Venous thromboembolism, risk of which is increased in surgical patients, is a preventable cause of morbidity and death. The primary objective of this study was to estimate the incidence of symptomatic postoperative venous thromboembolism in adults at a tertiary university hospital, overall and by surgical specialty. The secondary objective was to analyze severity of and mortality from thromboembolic events.
MethodsWe performed a retrospective study to identify cases of in-hospital postoperative venous thromboembolism, encoded by the International Classification of Diseases, Ninth Revision, according to the Joint Commission International criteria. Adult patients admitted for surgery in 2008-2012 were included.
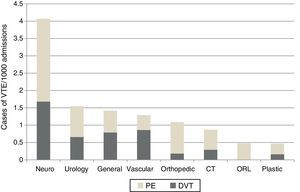
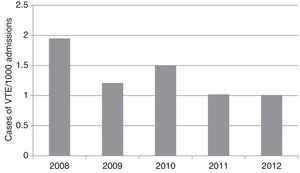
ResultsAmong 67635 hospitalizations, 90 cases of postoperative symptomatic venous thromboembolism were identified (median age 59 years), corresponding to an incidence of 1.33/1000 admissions (95% confidence interval [CI] 1.1-1.6/1000). Neurosurgery had the highest risk (4.07/1000), followed by urological surgery and general surgery (p<0.001). There were 50 cases of pulmonary embolism, 11 of which were fatal. Of the 90 cases, 12.2% occurred under neuraxial anesthesia and 55.1% in patients with American Society of Anesthesiology III physical status. At least 37.7% of patients with events received a prophylactic dose of injectable anticoagulant postoperatively. The overall risk decreased from 2008 to 2012. Venous thromboembolism-associated mortality during hospitalization was 21.1% (95% CI 13.6-30.4).
ConclusionsThe incidence of postoperative symptomatic venous thromboembolism was 1.33/1000. Neurosurgery showed the greatest risk. Mortality was 21.1%.
O tromboembolismo venoso, cujo risco está aumentado no doente cirúrgico, é uma causa evitável de morbimortalidade. O objetivo primário deste estudo foi estimar o risco de tromboembolismo venoso sintomático pós-operatório global e por especialidade cirúrgica, num hospital terciário. Secundariamente, foram analisadas a gravidade e mortalidade dos eventos tromboembólicos.
MétodosFoi realizado um estudo retrospetivo para a identificação de casos de tromboembolismo venoso pós-operatório intra-hospitalar, codificados pela Classificação Internacional de Doenças – 9.ª revisão, pelos critérios da Joint Commission International. Foram incluídos episódios de internamento de doentes adultos, operados, no período 2008-2012.
ResultadosEm 67635 episódios de internamento com cirurgia identificaram-se 90 casos de tromboembolismo venoso pós-operatório (mediana de idades: 59 anos), correspondendo a um risco de 1,33/1000 episódios (intervalo de confiança a 95% [IC95%], 1,1-1,6/1000). A neurocirurgia apresentou maior risco (4,07/1000), seguida pela urologia e pela cirurgia geral p<0,001. Houve 50 episódios de embolia pulmonar, dos quais 11 foram fatais. Dos 90 casos, 12,2% decorreram sob anestesia do neuro-eixo e 55,1% em doentes com estado físico ASA III. Foi administrada dose profilática de anticoagulante injetável no pós-operatório a, pelo menos, 37,7% dos doentes. O risco decresceu de 2008 até 2012. A mortalidade associada aos eventos de tromboembolismo venoso durante o internamento foi 21,1% (IC95%, 13,6-30,4).
ConclusõesO risco de tromboembolismo venoso sintomático pós-operatório foi de 1,33/1000. A neurocirurgia apresentou maior risco. A mortalidade foi de 21,1%.
Venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is a leading cause of morbidity and mortality and results in high financial costs, and is considered a major public health problem. The estimated annual incidence rates of VTE range between 104 and 183/100000 person-years1; early mortality is 12.6% and five-year mortality is 50-60% for PE and 25% for DVT.2
It is difficult to obtain reliable and comparable estimates of VTE incidence, for various reasons. Symptoms and clinical signs are non-specific, and hence only 50% of cases are diagnosed and the predictive value of screening asymptomatic patients is low.3 These factors help explain the variations seen in epidemiological data from different studies, although there are also differences related to ethnicity.1
Surgical patients are at increased risk for VTE, which in the absence of thromboprophylaxis ranges between 15% and 60% depending on the type of surgery; it is highest in major orthopedic procedures.4,5 Individual patient characteristics, type of anesthesia, and length of procedure and hospital stay also affect risk.4,5
The ENDORSE study,6 which analyzed VTE risk in 32 countries, showed that of the 762 surgical patients assessed in Portugal, 69% were at risk. Despite the importance of awareness of outcome indicators, there have been few epidemiological studies on postoperative VTE in Portugal.
