CTI) ablation for typical atrial flutter (AFL) has improved in recent years, especially with three-dimensional (3D) electroanatomic mapping systems. These tools allow a better understanding of the arrhythmia with higher ablation success rates while reducing radiation exposure. However, most ablation procedures still require varying amounts of fluoroscopy. Our aim was to examine whether fluoroless CTI ablation is effective and safe in reducing AFL recurrence, compared with CTI ablation using fluoroscopy.
MethodsWe conducted a retrospective analysis of CTI ablations performed at a tertiary center between December 2010 and December 2022. Patients were divided into two groups: fluoroless and fluoroscopic, according to the use of radiation. Procedural duration, fluoroscopy time (FT), radiofrequency time (RF), acute complications and recurrence rates at one year were analyzed.
ResultsA total of 324 CTI ablations were performed. Mean age was 62.3±14.0 years, with 78.1% male patients. The FT was zero in the fluoroless group (n=31), and 7.0±7.0 minutes in the fluoroscopic group (n=293) (p<0.001). There was no statistically significant difference between the two groups, regarding AFL recurrence at one year. RF was shorter in the fluoroless group (8±4 vs. 14±11 minutes, p<0.001). Total time procedure duration was shorter in the fluoroless group (60±20 minutes vs. 99±45 minutes, p<0.001). There were no acute complications.
ConclusionFluoroless CTI ablation, avoiding any radiation exposure to the patient and operator, can be performed in patients with typical AFL, without compromising duration, safety or efficacy of the procedure.
A ablação do istmo cavotricúspide (ICT) no flutter auricular típico (FLA) melhorou nos últimos anos, especialmente com o uso de sistemas de mapeamento eletroanatomico tridimensional (3D). Estas ferramentas contribuíram para reduzir a exposição à radiação, mas a maioria dos procedimentos de ablação ainda requer alguma quantidade de fluoroscopia. O nosso objetivo passou por avaliar se a ablação do ICT sem fluoroscopia é eficaz e segura na redução da recorrência de FLA, em comparação com a ablação do ICT com utilização fluoroscopia.
MétodosAnálise retrospetiva de ablações do ICT realizadas num centro terciário entre dezembro de 2010 e dezembro de 2022. Os doentes foram divididos em dois grupos: sem fluoroscopia e com fluoroscopia, conforme o uso de radiação. Foram analisados o tempo total do procedimento, tempo de fluoroscopia (TF), tempo de radiofrequência (RF), complicações agudas e taxas de recorrência após um ano.
ResultadosUm total de 324 ablações de ICT foram realizadas. A idade média foi de 62,3 ± 14,0 anos, com 78,1% de doentes do sexo masculino. O TF foi zero no grupo sem fluoroscopia (n=31) e 7,0±7,0 minutos no grupo com fluoroscopia (n=293) (p<0,001). Não houve diferença estatisticamente significativa entre os dois grupos em relação à recorrência de FLA após um ano. O RF foi menor no grupo sem fluoroscopia (8±4 versus 14±11 minutos, p<0,001). A duração total do procedimento também foi menor no grupo sem fluoroscopia (60±20 minutos versus 99±45 minutos, p<0,001). Não foram observadas complicações agudas.
ConclusãoA ablação do ICT sem fluoroscopia pode ser realizada em doentes com FLA típico, sem comprometer a duração, segurança ou eficácia do procedimento.
Typical atrial flutter (AFL) is a common macro-reentrant arrhythmia that often requires intervention to treat and improve symptoms. Cavotricuspid isthmus (CTI) ablation has proven to be an effective treatment for typical AFL.1,2
Over the past decade, advancements in three-dimensional (3D) electroanatomic mapping systems have significantly improved the success and safety of CTI ablation. Despite these advances, most ablation procedures still rely on varying amounts of fluoroscopy, which is a source of ionizing radiation with risks for both patients and operators.3–5
There is growing interest in fluoroless ablation techniques that eliminate radiation exposure. Previous studies have suggested that fluoroless ablations using 3D mapping systems can be performed effectively for various arrythmias,6–8 but comprehensive data comparing the outcomes of fluoroless versus fluoroscopic CTI ablation for typical AFL are limited.
