Clinical use of chronotropic response has been limited due to lack of consensus on the appropriate formula for chronotropic index (Ci) calculation and the definition of chronotropic incompetence.
ObjectivesTo assess the effects of cardiac rehabilitation programs (CRP) on Ci, irrespective of betablockers (BB) use and dosage. Assess the relative contribution of change in Ci on improvement in functional capacity.
MethodsRetrospective analysis of a sample of patients admitted to a CRP after acute coronary syndrome, with at least 12 months of follow-up. Ci was calculated using the conventional (CCi) and the Brawner formula (BCi) for age-predicted maximum heart rate. Ci and functional capacity were estimated at three time points: T1 and T2, before and at the end of the CRP, and T3, at 12 months. The sample was categorized according to BB dosage modification between T1 and T3: G1 – reduced; G2 – no change; G3 – increased.
ResultsIn G1, CCi increased from 63.5% in T1 to 77.9% in T3; in G2, from 67.3% to 77.9%; in G3, from 71.2% to 75.4%. In G1, BCi increased from 110.4% to 140.0%; in G2, from 122.8% to 140.1%; in G3, from 133.3% to 139.2%. An average increase in 1.0% in CCi was associated with an average increase in functional capacity of 0.37 METS.
ConclusionsChronotropic index significantly improves with CRP, irrespective of BB dose changes. CCi is more closely related with improvement in functional capacity than BCi. Improvement of Ci is an important predictor of functional capacity and prognosis in cardiovascular disease patients.
A aplicabilidade clínica da resposta cronotrópica é limitada pela ausência de consenso na fórmula para o cálculo do índice cronotrópico (IC) e na definição de incompetência cronotrópica.
ObjetivosAvaliação do efeito dos programas de reabilitação cardíaca (PRC) no IC, independentemente da utilização de β-bloqueadores (BB) e respetiva dosagem. Avaliação da contribuição relativa da modificação do IC na melhoria funcional.
MétodosAnálise retrospetiva de uma amostra de doentes admitidos num PRC após uma síndrome coronária aguda, com pelo menos 12 meses de seguimento. O IC [estimado pela fórmula convencional (ICC) e de Brawner (ICB) para a frequência cardíaca máxima prevista para a idade] e a capacidade funcional foram avaliados em três momentos: T1 e T2, antes e após o término do PRC, e T3, aos 12 meses. A amostra foi categorizada pela modificação da dose de BB entre T1 e T3: G1 – reduzida; G2 – mantida; G3 – aumentada.
ResultadosNo G1, o ICC aumentou de 63,5% em T1 para 77,9% em T3; no G2, de 67,3% para 77,9%; no G3, de 71,2% para 75,4%. No G1, o ICB aumentou de 110,4% para 140,0%; no G2, de 122,8% para 140,1%; no G3, de 133,3% para 139,2%. O aumento médio de 1,0% no ICC associou-se ao aumento médio de 0,37 METS na capacidade funcional.
ConclusõesO PRC melhora o IC, independentemente das alterações de dose dos BB. ICC correlaciona-se mais com a melhoria funcional do que o ICB. O IC é preditor da capacidade funcional e do prognóstico na doença cardiovascular.
Chronotropic response is the ability to adapt heart rate (HR) to the level of activity or demand1 and is frequently impaired in patients with cardiovascular (CV) disease.2 This physiologic reflex is a strong and independent predictor of functional capacity and CV morbidity and mortality.1,3 It is usually represented by the chronotropic index (Ci), defined as the fraction of the age-predicted maximal HR (APMHR) or, more commonly, of the age-predicted HR reserve achieved at maximal effort.4 Wider use of Ci has been limited by the lack of consensus on the appropriate definition and cut-off points to establish chronotropic incompetence (CI), with most studies suggesting failure to attain a Ci ≥80%, measured during a graded exercise test, as the primary criterion for CI,1 although other thresholds have been used (either 85% or 70%, for example).5
Chronotropic index produces exercise intolerance and, although the increase in HR is the strongest contributor to aerobic performance,6 other factors should be considered, such as failure to achieve maximal HR, inadequate submaximal HR, HR instability during exertion and the rate of HR recovery after exertion, which is also an important indicator of risk of all-cause mortality.1,7,8 HR responses at rest, during and after exercise are thus strongly associated with increased risk of adverse CV outcomes.2,9 Moreover, confounding effects of gender, age and medication (particularly beta blockers (BB)) in HR should be considered when diagnosing CI, as these factors influence the maximal HR attained during exertion.