ObjectivesThe primary objective of the postoperative venous thromboembolism (TREVO) study was to estimate the incidence of symptomatic postoperative VTE, overall and by surgical specialty, at a tertiary hospital. The secondary objective was to analyze severity of and mortality from thromboembolic events, including the characteristics of the patients involved and their treatment.
MethodsTREVO is a retrospective epidemiological study of an adult population of surgical patients at Centro Hospitalar de São João, a tertiary university hospital. The study was approved by the institution's ethics committee.
Study designAll hospitalizations recorded in the hospital's database of patients aged 18 or over admitted for at least one elective or urgent surgical procedure between January 1, 2008 and December 31, 2012 were analyzed.
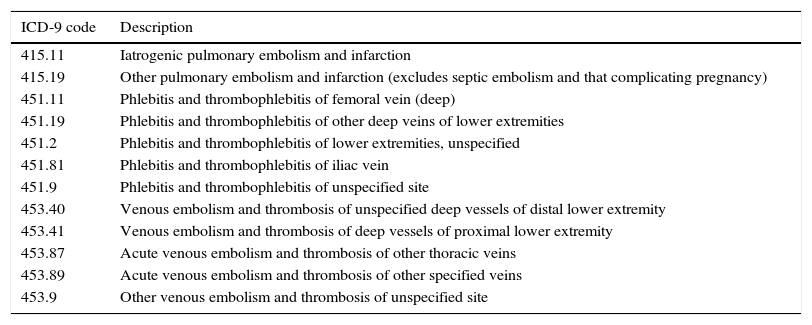
Cases of VTE as a secondary diagnosis during the first 120 days of hospital stay were identified based on the codes of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9). The criteria used were those of the Joint Commission International7 (Table 1).
Joint Commission International criteria for a diagnosis of venous thromboembolism.
| ICD-9 code | Description |
|---|---|
| 415.11 | Iatrogenic pulmonary embolism and infarction |
| 415.19 | Other pulmonary embolism and infarction (excludes septic embolism and that complicating pregnancy) |
| 451.11 | Phlebitis and thrombophlebitis of femoral vein (deep) |
| 451.19 | Phlebitis and thrombophlebitis of other deep veins of lower extremities |
| 451.2 | Phlebitis and thrombophlebitis of lower extremities, unspecified |
| 451.81 | Phlebitis and thrombophlebitis of iliac vein |
| 451.9 | Phlebitis and thrombophlebitis of unspecified site |
| 453.40 | Venous embolism and thrombosis of unspecified deep vessels of distal lower extremity |
| 453.41 | Venous embolism and thrombosis of deep vessels of proximal lower extremity |
| 453.87 | Acute venous embolism and thrombosis of other thoracic veins |
| 453.89 | Acute venous embolism and thrombosis of other specified veins |
| 453.9 | Other venous embolism and thrombosis of unspecified site |
ICD-9: International Classification of Diseases, Ninth Revision.
Medical records, both electronic and paper versions, of the cases identified were reviewed. The relevant data were entered on a specially designed form, and included demographic characteristics and associated diseases, admission and discharge diagnoses, treatment details, including type of anesthesia, type of surgery, central venous catheterization, postoperative immobility for more than two days and prescription of postoperative thromboprophylactic drugs, and vital status at discharge. The severity of postoperative VTE was classified into four groups: fatal PE, non-fatal PE, DVT and other VTE.
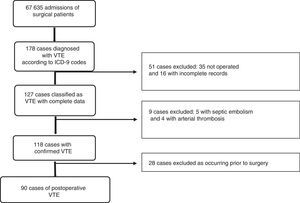
Surgical patients who were admitted but not operated, those with incomplete records and those in whom a secondary diagnosis of VTE was not confirmed were excluded, as were those in whom VTE occurred before surgery.
The selection of cases was based on a recorded diagnosis of VTE, supported by a report of imaging findings. PE was confirmed by spiral computed tomography, digital subtraction angiography or high-probability ventilation-perfusion scan; DVT by ultrasound or venography; and other VTE by ultrasound, venography or magnetic resonance angiography. The images were not reviewed by the investigators, who nevertheless checked the information recorded against the ICD-9 code.
The episodes initially identified were subsequently reviewed by a different investigator in order to confirm the data collected.
The outcome analyzed was symptomatic VTE, since the hospital's policy is to refer patients for imaging studies based on clinical assessment rather than to screen for VTE.
In cases in which there was more than one VTE event, only the most severe was considered in the statistical analysis.
Statistical analysisDescriptive statistics were used to analyze the data, expressed as medians and interquartile range (P25-P75) for quantitative variables and percentages for qualitative variables. Estimates are presented with 95% confidence intervals (CI). The incidence of VTE and PE among the subgroups was compared by the chi-square test. Tests for linear tendency were used to assess changes over time in the risk for a VTE event. The data were analyzed using Stata for Windows, version 11.1 (StataCorp LP, College Station, TX) and Microsoft Excel 2010 (Microsoft Corp., Redmond, WA).