ObjectivesThis study aimed to evaluate whether fluoroless CTI ablation could achieve comparable success rates in AFL control while maintaining safety, when compared with a fluoroscopy-guided ablation. By analyzing procedural outcomes and AFL recurrence rates at one year, we aimed to determine the viability of fluoroless ablation as a standard treatment option.
MethodsStudy population and designThe present study was a retrospective analysis conducted at a single high-volume tertiary medical center by experienced operators, evaluating patients who underwent CTI ablation for documented typical atrial AFL between December 2010 and December 2022. Patients were categorized into two distinct groups based on fluoroscopy use. The fluoroscopic group, which received ablation guided by fluoroscopy with or without the use of a 3D electroanatomic mapping system, and the fluoroless group, which underwent CTI ablation without the use of fluoroscopy, based solely on the analysis of electroanatomic signs and a 3D electroanatomic mapping system. An additional analysis was conducted between fluoroscopic and fluoroless procedures, adjusting for the presence of 3D mapping.
Patients >18 years of age with documented CTI-dependent atrial flutter were included. Patients <18 years old, pregnant women and patients with concomitant arrhythmias submitted to ablation in the same procedure were excluded.
Data collected included clinical and procedural variables. The total duration of the procedure was measured from the insertion of catheters to the removal of all equipment. Fluoroscopy time (FT) was recorded as the total time during which fluoroscopy was actively used during the procedure. The radiofrequency time (RF), representing the duration of energy delivery to achieve CTI ablation, was also documented.
In addition to procedural variables, we analyzed acute complications, defined as any adverse events occurring during or immediately after the procedure. Furthermore, patients were followed for one-year post-procedure to assess the recurrence of AFL, which was defined as the return of typical AFL symptoms confirmed by 12-lead electrocardiogram (ECG) or 24-hour Holter monitoring.
Procedural descriptionIn the fluoroless group, CTI ablation was performed exclusively using 3D electroanatomic mapping systems (CARTO™, Biosense Webster, Inc. or EnSite Precision™, Abbott, Inc). The choice between mapping systems was determined by operator preference and equipment availability at the time of the procedure. Catheters were advanced into the heart and visualized by the 3D mapping system with localization confirmed by the interpretation of local electrograms, without the need for fluoroscopy. A Decapolar catheter was positioned inside the coronary sinus, and an ablation catheter was used to deliver radiofrequency to the CTI. In the fluoroscopy group, the use of fluoroscopy to guide catheter insertion and localization was allowed, with or without concomitant 3D mapping system use. CTI ablation was performed with 35–40 W, and acute success was defined as a bidirectional CTI block confirmed by a differential pacing maneuver.
Follow-upThe patients underwent follow-up with a cardiology physician at the hospital outpatient clinic from post-procedure to at least one year after the procedure. Twelve-lead ECG was performed in all patients at every office visit, and a 24-hour Holter monitoring was obtained in the first and 12th months to assess arrhythmia recurrence.
Statistical analysisStatistical analysis was performed to compare outcomes between the fluoroless and fluoroscopic groups. Continuous variables, such as age, procedural duration, and RF time, were expressed as mean±standard deviation (SD) and compared using independent t-tests. Categorical variables, including sex, presence of comorbidities, and recurrence rates, were compared using chi-square tests or Fisher's exact tests where appropriate. Odds ratios (OR) with 95% confidence intervals (CI) were calculated to evaluate the association between fluoroscopy use and AFL recurrence at one year. P-value <0.05 was considered statistically significant.
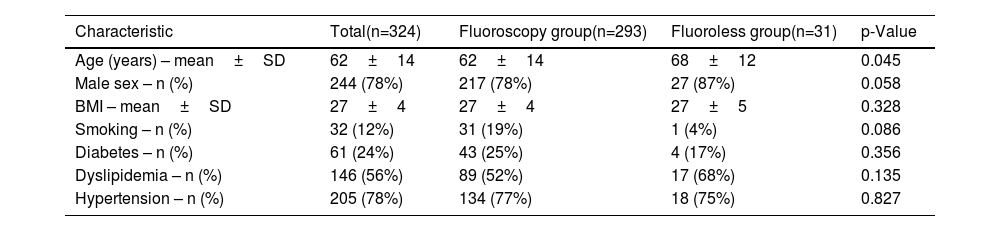
ResultsA total of 324 CTI ablation procedures were included in the analysis, with 31 patients (9.6%) undergoing fluoroless ablation and 293 patients (90.4%) receiving ablation with fluoroscopic guidance (Table 1). The mean age was 62.3±14.0 years, with a predominance of male patients (78.1%). A statistically significant difference in age was observed between the two groups; patients in the fluoroless group were older, with a mean age of 68±12 years compared to 62±14 years in the fluoroscopic group (p=0.045). There was no statistically significant difference in the proportion of male patients between the groups, with 93% in the fluoroless group and 78% in the fluoroscopic group (p=0.058).
