Neurocardiogenic syncope (NCS) is a common clinical entity resulting from an excessive reflex autonomic response, particularly during orthostatism. Treatment options are controversial and of limited effectiveness. Tilt training (TT) is a promising option to treat these patients. However, its mechanism of action and clinical impact remain unclear.
ObjectiveTo characterize hemodynamic and autonomic responses during a TT program in patients with NCS refractory to conventional measures.
MethodsWe studied 28 patients (50% male, mean age 41±14 years) without structural heart disease, with NCS documented by tilt testing. The TT program included nine tilt sessions (three times a week, 30min) (60° – 6 sessions, 70° – 3 sessions), under ECG and blood pressure monitoring combined with home orthostatic self-training and 10° head-up during sleep. Systolic volume, cardiac output, total peripheral resistance, baroreflex sensitivity and heart-rate variability were computed. Patients were reassessed at 1 month and every 6 months for a maximum of 36 months (24±12 months).
ResultsOver the course of the TT program there was a significant increase in total peripheral resistance (1485±225 vs. 1591±187dynscm−5, p<0.05), with a decrease in standard deviation (206±60 vs. 150±42, p<0.05). During follow-up, syncope recurred in five patients (19%), with a significant reduction in the number of episodes (4.0±3.2/patient in the 12 months before TT vs. 1.4±0.8/patient post-TT, p<0.05).
ConclusionIn refractory NCS, TT may be an effective therapeutic option, with long-term benefits. These results appear to be due to an increase in vasoconstrictor reserve combined with a reduction in its variance.
A síncope neurocardiogénica (SNc) é uma entidade clínica comum, resultante de uma resposta autonómica reflexa excessiva durante o stress ortostático. As diferentes opções terapêuticas são controversas e de eficácia limitada. O treino de ortostatismo (TTr) tem-se mostrado uma alternativa prometedora no tratamento destes doentes (D). No entanto, permanece por esclarecer o seu mecanismo de acção e o impacto clínico numa população com SNc recorrente.
ObjectivoCaracterizar a resposta hemodinâmica e autonómica durante um programa de TTr em doentes com SNc refractária às medidas convencionais.
População e métodosForam estudados 28D (50% do sexo masculino, 41±14 anos), sem evidência de cardiopatia, com SNc documentada em teste de ortostatismo passivo. O TTr incluiu 9 sessões hospitalares (3×/semana, 30 minutos) com monitorização contínua de pressão arterial e frequência cardíaca (60° – 6 sessões – 70° – 3 sessões), complementadas com treino diário no domicílio e elevação da cabeceira a 10° durante o sono. O volume sistólico, o débito cardíaco, a resistência vascular periférica, a sensibilidade do barorreflexo e a variabilidade da frequência cardíaca foram calculados. Todos os doentes foram reavaliados no fim do 1° mês e no final de cada 6 meses num período máximo de 36 meses (follow-up 24±12 meses).
ResultadosAo longo das sessões de TTr verificou-se um aumento significativo e consistente da resistência total periférica (1485±225 vs. 1591±187 dyne*s/cm5, p<0,05) associado a uma diminuição do seu desvio-padrão (206±60 vs. 150±42, p<0,05). Durante o período de follow-up, houve recorrência de síncope em 5D (19%), com redução significativa do numero de síncopes (4.0±3.2/D nos 12 meses pre-TTr vs. 1.4±0.8/D pos-TTr, p<0.05).
ConclusãoEm doentes com SNc refractária, o TTr mostrou ser uma opção terapêutica eficaz, com beneficio a longo-prazo. A melhor tolerância ao ortostatismo parece resultar do aumento da reserva vasoconstritora e da sua menor variabilidade.
Syncope is defined as a transient loss of consciousness due to transient global cerebral hypoperfusion characterized by rapid onset, short duration, and spontaneous complete recovery. It is common in the general population, with an estimated incidence of 18.1–39.7events/1000 person-years,1 and has serious effects on quality of life, including high morbidity, risk of physical injury and work absenteeism.2,3
Neurocardiogenic syncope (NCS) is the most common form, with a higher incidence in young adults.4,5 Its pathophysiology is poorly understood, but it has been demonstrated that alterations in the reactions of the autonomic nervous system to stressful stimuli such as active orthostatism are involved in triggering syncope.6
Various treatment options have been proposed over the years for NCS, ranging from behavior modification to cardiac pacing and various types of drug therapy, but none has been shown to be fully effective.