ResultsCase selectionThe study sample consisted of 67635 admissions of adult patients for cardiothoracic, general, plastic, vascular, neurological, orthopedic, otorhinolaryngological or urological surgery.
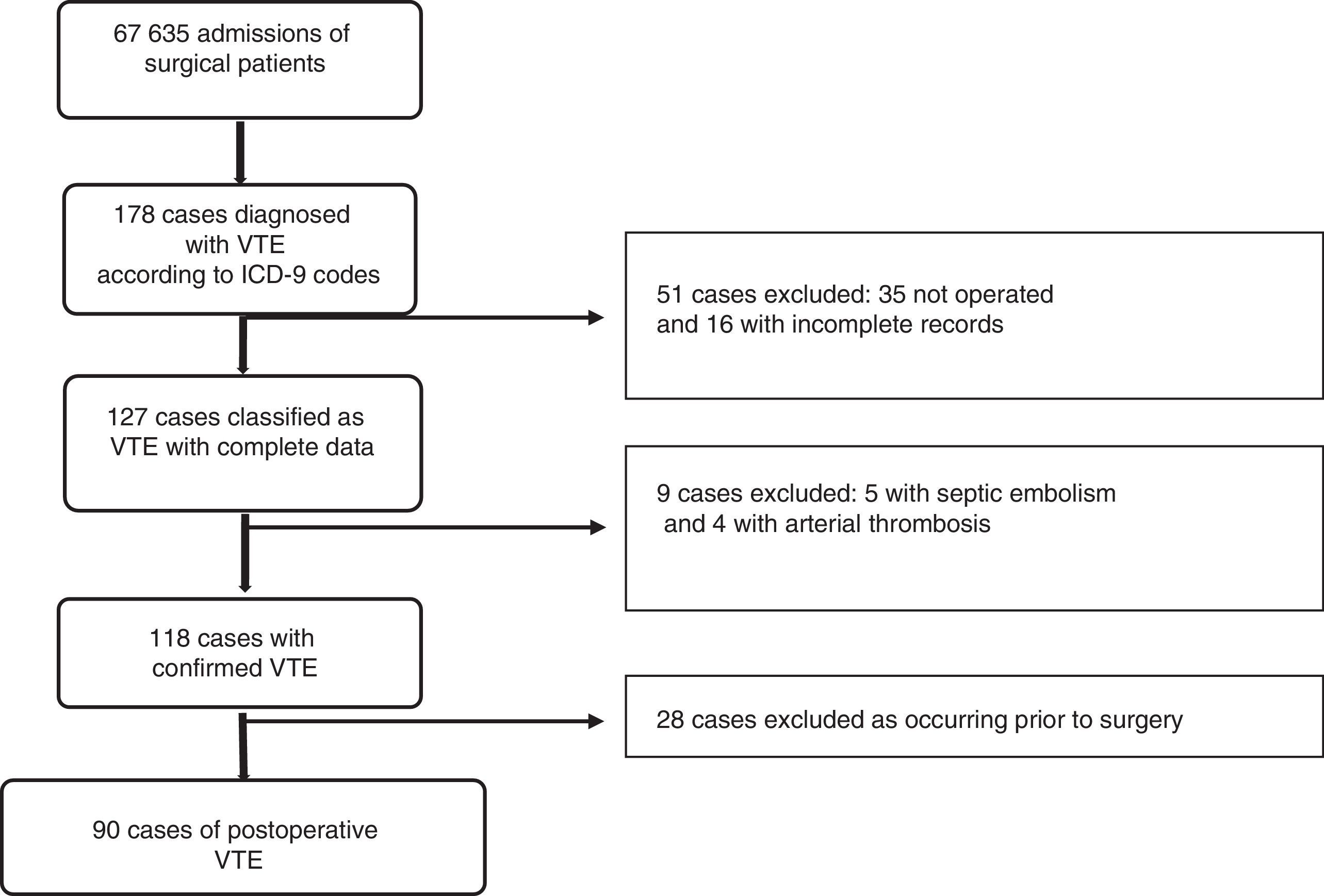
Of the 178 cases initially identified with VTE according to the ICD-9 diagnostic codes, 35 patients were excluded as they were not operated, 16 due to incomplete data, nine due to diagnostic codes inconsistent with the clinical information, and 28 because the VTE event occurred before surgery (Figure 1).
