Pulmonary embolism (PE) is an entity with high mortality and morbidity, in which risk stratification for adverse events is essential. N-terminal brain natriuretic peptide (NT-proBNP), a right ventricular dysfunction marker, may be useful in assessing the short-term prognosis of patients with PE.
AimsTo characterize a sample of patients hospitalized with PE according to NT-proBNP level at hospital admission and to assess the impact of this biomarker on short-term evolution.
MethodsWe performed a retrospective analysis of consecutive patients admitted with PE over a period of 3.5 years. Based on the median NT-proBNP at hospital admission, patients were divided into two groups (Group 1: NT-proBNP < median and Group 2: NT-proBNP ≥ median). The two groups were compared in terms of demographic characteristics, personal history, clinical presentation, laboratory, electrocardiographic and echocardiographic data, drug therapy, in-hospital course (catecholamine support, invasive ventilation and in-hospital death and the combined endpoint of these events) and 30-day all-cause mortality. A receiver operating characteristic (ROC) curve was constructed to determine the discriminatory power and cut-off value of NT-proBNP for 30-day all-cause mortality.
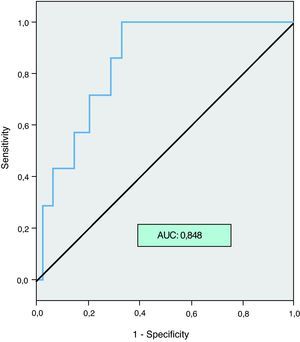
ResultsNinety-one patients, mean age 69±16.4 years (51.6% aged ≥75 years), 53.8% male, were analyzed. Of the total sample, 41.8% had no etiological or predisposing factors for PE and most (84.6%) were stratified as intermediate-risk PE. Median NT-proBNP was 2440pg/ml. Patients in Group 2 were significantly older (74.8±13.2 vs. 62.8±17.2 years, p=0.003) and more had a history of heart failure (35.5% vs. 3.3%, p=0.002) and chronic kidney disease (32.3% vs. 6.7%, p=0.012). They had more tachypnea on initial clinical evaluation (74.2% vs. 44.8, p=0.02), less chest pain (16.1% vs. 46.7%, p=0.01) and higher creatininemia (1.7±0.9 vs. 1.1±0.5mg/dl, p=0.004). Group 2 also more frequently had right chamber dilatation (85.7% vs. 56.7%, p=0.015) and lower left ventricular ejection fraction (56.4±17.6% vs. 66.2±13.5%, p=0.036) on echocardiography. There were no significant differences in drug therapy between the two groups. Regarding the studied endpoints, Group 2 patients needed more catecholamine support (25.8% vs. 6.7%, p=0.044), had higher in-hospital mortality (16.1% vs. 0.0%, p=0.022) and more frequently had the combined endpoint (32.3% vs. 10.0%, p=0.034). All-cause mortality at 30 days was seen only in Group 2 patients (24.1% vs. 0.0%, p=0.034). By ROC curve analysis, NT-proBNP had excellent discriminatory power for this event, with an area under the curve of 0.848. The best NT-proBNP cut-off value was 4740pg/ml.
ConclusionElevated NT-proBNP levels identified PE patients with worse short-term prognosis, and showed excellent power to predict 30-day all-cause mortality. The results of this study may have important clinical implications. The inclusion of NT-proBNP measurement in the initial evaluation of patients with PE can add valuable prognostic information.
O tromboembolismo pulmonar (TEP) é uma entidade responsável por elevada morbi-mortalidade, na qual a estratificação de risco assume um papel fulcral. A porção N-terminal do péptido natriurético tipo B (NT-proBNP), marcador de disfunção ventricular direita, poderá ser um biomarcador útil na avaliação prognóstica a curto-prazo dos doentes com TEP.
ObjectivosCaracterizar uma amostra de doentes internados com TEP agudo de acordo com o valor sérico de NT-proBNP à data da admissão hospitalar e avaliar o impacto deste biomarcador na evolução a curto-prazo.