Baseline characteristics of the study population.
| Characteristic | Total(n=324) | Fluoroscopy group(n=293) | Fluoroless group(n=31) | p-Value |
|---|---|---|---|---|
| Age (years) – mean±SD | 62±14 | 62±14 | 68±12 | 0.045 |
| Male sex – n (%) | 244 (78%) | 217 (78%) | 27 (87%) | 0.058 |
| BMI – mean±SD | 27±4 | 27±4 | 27±5 | 0.328 |
| Smoking – n (%) | 32 (12%) | 31 (19%) | 1 (4%) | 0.086 |
| Diabetes – n (%) | 61 (24%) | 43 (25%) | 4 (17%) | 0.356 |
| Dyslipidemia – n (%) | 146 (56%) | 89 (52%) | 17 (68%) | 0.135 |
| Hypertension – n (%) | 205 (78%) | 134 (77%) | 18 (75%) | 0.827 |
BMI: body mass index; SD: standard deviation.
Body mass index (BMI) was similar between the two groups, with a mean BMI of 27± 4 kg/m2 in the fluoroscopic group and 27±5 kg/m2 in the fluoroless group (p=0.328). Risk factors, including smoking, diabetes, dyslipidemia, and hypertension, were also compared. While the incidence of smoking was lower in the fluoroless group (4%) compared to the fluoroscopic group (19%), this difference did not reach statistical significance (p=0.086). Similarly, there were no statistically significant differences in the prevalence of diabetes (17% vs. 25%, p=0.356), dyslipidemia (68% vs. 52%, p=0.135), or hypertension (75% vs. 77%, p=0.827) between the two groups.
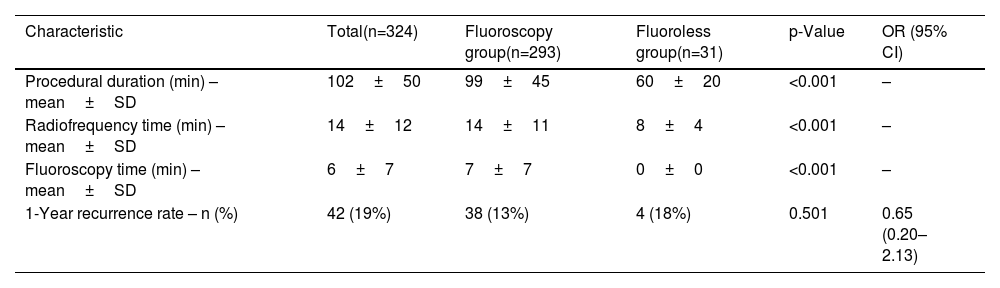
Regarding procedural outcomes (Table 2), the total duration of the procedure was significantly shorter in the fluoroless group, with a mean time of 60±20 minutes compared to 99±45 minutes in the fluoroscopic group (p<0.001).
Procedural characteristics and one-year recurrence rate.
| Characteristic | Total(n=324) | Fluoroscopy group(n=293) | Fluoroless group(n=31) | p-Value | OR (95% CI) |
|---|---|---|---|---|---|
| Procedural duration (min) – mean±SD | 102±50 | 99±45 | 60±20 | <0.001 | – |
| Radiofrequency time (min) – mean±SD | 14±12 | 14±11 | 8±4 | <0.001 | – |
| Fluoroscopy time (min) – mean±SD | 6±7 | 7±7 | 0±0 | <0.001 | – |
| 1-Year recurrence rate – n (%) | 42 (19%) | 38 (13%) | 4 (18%) | 0.501 | 0.65 (0.20–2.13) |
CI: confidence interval; OR: odds ratio; SD: standard deviation.