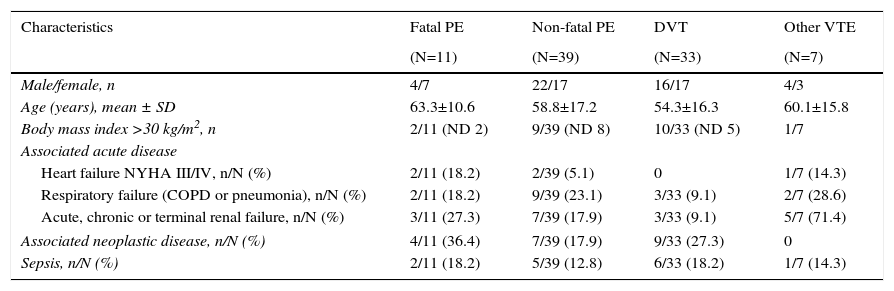
Demographic characteristicsThe overall incidence of VTE was similar in men and women (1.35 vs. 1.31/1000 admissions, respectively, p=0.96), but 63.6% of those with fatal PE were female.
The median age of those with VTE was 59 years (P25-P75: 46-70). There was no significant difference in mean age between cases of VTE and the overall study population (p=0.191). Fatal PE occurred at a mean age of 63.3±10.6 years. Patients with VTE tended to be younger (mean 54±16.3 years).
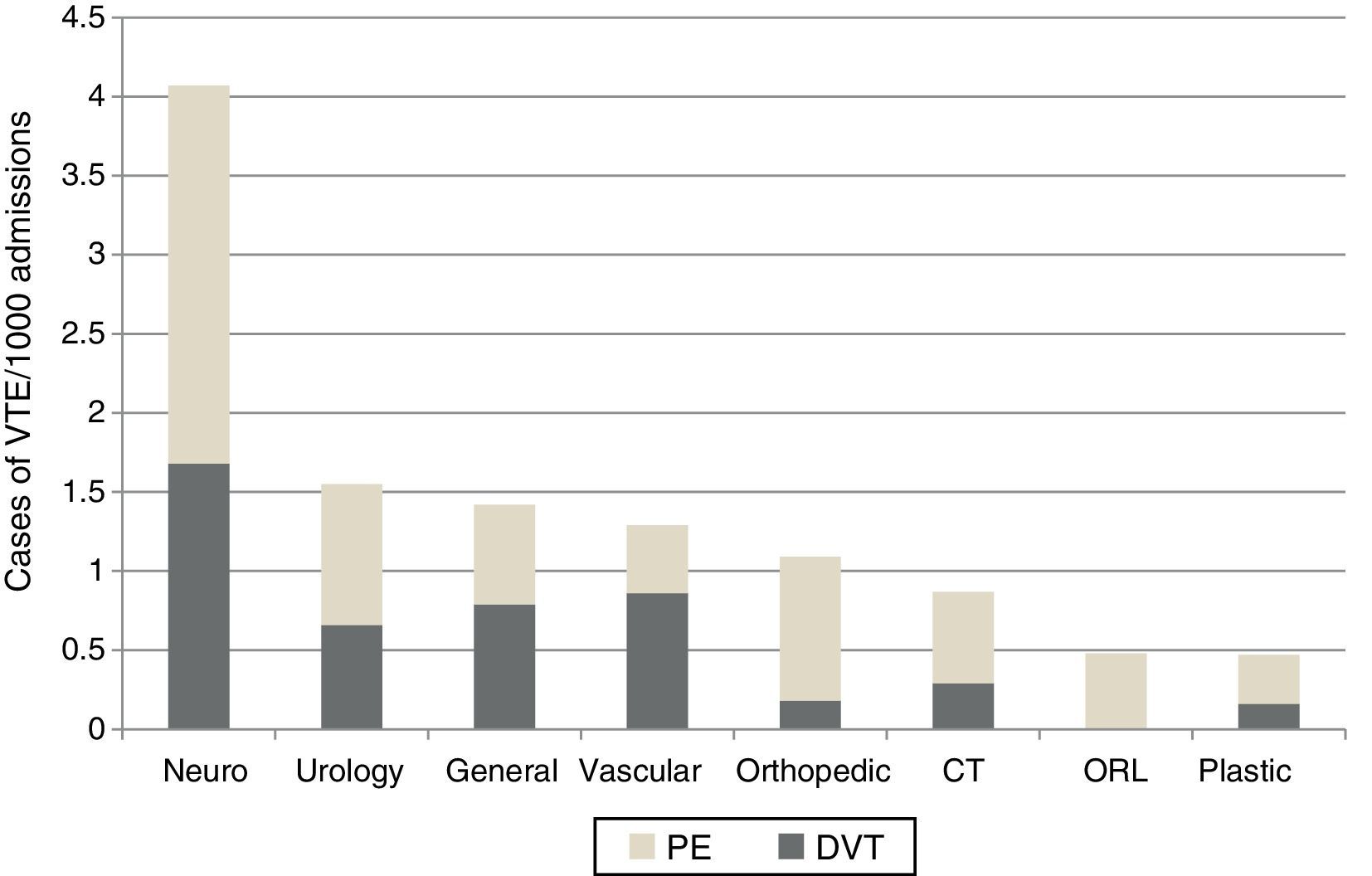
Risk by surgical specialtyThe 90 confirmed cases of symptomatic postoperative VTE correspond to an incidence of 1.33/1000 admissions (95% CI: 1.1-1.6/1000). Regarding estimated risk by surgical specialty, neurosurgery had the highest risk (4.07/1000), followed by urological surgery (1.55/1000) and general surgery (1.42/1000) (p<0.001). Plastic surgery had the lowest risk (0.47/1000) (Figure 2).
