Isolated pulmonary valve endocarditis is a very rare entity, usually associated with intravenous drug abuse. We describe a case of isolated pulmonary valve endocarditis in a diabetic patient with no apparent precipitating factors besides a lesion on the right hallux. The clinical course was favorable and he was discharged home after a six-week course of antibiotic therapy.
A endocardite isolada da válvula pulmonar é uma patologia extremamente rara, estando mais comummente associada ao consumo de drogas por via intravenosa. Descrevemos um caso de endocardite isolada da válvula pulmonar num doente diabético cujo único factor de risco identificado era uma lesão no hálux direito. A evolução foi favorável e o doente teve alta clínica após Seis semanas de antibioterapia.
Infective endocarditis (IE) involving the right heart valves accounts for 6% of patients with IE. The typical site of infection is the tricuspid valve (TV), either in isolation or accompanied by pulmonary valve (PV) involvement.1 Isolated pulmonary valve endocarditis is very rare, affecting less than 1.5% of patients suffering from IE2: the literature includes 36 cases described from 1960 to 19993 and 45 cases between 1960 and 2005.4 Risk factors include intravenous drug abuse, alcoholism, sepsis and central venous catheter or pacemaker interventions with subsequent lead infection; in 28% of cases no definite risk factor is found.3–6 When not associated with intravenous drug abuse – in which the most commonly involved agent is Staphylococcus aureus – Streptococcus viridans is the most prevalent pathogen (55-60%).4
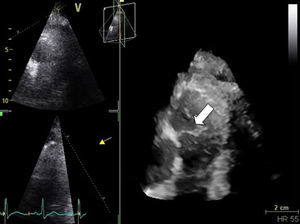
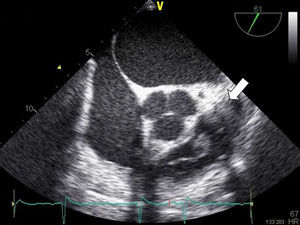
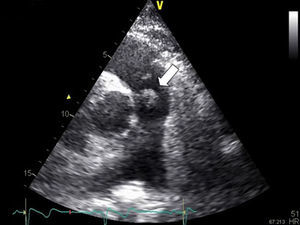
Case reportA 68-year-old man, diabetic with peripheral neuropathy, was admitted to the Internal Medicine ward due to prolonged fever. He reported suffering from both asthenia and fever over the preceding three weeks. He had been given empirical amoxicillin plus clavulanic acid two weeks previously, a treatment that led to transient symptomatic improvement. During initial observation the patient was normotensive with an axillary temperature of 37.6°C. Both cardiac and pulmonary examinations were normal. His right hallux exhibited a lesion, which by his account had been present for the preceding twelve months (Figure 1). Blood tests revealed leukocytosis – 22.70×109/l with 95.8% neutrophils – and elevated CRP (2.14mg/dl). PA chest X-rays were normal. Blood cultures revealed methicillin-susceptible Staphylococcus aureus (MSSA). Transthoracic echocardiography (TTE), and later transesophageal echocardiography (TEE), both revealed a mobile, ovoid, 1-cm diameter mass adhering to the arterial face of the pulmonary valve, and another highly mobile filiform mass also adhering to the PV and protruding into the right ventricle (Figures 2 and 3) without causing any obstruction. Taking into account the antibiotic susceptibility test results, the prescribed antibiotic therapy consisted of flucloxacillin 1000mg IV every 4h and gentamicin 1mg/kg every 8h for six weeks. The fever began to subside on the eighth day. Control echocardiography during hospitalization showed only mild to moderate pulmonary regurgitation. The patient had no other clinical manifestations or identifiable complications, including thromboembolism. Blood cultures were negative after the antibiotic course was completed. The patient was discharged home after six weeks. Nevertheless, the pre-discharge echocardiogram revealed persistence of the vegetations (Figure 4), which had developed a fibrotic appearance, and persistent mild to moderate pulmonary regurgitation.
In association with TV endocarditis, pulmonary valve IE is a rare entity, but it is even less common when it arises in isolation. It is assumed that its rarity is due to the low pressure gradients within the right heart, the low prevalence of congenital malformations, the lower oxygen content of venous blood and the differences in the covering and vascularization of the right heart endothelium.3 Pulmonary valve IE is more frequent in males carrying the risk factors of intravenous drug abuse, alcoholism, sepsis or infection of central venous catheter or pacemaker leads.3 In the present case, the absence of typical risk factors or structural heart problems increased the difficulty of reaching an accurate diagnosis. However, the patient is diabetic, which is a host risk factor for IE7,8 and S. aureus bacteremia.5,6,8 Diabetes is related to depressed leukocyte chemotaxis, adherence, phagocytosis, intracellular killing, and opsonization, factors that predispose to increased incidence and severity of infections.8 Several studies show that the incidence of S. aureus IE is rising5,6; there is an increasing number of patients at risk for IE – due to ageing populations and increasing use of prosthetic cardiac devices – and of those at risk for S. aureus bacteremia, due to comorbidities such as diabetes, hemodialysis and immunosupression.5,6 In this case the presence of a chronic diabetic ulcer on the right foot and the absence of other identifiable risk factors led us to believe that this might constitute the etiologic source of S. aureus bacteremia.9 The management and prognosis of this rare entity are determined by early diagnostic suspicion.2 Due to the low sensitivity of TTE for evaluating the PV (vegetations are only identified by TTE in 70% of cases), TEE is the next step in diagnostic workup. Right-side S. aureus IE typically has a favorable prognosis with medical therapy alone; by contrast, left-side S. aureus IE has high morbidity and mortality.6 There is no difference between diabetic and non-diabetic patients with IE with respect to complications such as embolism, congestive heart failure, valvular vegetation, new valvular regurgitation, or intracardiac abscess, but the former are less likely to undergo surgery for the index IE episode. This may be explained by their worse clinical profile rather than by their having less indications for surgery.8 Indications for surgery are abscess formation, progressive valve destruction and incompetence, persistent bacteremia despite antimicrobial therapy and relapsing infection after completion of a full course of antibiotics.10 In this case the evolution was favorable, without complications. However, current evidence shows that diabetic patients have higher overall in-hospital mortality and diabetes is an independent predictor of IE mortality, especially in male patients.8
This case is notable not only due to the rarity of isolated PV endocarditis but also due to the absence of typical risk factors for IE, and highlights the need for meticulous skin care in diabetic patients.
Conflicts of interestThe authors have no conflicts of interest to declare.