MetodologiaAnálise retrospectiva de doentes admitidos consecutivamente por TEP, durante 3,5 anos. De acordo com o valor da mediana do NT-proBNP doseado à data da admissão hospitalar, subdividimos os doentes em dois grupos (Grupo 1: NT-proBNP < mediana e Grupo 2: NT-proBNP ≥ mediana). Comparámos os dois grupos quanto às características demográficas, antecedentes pessoais, apresentação clínica, parâmetros analíticos, electrocardiográficos, ecocardiográficos, terapêutica instituída, evolução intrahospitalar (suporte catecolaminérgico, ventilação invasiva, morte intra-hospitalar e o endpoint conjunto destes eventos), bem como a mortalidade por todas as causas aos 30 dias. Construímos uma curva ROC (Receiver Operating Characteristic Curve) para determinar o poder e limiar discriminatório (valor de corte) do NT-proBNP para a ocorrência de morte por todas as causas aos 30 dias após o evento agudo.
ResultadosForam analisados 91 doentes, m=69±16,4 anos (51,6%≥75 anos), 53,8% do género masculino. Da totalidade da amostra, 41,8% não apresentava factores etiológicos/predisponentes para TEP e a maioria, 84,6% dos doentes, estratificava-se em TEP de risco intermédio. A mediana de NT-proBNP sérico foi 2440 pg/ml. Os doentes do Grupo 2 eram significativamente mais velhos (74,8±13,2 versus 62,8±17,2 anos, p=0,003) e tinham mais frequentemente história de insuficiência cardíaca (35,5% versus 3,3%, p=0,002) e de doença renal crónica (32,3% versus 6,7%, p=0,012); na avaliação clínica inicial apresentaram mais polipneia (74,2% versus 44,8, p=0,02), menos frequentemente dor torácica (16,1% versus 46,7%, p=0,01) e valores mais elevados de creatininemia (1,7±0,9 vs 1,1±0,5mg/dl, p=0,004). Quanto aos dados ecocardiográficos o Grupo 2 apresentou mais frequentemente dilatação das cavidades direitas (85,7% versus 56,7%, p=0,015) e menor fracção de ejecção ventricular esquerda (56,4±17,6% vs 66,2±13,5%, p=0,036). Os doentes do Grupo 2 necessitaram mais frequentemente suporte catecolaminérgico (25,8% versus 6,7%, p=0,044) e tiveram maior taxa de mortalidade intrahospitalar (16,1% versus 0,0%, p=0,022) e do endpoint conjunto (32,3% vs 10,0%, p=0,034). O evento morte por todas as causas aos 30 dias ocorreu apenas no Grupo 2 (24,1% versus 0,0%, p=0,034). Na análise por curva ROC, o NT-proBNP teve um poder discriminatório excelente para a ocorrência deste evento, com área sob a curva=0,848; o valor de corte do NT-proBNP foi 4740 pg/ml.
ConclusãoNíveis elevados de NT-proBNP identificaram os doentes com TEP e pior evolução a curto-prazo, apresentando uma excelente acuidade para a predição da morte de qualquer causa aos 30 dias. Os resultados deste estudo poderão ter implicações clínicas importantes, porque a incorporação do doseamento do NT-proBNP na avaliação inicial dos doentes com TEP, poderá fornecer informação prognóstica importante.
Diagnosis of pulmonary embolism (PE) is a challenge, being based on clinical suspicion or probability. It has an estimated annual incidence of 1 out of 1000 patients, which increases with age (mean age 62 years) in both sexes.1
PE has high morbidity and mortality, both early and late. Overall mortality is 7–11%, 10% of deaths occurring within an hour of hospital admission; it is 15% at three months and reaches around 50% in patients who present in shock at admission.1–4 Factors contributing to these alarming figures include inadequate primary and secondary prevention, the wide spectrum of clinical presentation and the high rate of recurrence of thromboembolic events.
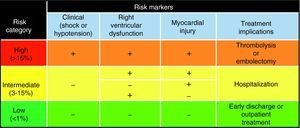
Early diagnosis and risk stratification are thus essential in adjusting therapy to individual patient risk. The European Society of Cardiology (ESC) recommends classifying PE patients into three risk categories (low, intermediate or high), based on clinical criteria (presence or absence of shock and hypotension), biomarkers of myocardial injury (troponins) and echocardiographic evidence of right ventricular (RV) dysfunction (Figure 1).
Risk stratification for early (30-day) mortality in patients with pulmonary embolism.
Patients with high-risk PE present mortality of >15% at 30 days, and are indicated for thrombolysis based on available evidence.5 Those at intermediate risk (hemodynamically stable, with elevated troponin and/or RV dysfunction) include a wide variety of patients with differing forms of clinical presentation and prognosis, for whom early mortality ranges between 3 and 15%.5 In this gray area, thrombolysis has shown no benefit in terms of mortality, although it does appear to improve morbidity and length of hospital stay, and so therapeutic options vary.5 There is an obvious need for more accurate risk stratification, based on clinical and/or laboratory factors that have greater discriminatory power and are thus better predictors of prognosis.