Among the neurosurgical cases, PE was observed in five procedures to remove neoplastic lesions (two acoustic neuromas, one astrocytoma, one hypophyseal adenoma and one meningioma) and in another five procedures (two to drain brain abscess, one brain biopsy, one to drain cerebral hemorrhage, and one to implant an intracranial pressure monitor). There were three cases of DVT in procedures to drain subdural hematomas and one in a procedure to drain an intracerebral hemorrhage. One patient with Parkinson's disease undergoing implantation of a deep brain stimulator had another type of VTE. None of the patients with neoplastic lesions had fatal PE.
Of the 14 urological patients, four underwent kidney transplantation and PE occurred in three of these and another type of VTE in one. One of the transplant patients presented PE, DVT and another type of VTE. This patient and another transplant recipient, both male, died. PE was also a complication in a transurethral resection of the prostate, a ureteroscopy with biopsy and a nephroureterectomy. All other episodes in urological patients were DVT.
Of the 90 cases of TVE, 11 (12.2%) occurred under neuraxial anesthesia, which in three cases was combined with general anesthesia and in two was combined subarachnoid and epidural block.
The distribution of TVE cases according to the American Society of Anesthesiology (ASA) classification of physical status was as follows: ASA III (55.1%), ASA II (21.4%) and ASA IV (13.5%).
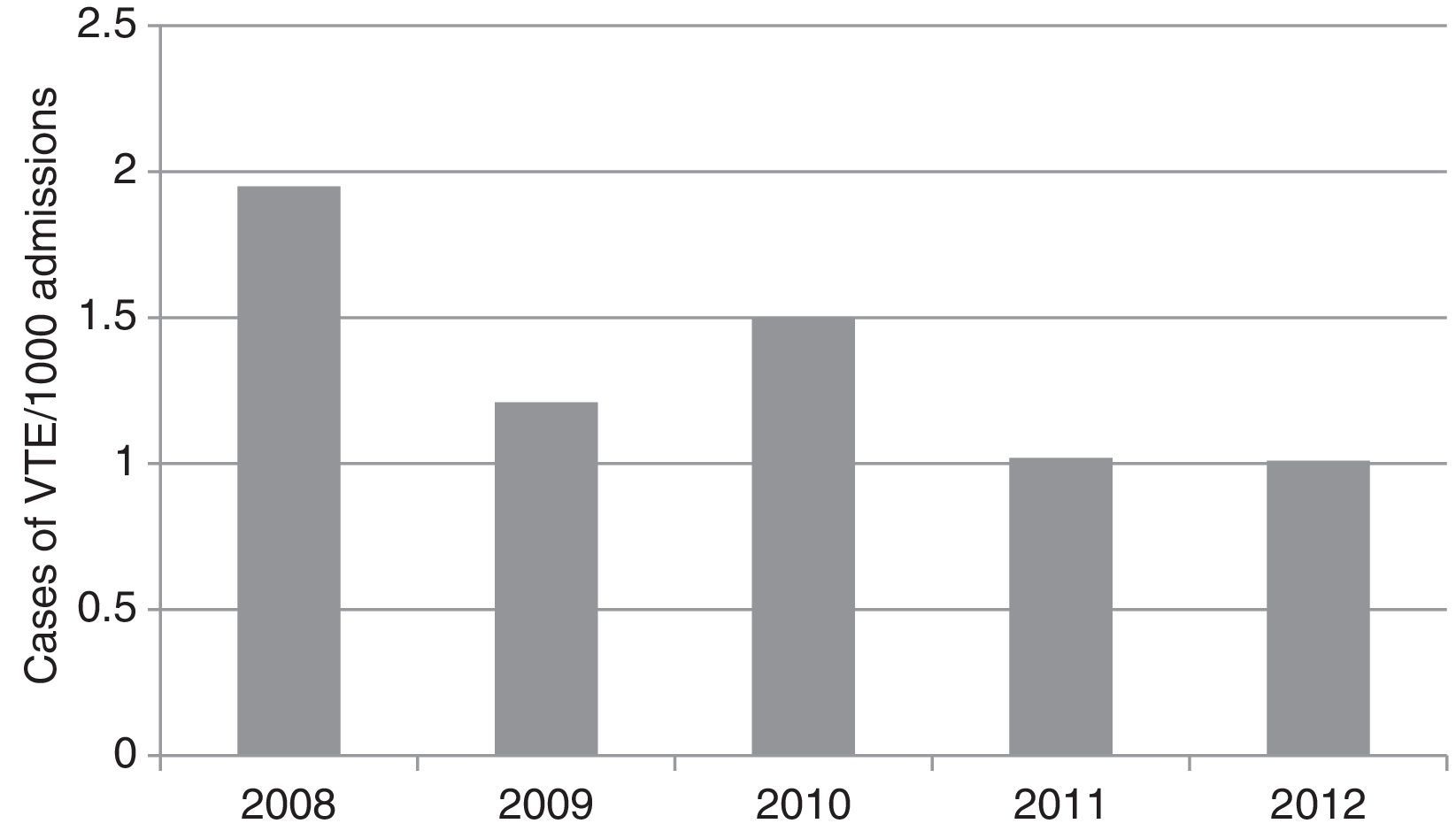
The overall incidence of TVE fell over the study period, from 1.95/1000 in 2008 to 1.01/1000 in 2012 (p=0.036 for linear tendency) (Figure 3).