The conventional equation to predict APMHR (220 – age in years), which is based on the physiological decrease in maximal HR with aging, was established in a cohort of healthy young men, shows a large variability between subjects and may not be adequate in patients with coronary artery disease (CAD), particularly those taking BB, with standard deviations of ±40 beats per minute (bpm) in some cases.10,11 In fact, maximal HR is expected to be lower in patients on BB therapy irrespective of age, suggesting the need to use alternative equations and different CI thresholds in those taking BB. Brawner proposed using APMHR (164 – 0.7(age in years)) and the ≥80% threshold to define CI, while others suggest using the conventional formula with a lower threshold of Ci ≤62% for diagnosing CI.11,12 However, having multiple criteria and a lack of standardization can dampen practicality for Ci clinical use. This indicator is, therefore, frequently overlooked, particularly in the setting of cardiac rehabilitation programs (CRP), where it can stand as a useful tool to assess the outcomes after an acute coronary syndrome (ACS). CRP programs tend to enhance chronotropic response and when CI is correctly managed, functional capacity and quality of life of the individual are strongly improved.1
ObjectivesThe aim of this study was to assess the short and long-term effects of an exercise training program after an ACS on HR response during exercise and, mostly, its effect on the Ci, irrespective of BB use and dose. In addition, we assessed the relative contribution of change in Ci with CRP for improvement of functional capacity.
MethodsSubjectsData was obtained on 543 patients, selected through a retrospective analysis of a consecutive sample of patients admitted to an ambulatory CRP, after ACS, between 2009 and 2017, and with at least 12 months of follow-up. Clinical information was obtained from electronic clinical records and office visits at three different times: T1, before the CRP; T2, at the end of the CRP; T3, 12 months after the event. There was no patient allocation by the investigators for any intervention. BB dosage was converted into equivalents and the sample was categorized according to the dosage modification from T1 to T3 in: Group 1 (G1) – dose reduced –, Group 2 (G2) – no change – and Group 3 (G3) – dose increased. The investigators had no specific intervention on BB dosage modification; this was determined by each patient's attending cardiologist.
Exercise testingSymptom-limited and electrocardiographic monitored exercise testing on a treadmill following the Bruce protocol was performed at the Cardiology Department at T1, T2 and T3. Among other parameters, the records included resting HR and maximal attained HR. Ci and functional capacity were estimated at each timepoint. For functional capacity, metabolic equivalents (METS) achieved in exercise testing were used.
Cardiac rehabilitation programThe cardiac rehabilitation program consisted of two 60-minute weekly exercise training sessions comprising 40 minutes of aerobic training (at an intensity between 60% and 80% of the HR reserve, achieved at baseline exercise testing, with a perceived effort score of 11 to 13 in the Borg Scale of Perceived Exertion) and muscular strengthening in the remaining time (targeting five muscle, 15 repetitions per exercise corresponding to an estimated load of 60% 1-RM). The number of training sessions ranged from eight to 24, considering ACS severity and patient preference. Additionally, every patient received nutritional counseling and cognitive-behavioral intervention.
Definition of chronotropic index and chronotropic incompetenceChronotropic index was calculated based on APMHR, the latter being determined using the CCi and the BCi equations at each time point (T1, T2 and T3). Patients who failed to achieve a Ci of 80%, with either equation, were classified as having CI. Patients with a Ci of 80% or higher were classified as having chronotropic competence. For CCi, an additional analysis was performed considering the threshold of 62% for CI.
Statistical analysisWe used IBM SPSS Statistics® to perform our analysis. Standard descriptive measures, including mean and SD for normally distributed continuous variables and proportion (expressed as %) for categorical variables, were used. For comparison between groups, we used a repeated measure analysis of variance, considering a significance p<0.05. Functional capacity was determined by metabolic equivalents and the change ([METS(T3-T1)]/T1*100) correlated to the CCi and BCi using a scatter plot. Linear regression analysis of the CCi was performed using functional capacity change as dependent variable, considering gender, age, BB medication and BB dosage modification.