The mean radiofrequency time was significantly shorter in the fluoroless group, 8±4 minutes compared to 14±11 minutes in the fluoroscopic group (p<0.001). FT was zero minutes in the fluoroless group, whereas the fluoroscopic group had a mean FT of 7±7 minutes.
At one-year follow-up, AFL recurrence was observed in 18% of patients in the fluoroless group and 13% in the fluoroscopic group, without a statistically significant difference (p=0.501). The odds ratio for AFL recurrence in the fluoroless group compared to the fluoroscopic group was 0.65, with a 95% confidence interval of 0.20–2.13 (p=0.501).
An additional analysis was performed adjusting for the use of 3D electroanatomic mapping systems. Out of all CTI ablation procedures, 209 (64.5%) were performed with the use of a 3D electroanatomic mapping system. This included all 31 fluoroless cases and 178 fluoroscopic procedures. The remaining 115 procedures (35.5%) were fluoroscopic ablations without 3D mapping. Procedures using 3D systems demonstrated significantly shorter procedural durations compared to those without 3D mapping (84±43 minutes vs. 112±47 minutes, p<0.001). Similarly, RF time was significantly lower in the 3D group (11±9 minutes vs. 17±12 minutes, p<0.001). AFL recurrence at one year was 14% in the 3D group versus 12% in the non-3D group (p=0.663), showing no statistically significant difference in arrhythmia recurrence between groups.
No acute complications were reported.
DiscussionIn this study, we evaluated the efficacy and safety of fluoroless CTI ablation for the treatment of typical AFL compared with a fluoroscopy-guided approach. Our findings demonstrate that fluoroless CTI ablation, performed using advanced 3D electroanatomic mapping systems can achieve outcomes comparable to fluoroscopic ablation, while eliminating radiation exposure to both patients and operators.
The primary outcome of our study was the recurrence rate of AFL at one year. We found no statistically significant difference in recurrence rates between the fluoroless group (18%) and the fluoroscopic group (13%), suggesting that the absence of fluoroscopy does not compromise the long-term effectiveness of the ablation. This result is consistent with previous studies that have shown the feasibility of fluoroless ablation in various arrhythmias, including atrial fibrillation, atrioventricular node re-entry tachycardia and typical AFL.6–10
An interesting finding of our study is the significant reduction in total procedural duration in the fluoroless group. Since the earliest procedures date back to 2010, earlier fluoroscopic ablations may have relied more on traditional fluoroscopy, while more recent procedures, regardless of fluoroscopy use, likely benefited from advancements in 3D electroanatomic mapping systems. To further investigate this, we performed a subgroup analysis comparing fluoroless and fluoroscopic procedures with and without 3D mapping. The results indicate that procedures utilizing 3D mapping had significantly shorter procedural times compared to cases without 3D, supporting the hypothesis that mapping system adoption played a role in procedural efficiency.11–13
Regarding safety, no acute complications were observed in either the fluoroless or fluoroscopic groups, indicating that fluoroless CTI ablation is a safe alternative to fluoroscopic methods. On the other hand, the complete elimination of fluoroscopy not only removes the risks associated with radiation exposure to the patient but also enhances safety for the operator by reducing cumulative radiation dose.14–16
Several limitations should be acknowledged. First, the retrospective nature of the study introduces the possibility of selection bias, as the choice of fluoroless versus fluoroscopic ablation was not randomized but rather determined by operator preference and clinical circumstances. Additionally, the number of patients in the fluoroless group was relatively small, which may limit the generalizability of our findings. Further prospective studies with larger sample sizes and randomized designs are needed to confirm these results and to establish standardized protocols for fluoroless CTI ablation.
ConclusionIn conclusion, our study demonstrates that fluoroless CTI ablation using 3D electroanatomic mapping systems is a safe and effective alternative to fluoroscopy-guided ablation for typical AFL. In our cohort, this approach not only eliminated radiation exposure but also reduced procedural duration without compromising the efficacy of the procedure.
FundingThe authors have not declared a specific grant for this research from any funding agency in the public commercial or not-for-profit sectors.
Conflict of interestsThe authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.