Severity of eventsOf the total, 50 cases of PE were identified, corresponding to an incidence of 0.75/1000 episodes (95% CI: 0.56-0.99/1000), highest in neurosurgery (2.39/1000), followed by orthopedic (0.91/1000) and urological procedures (0.89/1000) (Figure 2).
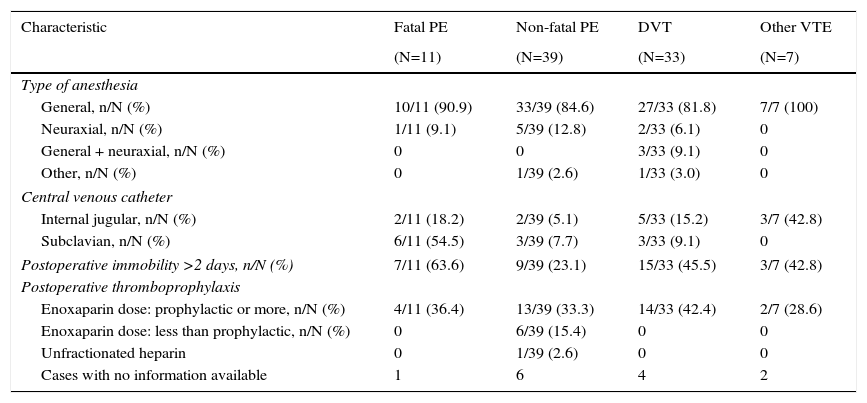
There were 11 fatal PE (22.0% mortality), most frequently associated with neoplastic disease or renal failure (Table 2). Over half of these patients had undergone central venous catheterization of the right subclavian vein, and 72.7% had a central catheter if those with catheterization of the internal jugular are included (Table 3).
Characteristics of patients according to type of thromboembolic event.
| Characteristics | Fatal PE | Non-fatal PE | DVT | Other VTE |
|---|---|---|---|---|
| (N=11) | (N=39) | (N=33) | (N=7) | |
| Male/female, n | 4/7 | 22/17 | 16/17 | 4/3 |
| Age (years), mean ± SD | 63.3±10.6 | 58.8±17.2 | 54.3±16.3 | 60.1±15.8 |
| Body mass index >30 kg/m2, n | 2/11 (ND 2) | 9/39 (ND 8) | 10/33 (ND 5) | 1/7 |
| Associated acute disease | ||||
| Heart failure NYHA III/IV, n/N (%) | 2/11 (18.2) | 2/39 (5.1) | 0 | 1/7 (14.3) |
| Respiratory failure (COPD or pneumonia), n/N (%) | 2/11 (18.2) | 9/39 (23.1) | 3/33 (9.1) | 2/7 (28.6) |
| Acute, chronic or terminal renal failure, n/N (%) | 3/11 (27.3) | 7/39 (17.9) | 3/33 (9.1) | 5/7 (71.4) |
| Associated neoplastic disease, n/N (%) | 4/11 (36.4) | 7/39 (17.9) | 9/33 (27.3) | 0 |
| Sepsis, n/N (%) | 2/11 (18.2) | 5/39 (12.8) | 6/33 (18.2) | 1/7 (14.3) |
COPD: chronic obstructive pulmonary disease; DVT: deep vein thrombosis; n: number of cases by characteristic; N: total number of events; ND: no data; NYHA: New York Heart Association; PE: pulmonary embolism; SD: standard deviation; VTE: venous thromboembolism.