ResultsPopulation characteristicsOf the 543 patients included, 85.1% were men and the mean age (standard deviation (SD)) was 54.7 (10.1) years old. All the patients were referred after an ACS, 468 (86.2%) underwent percutaneous coronary intervention, 11 (2.0%) coronary bypass and 64 (11.8%) had only medical treatment.
There was a total of 279 (51.4%) ST-segment elevation myocardial infarctions (STEMI) and 264 (48.6%) non-ST-segment elevation ACS [215 (38.7%) non-STEMI and 49 (8.7%) unstable anginas]. The majority of patients was in class I of the New York Heart Association (NYHA) functional classification, with only 60 (11.0%) scoring as NYAH class II. Left ventricle ejection fraction (LVEF) had a mean (SD) value of 52.7 (11.7) % at T1. At T3, there was information on the LVEF from 483 patients, with a mean (SD) value of 60.4 (9.1) %. The additional demographic and clinical characteristics of the population at baseline are presented in Table 1. CRP had a mean (SD) of 12.9 (4.4) sessions and 497 (91.5%) of the patients completed it; the remaining were lost to follow-up or had to interrupt the sessions because of intolerance or complications associated with the exercise.
Summary of demographic and clinical information of the population at baseline.
| Gender, male (%) | 85.1% | |
|---|---|---|
| Age in years, mean (SD) | 54.7 (10.1) | |
| Marital status | Single, n (%) | 31 (5.7%) |
| Married, n (%) | 423 (77.9%) | |
| Divorced, n (%) | 61 (11.2%) | |
| No information, n (%) | 28 (5,2%) | |
| Literacy in years of education, mean (SD) | 9.1 (4.8) | |
| Professional situation | Employed, n (%) | 291 (53.6%) |
| Unemployed, n (%) | 88 (16.2%) | |
| Retired, n (%) | 139 (25.6%) | |
| No information, n (%) | 25 (4,6%) | |
| Clinical background | CAD, n (%) | 51 (9.4%) |
| Dyslipidemia, n (%) | 336 (61.9%) | |
| Hypertension, n (%) | 235 (43.3%) | |
| DM, n (%) | 97 (17.9%) | |
| Weight in kg, mean (SD) | 77.0 (12.3) | |
| Abdominal perimeter in cm, mean (SD) | 96.4 (10.1) | |
| Actual or former smoker, n (%) | 416 (76.6%) | |
| COPD, n (%) | 6 (1.1%) | |
| Depression, n (%) | 28 (5.2%) | |
| Familial history of CVD, n (%) | 142 (26.2%) | |
| Pharmacological treatments | Beta-blocker, n (%) | 468 (86.2%) |
| ACE inhibitor, n (%) | 461 (84,9%) | |
| Aldosterone receptor antagonist, n (%) | 15 (2,8%) | |
| Nitrates, n (%) | 12 (2,2%) | |
| Calcium channel blocker, n (%) | 23 (4,2%) | |
| Beta2-Adrenoreceptor agonist, n (%) | 8 (1,5%) | |
| Exercise testing | Rest HR in bpm, mean (SD) | 73.8 (11.9) |
| Maximal attained HR in bpm, mean (SD) | 135.7 (18.6) | |
| Percentage of APMHR, mean (SD) | 83.6 (37.2) | |
| ACS type | NST ACS, n (%) | 264 (48.6%) |
| STEMI, n (%) | 279 (51.4%) | |
| Anterior, n (%) | 106 (38.0%*) | |
| Inferior, n (%) | 92 (33.0%*) | |
| Posterior-inferior, n (%) | 36 (12.9%*) | |
| Anterior-lateral, n (%) | 19 (6.8%*) | |
| Others, n (%) | 26 (9.3%*) | |
| LVEF per category | Normal or slightly reduced (≥40%), n (%) | 429 (79.0%) |
| Moderate to severely reduced (≤39%), n (%) | 94 (17.3%) | |
| No information, n (%) | 20 (3.7%) |
ACE, angiotensin converting enzyme; ACS, acute coronary syndrome; APMHR, age-predicted maximal heart rate; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; DM, diabetes mellitus; HR, heart rate; LVEF, left ventricle ejection fraction; NST, non-ST-segment elevation; STEMI, ST-segment elevation myocardial infarction.