Tilt training (TT), a new non-pharmacological treatment for NCS, was proposed in 1998 by Ector et al.,7 who showed that repeated and prolonged exposure of the cardiovascular system to orthostatic stimuli had therapeutic effects in patients with NCS. The effectiveness of tilt training has been evaluated in several non-randomized observational studies,8–10 but the results have been inconsistent, varying according to the training protocol and particularly patient compliance. The mechanisms of action are largely unknown; it is thought that desensitization of cardiopulmonary receptors to orthostatism may be involved, as well as autonomic remodeling and alterations in baroreflex activity.
The aim of this study was to clarify the mechanisms of action of tilt training, specifically to characterize hemodynamic and autonomic responses during a TT program in patients with NCS refractory to conventional measures.
Part of this work was awarded the prize for best communication at CPC2010.
MethodsPopulationBetween 2007 and 2010 we studied 28 patients (50% male, mean age 41±14 years), each with more than two syncopal episodes in the previous six months. All had NCS refractory to conventional measures (compression stockings and counterpulsation measures, midodrine, and paroxetine) and documented by tilt testing in accordance with our center's standard protocol. Briefly, after a supine resting period, the patient underwent passive tilt testing for 20 min at 70°; if no spontaneous syncope had occurred 375μg sublingual nitrates were administered. The test was terminated either by a positive response or 20 min after nitrate administration.11 A positive test was defined as reproduction of syncope in association with bradycardia (decrease in heart rate >30% of the maximum value in the upright position), hypotension (decrease in heart rate [HR] of >50% of the maximum value in the upright position), or both, and classified according to the VASIS system.11 The following exclusion criteria were applied: (1) structural heart disease or cardiac rhythm disturbance; (2) neurologically mediated syncope including classical or delayed orthostatic hypotension; (3) excessive reaction to nitrates; (4) refusal to consent to the test; (5) physical inability to remain standing for 30min; (6) impossibility of suspending cardiovascular medication that could interfere with assessment of the autonomic nervous system; and (7) pregnancy.
The study complies with the Declaration of Helsinki and informed consent was obtained from all participants.
Tilt training programThe TT protocol has two simultaneous components. The first, in-hospital, component consists of nine tilt training sessions three times a week in the mornings after a light breakfast, without ingestion of caffeine or other xanthines. Training took place in a laboratory specifically designed for autonomic evaluation, in a calm environment and with controlled temperature and humidity. After 15min of supine (0°) rest, the patient was placed on a tilt table with feet supported and with restraining straps to prevent falls in the event of syncope. For the first two weeks the tilt table was at 60° and at 70° for the third week. During training the patient underwent continuous non-invasive monitoring of BP, electrocardiogram (ECG) and thoracic impedance (Task Force Monitor, CNSystems, Graz, Austria), and the test was stopped if symptoms occurred. The hospital sessions were complemented by daily home training, with the patient in orthostatic position at 60° to a flat vertical surface with feet apart about 15cm from the wall for 20min, and 10° head-up during sleep. Patients were instructed to stop the daily orthostatic maneuver whenever they felt the onset of symptoms. All patients were followed clinically at 1 month and every 6 months for a maximum of 36 months.
Data acquisition and analysisRR intervals (RRI) and systolic blood pressure (SBP) were recorded continuously, beat-to-beat (Task Force Monitor, CNSystems, Graz, Austria). Other hemodynamic parameters – HR, mean blood pressure (MBP), systolic volume (SV), cardiac output (CO), and peripheral vascular resistance (PVR) – were calculated on the basis of thoracic impedance (Task Force Monitor, CNSystems, Graz, Austria).
The data were analyzed using an interface programmed in MATLAB (MathWorks, USA), implementing a routine to detect SBP peaks and the fiducial points of the R waves of each ECG complex, beat-to-beat, in order to construct a time curve of BP (systogram) and of HR (tachogram). The reconstructed signals were used to calculate HR and BP variability and baroreflex sensitivity.
Heart rate and systolic blood pressure variabilityAutoregression techniques were used to extract the characteristics of the cardiovascular parameters HR and BP. The total maneuver time was divided into 5-min segments, to facilitate computation and to better visualize the dynamics of cardiovascular alterations taking place during the maneuver. A frequency power spectrum was obtained for each interval and two main bands were isolated: high frequency (HF; 0.15–0.4Hz), an indicator of parasympathetic activity, and low frequency (LF; 0.04–0.15Hz), which indicates sympathetic activity.12
Baroreflex sensitivity and effectivenessBaroreflex sensitivity is a measure of overall response to baroreceptor activation that assesses the relationship between simultaneous changes in HR and BP. In the present work baroreflex sensitivity was estimated using the sequence method. Briefly, the SBP signal was analyzed to identify sequences (ramps) of three or more heartbeats with a progressive increase (up-ramp) or decrease (down-ramp) in BP of at least 1mmHg. The algorithm identified spontaneous baroreflex sequences, defined as SBP ramps followed by concomitant and concordant variations of ≥5ms in RRI that were analyzed in three time lags, of −0, −1 and −2 heartbeats. Each sequence was included only once.13 For each spontaneous sequence the slope of the linear relation between the SPB ramps and RRIs was calculated. Only periods with correlation coefficient >0.8 were analyzed.