Characteristics of treatment by type of thromboembolic event.
| Characteristic | Fatal PE | Non-fatal PE | DVT | Other VTE |
|---|---|---|---|---|
| (N=11) | (N=39) | (N=33) | (N=7) | |
| Type of anesthesia | ||||
| General, n/N (%) | 10/11 (90.9) | 33/39 (84.6) | 27/33 (81.8) | 7/7 (100) |
| Neuraxial, n/N (%) | 1/11 (9.1) | 5/39 (12.8) | 2/33 (6.1) | 0 |
| General + neuraxial, n/N (%) | 0 | 0 | 3/33 (9.1) | 0 |
| Other, n/N (%) | 0 | 1/39 (2.6) | 1/33 (3.0) | 0 |
| Central venous catheter | ||||
| Internal jugular, n/N (%) | 2/11 (18.2) | 2/39 (5.1) | 5/33 (15.2) | 3/7 (42.8) |
| Subclavian, n/N (%) | 6/11 (54.5) | 3/39 (7.7) | 3/33 (9.1) | 0 |
| Postoperative immobility >2 days, n/N (%) | 7/11 (63.6) | 9/39 (23.1) | 15/33 (45.5) | 3/7 (42.8) |
| Postoperative thromboprophylaxis | ||||
| Enoxaparin dose: prophylactic or more, n/N (%) | 4/11 (36.4) | 13/39 (33.3) | 14/33 (42.4) | 2/7 (28.6) |
| Enoxaparin dose: less than prophylactic, n/N (%) | 0 | 6/39 (15.4) | 0 | 0 |
| Unfractionated heparin | 0 | 1/39 (2.6) | 0 | 0 |
| Cases with no information available | 1 | 6 | 4 | 2 |
DVT: deep vein thrombosis; n: number of cases by characteristic; N: total number of events; PE: pulmonary embolism; VTE: venous thromboembolism.
Immobility for more than two days was associated with a greater number of severe events (Table 3).
At least 37.7% of patients with events received a prophylactic dose of injectable anticoagulant postoperatively (Table 3).
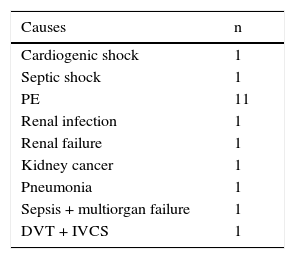
Nineteen patients with VTE died. Possible causes are shown in Table 4.
Causes associated with mortality in patients with venous thromboembolism.
| Causes | n |
|---|---|
| Cardiogenic shock | 1 |
| Septic shock | 1 |
| PE | 11 |
| Renal infection | 1 |
| Renal failure | 1 |
| Kidney cancer | 1 |
| Pneumonia | 1 |
| Sepsis + multiorgan failure | 1 |
| DVT + IVCS | 1 |
DVT: deep vein thrombosis; IVCS: inferior vena cava syndrome; PE: pulmonary embolism.
Overall mortality due to VTE events was 21.1% (95% CI: 13.6-30.4).
DiscussionThe TREVO study included elective and urgent surgical patients from eight specialties. The incidence of VTE (as indicated by in-hospital outcome) was estimated at 1.33/1000 admissions. This figure is extremely low compared to the risk attributed to the Portuguese surgical population in the ENDORSE study (69%).6,10 However, the latter assessed risk factors rather than outcome and only in acute patients undergoing general surgery or urogynecological or ortho trauma surgery, which carry a higher risk of VTE. Bilimoria et al. reported a risk of 5.35/1000 in a multicenter study in the US assessing outcomes in patients undergoing orthopedic, neurological, cardiothoracic, urological and general surgery.8 The authors highlight the fact that surveillance bias is a major factor influencing results, especially when local protocols are more interventionist in requesting imaging exams. Some events may have only mild symptoms that are disregarded in centers where standard diagnostic imaging is guided by symptoms, while in others, such as trauma centers, imaging studies are performed as routine.8
The incidence of VTE in this study reflects our institutional protocol for thromboprophylaxis, which decreases the incidence of VTE by 50-75%.9 In addition, symptomatic VTE, the outcome considered, accounts for only around 50% of all VTE events.3 Even so, the TREVO study shows lower rates than reported in the literature, which may be related to exclusion of cases for inconsistencies in medical records or less precise diagnosis and/or recording. The latter would explain the high mortality, since recording of fatal events is necessarily stricter; the literature shows a lower incidence of PE than of other VTE, unlike in our study, which raises the possibility that VTE other than PE was underdiagnosed. On the other hand, the lower incidence may reflect more effective thromboprophylaxis.