Various biomarkers have been studied in recent years for both diagnosis and stratification of risk and prognosis in PE patients, including natriuretic peptides such as N-terminal brain natriuretic peptide (NT-proBNP) that play an important role in cardiovascular, endocrine and renal homeostasis.6
Initially linked to left ventricular overload and wall stress, particularly in patients with heart failure and left ventricular dysfunction, release of NT-proBNP has since been demonstrated in RV dysfunction,7 and levels of this biomarker in PE correlate with the severity of RV dysfunction, hemodynamic compromise and prognosis.5,8–10 However, the role of NT-proBNP in the management of PE patients is poorly defined and remains the subject of debate.
The aims of this study were to characterize a sample of patients with acute PE according to NT-proBNP level at hospital admission and to assess the impact of this biomarker on short-term evolution.
MethodsWe performed a retrospective analysis of consecutive patients admitted to the coronary care unit between July 2005 and December 2008 with a diagnosis of acute PE (established according to the diagnostic algorithms proposed by the ESC).5 We assessed demographic characteristics, personal history, cardiovascular risk factors, etiological and predisposing factors for PE, form of clinical presentation, serum levels of NT-proBNP, troponin I and creatinine at admission, electrocardiographic alterations (complete or partial right bundle branch block, T-wave inversion in V1-V4 and S1Q3T3 pattern) and transthoracic echocardiographic data (left ventricular ejection fraction [LVEF], right chamber dilatation, pulmonary artery systolic pressure [PASP] and presence of right chamber thrombi), Geneva and Wells scores, and therapy.
Based on the median NT-proBNP (pg/ml) at admission, patients were divided into two groups: Group 1
Statistical analysisThe data were analyzed using SPSS for Windows version 17.0. Categorical variables were expressed as percentages and compared by the chi-square test, while continuous variables were expressed as means ± standard deviation and compared by the Student's t-test when appropriate (normality and homoscedasticity). Results with p<0.05 were considered statistically significant.
ResultsNinety-one patients, mean age 69±16.4 years (51.6% aged ≥75 years), 53.8% male, were analyzed. Of the total sample, 41.8% had no etiological or predisposing factors for PE, 38.5% had transient factors, and 19.8% had cancer. On admission, most patients had intermediate probability of PE according to both the revised Geneva score and the Wells score (65.9% and 72.5%, respectively). Most patients (84.6%) also had intermediate-risk PE according to the ESC guidelines.5 Only 9.9% presented high risk (shock or hypotension) and 5.5% had low risk.
Mean serum troponin I was 0.3μg/l (0.02–1.73), with a median of 0.06μg/l; mean creatininemia was 1.3mg/dl (0.5–5.2), with a median of 1.1mg/dl; and mean NT-proBNP was 7429.9pg/ml (23–57893), with a median of 2440pg/ml.
Those in Group 2 (61 patients), based on median NT-proBNP assessed at admission and before institution of therapy, were significantly older and more had a history of heart failure and chronic kidney disease (Table 1). On initial clinical evaluation, Group 2 patients had more tachypnea, less chest pain and higher creatininemia. On echocardiographic assessment, Group 2 patients also more frequently had right chamber dilatation, lower LVEF, and a tendency for PASP ≥60mmHg (Table 2).
Baseline characteristics of the study population.