For each period selected for analysis, the baroreflex effectiveness index (BEI) was calculated, defined as the ratio between the total number of baroreflex sequences detected and the total number of SBP ramps.13 The higher the BEI the more SBP ramps are followed by alterations in RRI, and hence the more effective the baroreflex in bringing about the necessary cardiovascular adaptations.
Statistical analysisFor the statistical analysis, performed using SPSS version 18, each session was divided into seven 5-min periods, the first being the baseline period and the others on the tilt table.
Continuous variables are presented as means±standard deviation and were tested for normality by the Kolmogorov–Smirnov test. The results of the first and ninth TT sessions were compared using the Student's t test for paired data. Values of p<0.05 were considered statistically significant.
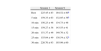
ResultsWe studied 28 patients, 14 male, mean age 41±14 years. The mean number of syncopal episodes before beginning the TT program was 4.0±3.2/patient/year (Table 1).
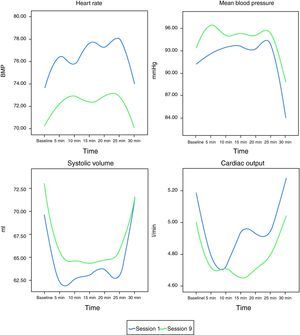
Heart rate: HR tended to decrease between the first and the ninth TT sessions (Figure 1).
Mean blood pressure and systolic volume: MBP and SV showed a non-significant increase between the first and the ninth TT sessions (Figure 1).
Cardiac output: No changes in CO were seen between the first and the ninth TT sessions (Figure 1).
Peripheral vascular resistance: A statistically significant increase in PVR (Figure 2 and Table 2) was observed between the first and the ninth TT sessions (1485±225 vs. 1591±187dynscm−5, p<0.05), with a decrease in standard deviation (206±60 vs. 150±42, p<0.05). This was reflected in a tendency towards a lower dynamic equilibrium value (Table 3).
In the assessment of cardiac autonomic function over the course of the TT program, analysis of HR and BP variability using autoregression techniques showed an increase in sympathetic tone reflected in a progressive increase in overall autonomic activity during TT (Table 4) and a significant increase in indices of variability in the LF (sympathetic) and HF (parasympathetic) bands. This increase was also seen, although without statistical significance, in changes in BEI (Table 5).
Changes in autonomic outflow to the cardiovascular system between the first and the ninth tilt training sessions.
| 20min | 25min | 30min | ||||
| Session 1 | Session 9 | Session 1 | Session 9 | Session 1 | Session 9 | |
| RRI (ms2) | ||||||
| LF | 500.87±106 | 942.90±280a | 544.08±146 | 914.64±225a | 712.91±288 | 1063.4±216a |
| HF | 217±74 | 335.18±103a | 182.06±54 | 325.27±100a | 208.17±62 | 524.6±120a |
| SBP (mmHg2) | ||||||
| LF | 5.11±0.8 | 7.56±0.9a | 5.32±0.7 | 7.42±0.8a | 5.64±0.7 | 6.92±0.7a |
| HF | 1.62±0.2 | 2.58±0.6a | 1.49±0.2 | 2.45±0.6a | 2.05±0.6 | 1.95±0.3 |
Changes in baroreflex sensitivity between the first and the ninth tilt training sessions.
| Session 1 | Session 9 | p | |
| Rest | 57.971±17 | 65.13±18 | 0.16 |
| 5min | 61.06±20 | 69.69±17 | 0.08 |
| 10min | 66.631±13 | 65.14±15 | 0.46 |
| 15min | 63.771±15 | 64.04±20 | 0.45 |
| 20min | 63.21±18 | 64.41±17 | 0.31 |
| 25min | 62.360±14 | 67.95±16 | 0.08 |
| 30min | 65.73±14 | 64.95±19 | 0.5 |
There was a significant decrease in the number of episodes of syncope (4.0±3.2/patient in the 12 months before TT vs. 1.4±0.8/patient post-TT, p<0.05). In five patients no change in the pattern of episodes was seen. Although all patients completed all the in-hospital sessions, after one year 11 (39%) had stopped home self-training due to symptomatic improvement.