*% relative to the total of STEMI ACS.
At baseline, 468 (86.2%) of patients were taking BBs, while at T3 there were 472 (87.0%). Considering BB therapy between T1 and T3, only 42 patients (7.7%) never took BB, 33 (6.1%) started BB, 29 (5.3%) suspended BB, 298 (54.9%) had no BB dose change, 43 (7.9%) reduced and 98 (18.0%) increased the BB dose. Accordingly, 72 (13.3%) of patients were included in G1, 340 (62.6%) in G2 and 131 (24.1%) in G3.
There were no significant differences between BB therapy groups at the different time points. At T1, in G1 there were 60 (83.3%) patients taking angiotensin converting enzyme (ACE) inhibitors, two (2.8%) taking aldosterone receptor antagonists (ARA), 2 (2.8%) taking calcium channel blockers (CCB), one (1.4%) taking nitrates and one (1.4%) taking beta2-adrenoreceptor agonists. At G2 and G3, there were, respectively, 293 (86.2%) and 108 (82.4%) patients taking ACE inhibitors, 10 (2.9%) and 3 (2.3%) taking ARA, 10 (2.9%) and one (0.8%) taking nitrates, 17 (5.0%) and 4 (1.3%) taking CCB and 6 (1.8%) and 1 (0.8%) taking beta2-adrenoreceptor agonists.
Chronotropic responseFor the entire sample we found that, at baseline exercise testing, HR increased from 73.8 (11.9) bpm, at rest, to a maximal HR of 135.7 (18.6) bpm. Considering BB therapy group, G1 showed an increase from a rest HR of 69.1 (10.8) bpm to a maximal HR of 130.3 (21.3) bpm. In G2, HR increased from 73.4 (11.9) bpm at rest to a maximal HR of 134.8 (17.8). Finally, in G3, HR increased from 77.1 (11.6) bpm to a maximal HR of 140.9 (17.8) bpm. Therefore, at baseline, there was a statistically significant difference between groups for resting and maximal HR values (p<0.05). After the CRP sessions, at T2, resting HR for the entire sample was 70.7 (12.3) bpm and increased to a maximal HR of 141.3 (18.0) bpm. Considering BB therapy group, G1 showed an increase from a rest HR of 67.9 (14.6) bpm to a maximal HR of 139.5 (20.8) bpm. In G2, HR increased from 69.8 (11.6) bpm at rest to a maximal HR of 140.9 (17.6) bpm and, in G3, from 74.4 (11.9) bpm to 143.3 (17.2) bpm.
When performing the exercise testing at T3, there was a resting HR of 72.4 (12.3) bpm and a maximal HR of 144.0 (17.7) bpm. In G1, resting HR was 71.8 (13.8) bpm and maximal HR was 144.9 (19.1) bpm. In G2, HR increased from 72.0 (11.8) bpm at rest to a maximal HR of 144.0 (17.6) bpm. Lastly, in G3, HR showed an increase from 73.8 (12.7) bpm to 143.4 (17.2) bpm, respectively. There were no significant differences between groups for resting or maximal HR (p>0.05).
Chronotropic indexConventional chronotropic index and BCi values for the entire sample and for each BB therapy group are presented in Tables 2 and 3, respectively. We found a similar significant change in both CCi, BCi and in % patients with CI after CRP in all BB therapy groups (CCi: within-group analysis: p<0.001; between-group analysis: p=0.57; BBi: within-group analysis: p<0.001; between-group analysis: p=0.14).