| Characteristics | Group 1 | Group 2 | p |
| Male (%) | 56.7 | 54.8 | NS |
| Age, years (mean±SD) | 62.8±17.2 | 74.8±13.2 | 0.003 |
| Hypertension (%) | 73.3 | 58.1 | NS |
| Dyslipidemia (%) | 23.3 | 29.0 | NS |
| Diabetes (%) | 3.3 | 12.9 | NS |
| Current smoking (%) | 16.7 | 16.1 | NS |
| Coronary disease (%) | 16.7 | 22.6 | NS |
| AF (%) | 26.7 | 35.5 | NS |
| HF (%) | 3.3 | 35.5 | 0.002 |
| Stroke (%) | 13.3 | 10.0 | NS |
| COPD (%) | 13.8 | 16.1 | NS |
| CRF (%) | 6.7 | 32.3 | 0.012 |
| Transient factor (%) | 26.7 | 32.3 | NS |
| Bone fracture (%) | 13.3 | 6.5 | NS |
| Major surgery (%) | 3.3 | 0 | NS |
| Major trauma (%) | 0 | 3.3 | NS |
| Venous insufficiency (%) | 26.7 | 19.4 | NS |
| Thrombophilia (%) | 3.3 | 3.2 | NS |
| Bedridden >3 days (%) | 16.7 | 29.0 | NS |
| Oral contraceptives (%) | 0 | 3.2 | NS |
| Cancer (%) | 13.3 | 25.8 | NS |
| No evident factor (%) | 60.0 | 41.9 | NS |
AF: atrial fibrillation; COPD: chronic obstructive pulmonary disease; CRF: chronic renal failure; HF: heart failure; SD: standard deviation.
Clinical assessment and diagnostic exams.
| Characteristics | Group 1 | Group 2 | p |
| Symptoms/signs | |||
| Dyspnea (%) | 83.3 | 87.1 | NS |
| Chest pain (%) | 46.7 | 16.1 | 0.01 |
| Syncope (%) | 13.3 | 6.5 | NS |
| DVT (%) | 16.7 | 12.9 | NS |
| Cough (%) | 6.7 | 6.5 | NS |
| Tachypnea (%) | 44.8 | 74.2 | 0.02 |
| NYHA class≥II (%) | 26.7 | 35.5 | NS |
| Shock (%) | 0 | 6.5 | NS |
| HR, bpm (mean±SD) | 96.9±32.9 | 98.4±32.4 | NS |
| HR>100bpm (%) | 43.3 | 51.6 | NS |
| SBP, mmHg (mean±SD) | 132±25 | 130.7±26.7 | NS |
| SBP≥140mmHg (%) | 44.4 | 48.4 | NS |
| SBP<90mmHg (%) | 0 | 9.7 | NS |
| Laboratory data | |||
| Creatinine, mg/dl (mean±SD) | 1.1±0.5 | 1.7±0.9 | 0.004 |
| Troponin, μg/l (mean±SD) | 0.3±0.4 | 0.3±0.4 | NS |
| D-dimers, ng/ml (mean±SD) | 2.5±1.7 | 3.1±1.7 | NS |
| Electrocardiogram | |||
| T-wave inversion in V1–V4 (%) | 35.7 | 29.0 | NS |
| S1Q3T3 (%) | 17.9 | 12.9 | NS |
| RBBB (%) | 10.7 | 16.1 | NS |
| Echocardiogram | |||
| Right chamber dilatation (%) | 56.7 | 85.7 | 0.015 |
| PASP, mmHg (mean±SD) | 50.0±22.0 | 56.4±17.2 | NS |
| PASP≥60mmHg (%) | 24.1 | 46.2 | 0.086 |
| Right chamber thrombus (%) | 3.3 | 3.6 | NS |
| LVEF (mean±SD) | 66.2±13.5 | 56.4±17.6 | 0.036 |
| Other exams | |||
| Thoracic CT angiography (%) | 86.2 | 83.3 | NS |
| Lower limb Doppler ultrasound (%) | 66.7 | 48.4 | NS |
CT: computed tomography; DVT: deep vein thrombosis; HR: heart rate; LVEF: left ventricular ejection fraction; NYHA: New York Heart Association; PASP: pulmonary artery systolic pressure; RBBB: right bundle branch block; SBP: systolic blood pressure.
Treatment did not differ significantly between the two groups.
Regarding the studied endpoints, Group 2 patients needed more catecholamine support, more frequently had the combined endpoint and had higher in-hospital and 30-day mortality (Table 3).
Treatment and endpoints analyzed.
| Variables (%) | Group 1 | Group 2 | p |
| Treatment | |||
| Thrombolysis | 13.3 | 12.9 | NS |
| UFH | 26.7 | 12.9 | NS |
| LMWH | 90 | 93.5 | NS |
| Endpoints | |||
| Invasive ventilation | 10.0 | 12.9 | NS |
| Catecholamines | 6.7 | 25.8 | 0.044 |
| In-hospital mortality | 0 | 16.1 | 0.022 |
| Combined endpoint | 10.0 | 32.3 | 0.034 |
| 30-Day mortality | 0.0 | 24.1 | 0.006 |
LMWH: low molecular weight heparin; UFH: unfractionated heparin.