In the TREVO study, the specialty with the highest risk of VTE was neurosurgery, while in the literature4,10–13 it is orthopedic surgery. In a retrospective study of 94 cases of in-hospital VTE, Wang et al. identified cranial surgery as an independent predictor of VTE, with a particularly high odds ratio of 16.1.9 In an earlier study, Hamilton et al. observed that half of neurosurgical patients presented detectable VTE on screening, while only 5% developed symptomatic VTE.14 A known risk factor for VTE that may account for this finding is the fact that cranial surgery entails central venous catheterization in a high proportion of cases, and a retrospective study found that central venous catheterization doubled the risk of in-hospital VTE.15 Furthermore, many of these patients are hospitalized in intensive care units and have longer operating times and hospital stays, which are additional risk factors for VTE. Limitations on the use of pharmacological thrombophylaxis in neurosurgery, irrespective of patient characteristics, may also help explain the increased risk observed. This further highlights the need, already stated in some guidelines,4,5 for mechanical thromboprophylaxis beginning in the preoperative period in neurosurgical patients as well as pharmacological thromboprophylaxis in those at increased risk of VTE.
The aim of the TREVO study was to estimate the risk of in-hospital VTE. While the high risk of VTE in major orthopedic surgery is well known, symptomatic postoperative event rates up to discharge do not reflect overall risk, since mean time to symptomatic events is 17 days in the case of hip arthroplasty and seven days in the case of knee arthroplasty, the high-risk period extending to 12 weeks for the former and six weeks for the latter.1,13 With enhanced recovery programs becoming increasingly common, such patients are now discharged long before the periods referred to above, which introduces even more bias into recorded in-hospital events as a measure of risk and may explain why orthopedic surgery occupied fifth place (1.09/1000 episodes) in the TREVO study.
The risk associated with urological procedures (1.55/1000) was the second highest in our study. Although risk in this patient group has been less studied, a recent cohort study reported moderate to high VTE event rates for total (3.96%) and partial cystectomy (2.35%), followed by radical open nephrectomy (1.67%).16 Other studies have reported a high risk of VTE in renal transplant recipients (7.9-9.1%).17,18 The TREVO study population included patients in a renal transplantation unit, which would have contributed to the high values observed. Beyer et al. reported a high incidence of PE (5.8%) in prostatectomy,19 another common procedure in the population studied.
The year-on-year trend for declining overall VTE rates between 2008 and 2012 supports the hypothesis of progressively more effective thromboprophylaxis.
Overall mortality due to VTE events (21.1%) was higher than reported in the literature and close to mortality due to PE (22.0%), which was also high. Reis reports early VTE mortality of 12.6%.2 Data from the Nationwide Inpatient Sample in the US indicate in-hospital mortality from PE of 12.3% to 8.2%, with a falling trend over the years.20 A Norwegian study reported 30-day mortality of 9.7% from PE and 4.6% from DVT.21 Comparison of the mortality observed in the TREVO study with the above findings supports the idea that non-fatal events are underdiagnosed.
Neuraxial anesthesia was used in 12.2% of procedures in this study. In a meta-analysis, Rodgers et al. showed that epidural anesthesia dramatically reduces risk for VTE, by 44% for DVT and by 55% for PE.22 Another meta-analysis confirmed the benefit of continuous lumbar epidural anesthesia in the postoperative period to reduce the risk of VTE following lower-limb surgery or prostatectomy.23 This may help explain the lower risk found in orthopedic procedures, since neuraxial anesthesia is the most commonly used technique in major lower-limb surgery.
With regard to ASA physical status, most of the study population (55.1%) was classified as ASA III. The literature reports a worsening of VTE risk in hip arthroplasty with progressively higher ASA classification.24
The study has certain limitations. Firstly, it was retrospective and therefore observational and dependent on the information available in medical records. Secondly, cases were excluded for inconsistencies in medical records. Thirdly, there may also have been surveillance bias between departments, which, together with the second limitation, may have contributed to underdiagnosis. Fourthly, it analyzed in-hospital events only, disregarding those that occurred after discharge. Lastly, data on thromboembolic prophylaxis was not available in all cases, particularly preoperative assessment of VTE risk (and indication for prophylaxis in light of the latest evidence) in order to more accurately assess the impact of thromboprophylaxis.
On the positive side, the TREVO study is, as far as we know, the only study on postoperative venous thromboembolism in Portugal apart from the ENDORSE study, which had a much smaller sample; TREVO included 67635 patients, with 90 documented cases of VTE, which is comparable to other international studies. The study was based on outcomes rather than assessment of risk, and care was taken to avoid selection bias, through use of ICD codes and the VTE criteria defined by the Joint Commission International.
ConclusionIn this study, the incidence of symptomatic postoperative VTE was 1.33/1000 admissions. Neurosurgery showed the greatest risk for VTE and PE.
Mortality was 21.1%. Underdiagnosis cannot be excluded, nor can failure to record non-fatal events.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Amaral C, Guimarães Pereira L, Moreto A, Sá AC, Azevedo A. Estudo TRomboEmbolismo Venoso pós-Operatório (TREVO) – risco e mortalidade por especialidade cirúrgica. Rev Port Cardiol. 2017;36:609–616.