Chronotropic index values using conventional formula for APMHR.
| T1 | T2 | T3 | ||||
|---|---|---|---|---|---|---|
| CCi in %,mean (SD) | CCi <80%, n (%) | CCi in %,mean (SD) | CCi <80%, n (%) | CCi in %,mean (SD) | CCi <80%, n (%) | |
| Total | 67.7 (18.7) | 400 (73.7%) | 74.7 (18.2) | 307 (56.5%) | 77.3 (17.3) | 297 (54.7%) |
| G1 | 63.5 (20.3) | 60 (83.3%) | 73.4 (17.1) | 44 (61.1%) | 77.9 (18.8) | 36 (50.0%) |
| G2 | 67.3 (18.2) | 251 (73.8%) | 75.2 (17.1) | 186 (54.7%) | 77.9 (16.9) | 181 (53.2%) |
| G3 | 71.2 (18.8) | 89 (67.9%) | 74.3 (17.9) | 77 (58.8%) | 75.4 (17.4) | 80 (61.1%) |
APMHR, age-predicted maximal heart rate; CCi, conventional chronotropic index; G1, group 1; G2, group 2; G3, group 3.
Chronotropic index values using Brawner formula for APMHR.
| T1 | T2 | T3 | ||||
|---|---|---|---|---|---|---|
| BCi in %,mean (SD) | BCi <80%, n (%) | BCi in %,mean (SD) | BCi <80%, n (%) | BCi in %, mean (SD) | BCi <80%, n (%) | |
| Total | 123.7 (41.9) | 61 (11.2%) | 132.2 (39.1) | 29 (5.3%) | 139.9 (44.3) | 25 (4.6%) |
| G1 | 110.4 (39.3) | 14 (19.4%) | 128.5 (56.4) | 9 (12.5%) | 140.0 (44.8) | 4 (5.6%) |
| G2 | 122.8 (42.0) | 41 (12.1%) | 132.2 (36.1) | 14 (4.1%) | 140.1 (39.4) | 13 (3.8%) |
| G3 | 133.3 (41.2) | 6 (4.6%) | 134.2 (34.8) | 6 (4.6%) | 139.2 (55.1) | 8 (6.1%) |
APMHR, age-predicted maximal heart rate; BCi, Brawner chronotropic index; G1, group 1; G2, group 2; G3, group 3.
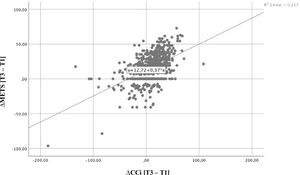
Functional capacity increased significantly from 8.6 (2.3) METS at T1 to 10.7 (2.1) METS at T2; plateauing at 10.65 (2.3) METS at T3. In G1, the values were 8.5 (2.6), 10.8 (2.7) and 11.0 (2.8) METS at T1, T2 and T3, respectively. With regard to G2, functional capacity was 8.6 (2.3), 10.7 (2.0) and 10.7 (2.3) METS at each sequential timepoint and, finally, the values for G3 were 8.5 (2.1), 10.6 (2.0) and 10.4 (2.0) METS. There was a positive correlation between improvement in functional capacity and increasing Ci (CCi and BCi) in the population and in each individualized group (Figures 1 and 2), which was more significant for CCi. Data showed that an average increase in 1.0% in CCi between T1 and T3 was associated with an average increase in functional capacity of 0.37 METS (95% confidence interval): 0.31-0.43; p<0.001), irrespective of age, gender, BB dose and BB dose change overtime.
Chronotropic response to exercise is a strong predictor of CV morbidity and mortality both in healthy subjects and in those with CAD. In this study we found that engaging in a CRP is associated with a short and long-term improvement in chronotropic response, irrespective of age, gender and use of BB.