By ROC curve analysis, NT-proBNP had excellent discriminatory power for 30-day all-cause mortality, with an area under the curve (AUC) of 0.848, p=0.003 (Figure 2). The best NT-proBNP cut-off value was 4740pg/ml.
DiscussionIn this study, elevated NT-proBNP levels at admission in patients with PE correlated significantly with worse in-hospital evolution and worse prognosis at three months.
These results corroborate those of other published studies that have demonstrated a lower rate of in-hospital complications and better short-term prognosis in PE patients with low NT-proBNP levels.10–12
Most of the study population presented intermediate-risk PE, the gray area in which there is uncertainty regarding therapeutic approach and aggressiveness of therapy. It is probably in this large patient group that biomarkers such as NT-proBNP will prove most useful by enabling more accurate risk stratification and guiding therapeutic decisions.
The short-term prognosis of patients with PE depends mainly on their hemodynamic status at admission and underlying conditions. Many factors besides natriuretic peptides have been shown to have prognostic value in the short term, including echocardiographic criteria of overload and RV dysfunction, as well as clinical parameters.13
In our study, Group 2 patients, with NT-proBNP ≥ median, also had significantly more heart failure and chronic kidney disease and were older, variables that have been shown to be associated with elevated NT-proBNP. This group also showed a greater incidence of tachypnea and had higher creatininemia on initial assessment.
There is debate regarding the biomarkers that should be measured. In a study comparing various biomarkers (NT-proBNP, troponin I, myoglobin, D-dimers and heart-type fatty acid-binding protein) in patients classified with non-massive PE, NT-proBNP was the best predictor of adverse events at three months.14
A recent meta-analysis of 32 studies, including 1127 patients with PE, again demonstrated the ability of NT-proBNP to predict adverse events, and also concluded that in patients with higher NT-proBNP, concomitant elevation of troponins added prognostic value.15
The inclusion of NT-proBNP with other recommended clinical, laboratory and echocardiographic parameters when evaluating patients with PE may provide valuable additional information for risk stratification and follow-up, with improved sensitivity and positive predictive value for assessment of clinical deterioration and short-term and long-term prognosis.16 Agterof et al. have gone so far as to suggest that PE patients who are hemodynamically stable and with low NT-proBNP levels (<500pg/ml) can be treated as outpatients, with no increase in complications or adverse events, which if confirmed would bring considerable benefits in both clinical and economic terms.17
Besides the importance of the absolute value of NT-proBNP level at admission, Kostrubiec et al. have shown that persistent NT-proBNP elevation 24hours after diagnosis (reduction of <50% from initial values) predicts higher mortality at 30 days.12 Serial measurement of NT-proBNP may thus provide additional prognostic information compared to a single measurement at admission, as well as being an indicator of therapeutic efficacy. In the same study, the clinical efficacy of thrombolysis was associated with a significant reduction in serum levels of this biomarker.12 It should be noted that since the mean half-life of NT-proBNP is 48–72hours, daily measurement of NT-proBNP is not indicated.
However, the results of previous studies are conflicting, probably due to small sample sizes, use of varying NT-proBNP cut-offs, measurement at different stages of presentation and clinical evolution and analysis of different endpoints.
Despite its proven relevance for prognostic assessment, routine NT-proBNP measurement is not a generally accepted strategy for patients with PE.
Study limitationsThe main limitation of this study is its retrospective nature. Data from patient assessment at hospital admission are often subjective and not recorded systematically. Analysis of echocardiographic data obtained in the emergency department also showed inconsistencies. A further limitation was the small sample size. Although PE is a common pathology, it remains underdiagnosed and is often a diagnosis of exclusion, which may mean that many of the recommended diagnostic exams are not performed during initial patient assessment. Furthermore, in-patients diagnosed with PE were not included, which means that an important group was excluded from the study.
ConclusionsThis work corroborates data from previous studies and meta-analyses that point to a potentially important role for NT-proBNP as an indicator of short-term prognosis in patients with PE. Prospective multicenter studies are essential to determine conclusively this biomarker's prognostic impact.
To summarize, it can be concluded that measurement of NT-proBNP at hospital admission of patients with suspected PE could be a useful parameter to monitor in-hospital evolution and to assess short-term prognosis.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Dores, H. NT-proBNP na estratificação de risco no tromboembolismo pulmonar. doi 10.1016/j.repc.2011.10.002.