DiscussionTo the best of our knowledge, this is the first study to combine assessment of alterations in cardiocirculatory parameters, cardiovascular autonomic function and baroreflex sensitivity resulting from tilt training in patients with NCS refractory to conventional measures. We demonstrated a significant increase in vasoconstrictor reserve in these patients after nine TT sessions, as well as significant increases in baroreflex sensitivity as determined by the sequence method and in parameters of HR variability (LF and HF) calculated by autoregression techniques. Our results show that TT significantly increases autonomic tone (both sympathetic and parasympathetic), as well as baroreflex sensitivity, after three weeks of training. This response, which in our opinion is due mainly to remodeling of autonomic activity in the periphery, in particular of the cardiovascular system, was beneficial, significantly reducing the number of syncopal episodes, and confirms that TT should be used as a complement to conventional therapeutic measures.
NCS is the most common cause of transient loss of conscious. It can be triggered by a variety of stimuli such as emotional stress, heat or prolonged standing. Although prognosis is generally good, it is associated with a marked reduction in quality of life, due to both risk of physical injury and loss of self-confidence induced by fear of further episodes.
The therapeutic options for these patients are limited to preventing new episodes and resulting physical injury, and improving their general quality of life. The most widely used measures include advice on avoiding possible triggers, recognition of prodromes and maneuvers that can abort a syncopal episode. In some patients drug therapy can complement these measures, while cardiac pacing is reserved for specific groups.1
Studies have indicated certain limitations to tilt training, the main one being patient compliance with the long treatment period.14,15 Compliance is in fact principally a problem in patients who become asymptomatic after a few sessions, and education and motivation are thus essential.
The ESC guidelines on syncope identify the fact that randomized trials have failed to demonstrate the value of tilt training as a reason for the limited use of this therapy. Comparing our study with others14,15 reveals differences that could affect the conclusions drawn, particularly the inclusion criteria, the training protocol, and most importantly, the diversity of the endpoints, which would tend to lead to differences in interpretation of the results and hence in evaluation of the efficacy of tilt training. Thus, while we set out to assess the effect of TT complemented with home self-training on reducing the number of syncopal episodes, thereby improving patients’ quality of life, Foglia-Manzillo et al.14 used a positive tilt test one month after tilt training as the endpoint. The question arises as to whether the aim of training is to bring about changes that enable individuals to improve their daily lives, or to prepare the individual to react to intense stimuli such as changes in posture. After assessing our patients, we are of the opinion that the choice of endpoint should incline towards the first, and in this case tilt training was shown to be effective.
Studies by Abe et al.16,17 and Reybrouck et al.18,19 have similar conclusions to ours. Abe et al., using a similar protocol to ours, observed no spontaneous or orthostatic stress-induced syncopal episodes after TT, while Reybrouck et al. reported a significantly lower number of episodes after TT complemented by home self-training. They also reported that patients who did not complete the TT program had no episodes of syncope up to a year after dropping out, which suggests that autonomic activity had been restored in these patients.
However, although the efficacy of tilt training has been demonstrated, the physiological mechanisms underlying the improvement in these patients’ general condition are not entirely clear. Previous studies have indicated that humoral mechanisms – the renin–angiotensin system20, baroreflex changes, and overall autonomic alterations – may be involved in the responses observed.21–24 In particular, Verheyden et al.23 observed increased vasoconstrictor reserve without changes in baroreflex or autonomic tone, while Tan et al.24 showed increases in HF and LF indicators of increased autonomic tone. Our study is the first to relate hemodynamic changes to modifications in autonomic tone assessed by changes in BP and HR variability. Our results show a significant increase in PVR and in LF and HF, without significant alterations in other variables. This implies that the increase in PVR is due mainly to increased sympathetic activity in the vascular system that maintains BP without large variations during postural changes. At the same time, a slight rise in mean BP is seen, accompanied as expected by reduced chronotropic response, reflected by increased HF and a slight, non-significant increase in baroreflex sensitivity and its ability to adapt to changes in posture. Besides these changes in PVR, it is also worth noting the decrease in standard deviation, which we take to reflect peripheral and somatic sympathetic remodeling, indicating a reduction in the variations around a mean equilibrium value that enables the individual to adapt better (without large variations) to postural changes. Furthermore, although not analyzed in the present study, TT may also increase muscle tone in the lower limbs, which together with the increase in PVR would improve postural adaptation.
In conclusion, in patients with refractory neurocardiogenic syncope, our training protocol may be an effective therapeutic option, with long-term benefits in terms of greater tolerance to orthostatism, through three main mechanisms: an increase in, and lower variability of, vasoconstrictor reserve; overall increase in autonomic tone; and changes in baroreflex sensitivity. This suggests that it improves patients’ quality of life.
Please cite this article as: Laranjo, S. O treino de ortostatismo (tilt training) aumenta a reserva vasoconstritora em doentes com síncope reflexa neurocardiogénica. Rev Port Cardiol. 2012;31(7-8):469-476.