Exercise testing is usually performed to determine whether new or worsening myocardial ischemia is present, but it may also be performed to evaluate a therapeutic regimen and/or develop an exercise prescription.12 In this context, assessing HR response to exercise and defining CI based on baseline exercise testing performance is cumbersome since there are different accepted definitions and cut-offs for chronotropic response and no consideration for the level of effort achieved and reason for exercise test termination. These may be some of the reasons why evaluation of HR response and CI is often overlooked in clinical practice,3 The end of the exercise test must be guided by symptoms and subjective perception of effort when other methods are not available, but the patient must be encouraged to continue until possible,1 as an abnormal chronotropic response provides prognostic information that is independent of myocardial perfusion – the combination of a myocardial perfusion abnormality and an abnormal Ci suggests a worse prognosis than either abnormality alone.13
Chronotropic index is common in patients with CV disease and is an important predictor of major adverse events and overall mortality. It reflects an imbalance in the autonomic nervous system,3 common in the early stages after ACS, as demonstrated by experimental and clinical studies.14 It has been well established that physical exercise promotes beneficial autonomic adaptations in patients after myocardial infarction including reduced resting HR, increased HR reserve and a steeper decrease in HR at 1 and 3 minutes after exercise termination. BB therapy seems to enhance these effects by promoting a shift in CV autonomic tone toward lower sympathetic and increased parasympathetic activity.15 Therefore, the combination of exercise training with BB therapy seems promising for CI improvement following ACS. Nevertheless, BB influence on HR response to exercise hinders interpretation and comparability of chronotropic response to exercise and renders the use of APMHR equations imprecise.12,16,17
Higher resting HR is associated with higher total and CV mortality and risk for major CV events.2,18 It has been suggested that the magnitude of increased CV mortality risk is higher than ischemic ST depression19 and that it is independent of other factors such as age, gender, functional capacity, other CV risk factors and even ST-segment changes during exercise.20 On the other hand, blunted HR response to exercise also has a prognostic value, independent of the presence of CAD or left ventricular disfunction.9,21 Despite the high rate of BB use in outpatients with stable CAD and post-ACS, most patients have, as in our study, a resting HR>70 bpm,16,22 reflecting an underdosing of BB possibly due to worries regarding patient tolerance and/or clinician decision.
Concerning the definition of CI, the use of different criteria for patients taking BB has been contradicted by some studies, based on the possible absence of any effect of this medication on the occurrence of CI, including at high doses.23 Nevertheless, we found that the prevalence of CI is highly dependent on the definition used, with values up to 73.7%, when using the APMHR and the CCi>80% cut-off at baseline, to 11.2%, when using the BCi equation and the BCi>80% cut-off at baseline. On the other hand, adding more variables would reduce applicability to clinical use. The BCi equation is found to be superior to the conventional equation for those with known or suspected CV disease11 and it appears to be a valid application in the setting of CRP. Chronotropic adaptations to exercise with increased HR variability seem to be independent of BB use and may in fact be potentiated by its use.14
There is substantial variability in the individual effect of BB on maximal HR and on functional capacity in CVD patients.24 Not considering the negative effect of BB on maximal HR, including the impact of dose modification, may lead to overtraining and increased risk of exercise-related adverse events.11,16 Overall, besides the effects on CV events and mortality, CRP improves exercise capacity with most benefit obtained in those more severely limited. We found that improvements in exercise capacity positively correlates to improvements in CCi, independent of age, gender and BB therapy or BB dose modification. Nevertheless, more studies are needed to calibrate the APMHR for those with CV disease and taking BB as well as to establish a universal threshold for diagnosis of CI in this patient population.
LimitationsThere were some limitations in this study. First of all, it is a descriptive study, with a relatively small sample and no control group. There was no information regarding the reasons for BB use and BB dose modification throughout the study period. Disease severity in our patients was somewhat mild, in accordance with the CRP admission criteria, and the NYHA functional classification was low. No information regarding physical activity habits outside the CRP exercise sessions was collected. Since our objective was the short-term effect of exercise training on chronotropic response, we did not collect information on major cardiovascular events.
ConclusionsWe found that Ci significantly improves with CRP after an ACS, irrespective of BB dose changes, and that CCi is more closely related to improvement in functional capacity than BCi. However, it is unclear which maximal predicted HR equation is more appropriate to use when BB therapy is held prior to exercise stress testing. This data supports the need for an appropriate screening for HR responses during exercise testing and recovery, as it can be helpful for risk stratification and prognosis definition.
Conflicts of interestThe author has no conflicts of interest to declare.
The authors wish to thank to Fernando Parada, MD, and João Barroso Monteiro, MD, former and current director of the Department of Physical Medicine & Rehabilitation at Centro Hospitalar e Universitário de São João, for their scientific guidance and manuscript revision. We also would like to thank the physiotherapists Judite Rodrigues, Paula Silva and Susana Oliveira for their valuable contribution when carrying out the exercise sessions.