Obese patients are at higher cardiovascular risk in primary prevention. In secondary prevention, an obesity paradox has been reported. We analyzed a cohort of individuals from a previous cross-sectional study on the impact of metabolic syndrome (MS) on coronary artery disease (CAD), aiming to assess the occurrence of cardiovascular events in a long follow-up.
MethodsWe analyzed 296 individuals in a mean follow-up of 6.9±2.2 years. Subjects were divided into four groups according to the presence of MS or CAD (defined as ≥70% coronary stenosis).
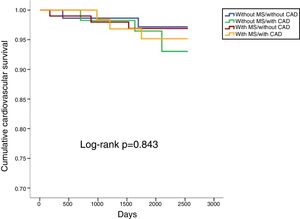
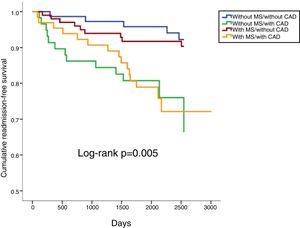
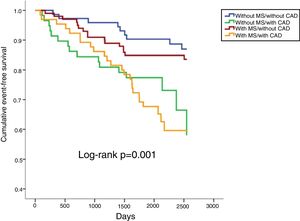
ResultsThe study population had a mean age of 65±9 years at the beginning of the study; 59.5% were male, 55.7% had MS and 41.6% had CAD. During follow-up 10.1% of the population suffered all-cause death, 3.7% cardiovascular death, 14.2% cardiovascular readmission and 22.0% the composite outcome (mortality, acute coronary syndrome, coronary revascularization, stroke/transient ischemic attack or heart failure admission). There were no significant differences in any type of mortality. Patients with CAD had more readmissions and composite outcomes (log-rank p<0.001 and p=0.001, respectively), but there was no difference according to the presence of MS. Only CAD was an independent predictor of cardiovascular admission (HR 3.21, 95% CI 1.66-6.21) and composite outcomes (HR 2.41, 95% CI 1.44-4.02).
ConclusionsIn patients with high cardiovascular risk or established CAD, the presence of MS is not associated with cerebral or cardiac events in long-term follow-up.
Os doentes com obesidade têm um maior risco de eventos cardiovasculares em prevenção primária. Em prevenção secundária tem sido descrito um paradoxo da obesidade. Foi nosso objetivo estudar uma coorte de indivíduos analisados previamente num estudo transversal sobre a relação entre síndrome metabólica (SM) e doença coronária (DC), estudando presentemente o impacto da SM na ocorrência de eventos cardiovasculares a longo-prazo.
MétodosForam analisados 296 indivíduos num seguimento médio de 6,9±2,2 anos. Os indivíduos foram divididos em quatro grupos em função da presença ou ausência de SM e de DC (estenoses coronárias ≥70%).
ResultadosA população analisada tinha uma idade de 65 ± 9 anos no início do estudo, 59,5% do sexo masculino, 55,7% com SM e 41,6% com DC. No seguimento, ocorreram 10,1% de mortes por todas as causas, 3,7% mortes cardiovasculares, 14,2% reinternamentos cardiovasculares e 22,0% de eventos compostos (morte, síndrome coronária aguda, revascularização coronária, acidente vascular cerebral/isquémico transitório, admissão por insuficiência cardíaca). Não se verificaram diferenças significativas em termos de mortalidade. Ambos os grupos com DC tiveram mais reinternamentos e eventos compostos (Log-rank, p<0,001 e p=0,001, respetivamente), mas sem diferenças em relação à presença de SM. A DC foi preditora independente de reinternamento cardiovascular (HR 3,21, IC 95% 1,66–6,21) e de eventos compostos (HR 2,41, IC 95% 1,44–4,02).
ConclusõesEm doentes de elevado risco cardiovascular ou com doença coronária estabelecida, a presença de SM não se associou a aumento de eventos cerebrais ou cardíacos num seguimento a longo-prazo.
Cardiovascular disease (CVD) is still the leading cause of death in Europe in the general population, including Portugal, although its prevalence has fallen in recent decades.1–3 By 2015, cancer had overtaken circulatory system diseases as the leading cause of death in men.3 Besides the well-established cardiovascular risk factors such as hypertension, smoking, diabetes, high low-density lipoprotein cholesterol, age and family history, a number of other risk factors have come under scrutiny in recent years. In particular, the cluster of risk factors known as metabolic syndrome (MS), which has a high prevalence worldwide, reaching almost epidemic proportions, is now a major problem, due to its demonstrated association with the development of type 2 diabetes and CVD, risk for which it increases up to two-fold. MS is particularly challenging to treat because profound changes in lifestyle, which are often difficult to implement in the general population, are needed.4–6
Several meta-analyses have demonstrated a clear association in primary prevention between MS and the occurrence of cardiovascular events during follow-up.4–7 This was also seen in the VALSIM study carried out in a Portuguese population.8 In secondary prevention the results are conflicting, with some studies showing no effect and others a higher incidence of cardiovascular events, but with less than three years of follow-up.9,10
In previous studies we demonstrated that MS by itself is not associated with subclinical atherosclerosis (as assessed by common carotid intima-media thickness), but that the latter is directly associated with some of the components of the syndrome, particularly hyperinsulinemia, hyperglycemia and low high-density lipoprotein (HDL) cholesterol, an indication of the heterogeneous effects of the various components of the entity known as MS.11–13 Similarly, no direct relationship was observed with angiographically significant stable coronary artery disease (CAD), although hyperglycemia and hypertriglyceridemia did predict CAD.14 In both studies, greater waist circumference paradoxically showed a protective effect.12,14
These earlier papers were based on a cross-sectional and observational study. More than five years after that analysis, the aim of the present study was to analyze the same group of patients and to determine in long-term follow-up (over five years) whether MS is associated with higher mortality or a higher incidence of cerebrovascular or cardiovascular events.
MethodsThe original study included adults (age ≥18 years) admitted electively for coronary angiography between 2008 and 2010 with suspected CAD (angina and/or ischemia documented by non-invasive tests). Patients with a history of acute coronary syndrome (ACS), previous myocardial revascularization or known CAD, significant valve disease, congenital heart disease or other cardiomyopathy were excluded. In the original study, the American Heart Association/National Heart, Lung, and Blood Institute's definition of MS was used.15 However, the definition of the syndrome has since been unified by several major medical societies, the main difference being that each country or region can define the limits of abdominal obesity in view of differences between ethnic groups.16 We therefore used the new definition, while retaining the previously defined limits for waist circumference (≥88 cm for women and ≥102 cm for men). The other criteria are blood pressure ≥130/85 mmHg (or under drug treatment), HDL cholesterol ≤40 mg/dl in men or ≤50 mg/dl in women (or under drug treatment), triglycerides ≥150 mg/dl (or under specific treatment), and blood glucose ≥100 mg/dl (or under drug treatment).15,16 MS is defined by the presence of at least three of these criteria. Angiographically significant CAD was defined as the presence of ≥70% stenosis in any coronary vessel.
Follow-up information on all patients was obtained by telephone interview with patients or family members 30 days and one year after admission by a specialist team responsible for follow-up data of patients hospitalized in the department. The same cohort was contacted again in 2017 to obtain additional follow-up information.
The following events were analyzed in follow-up: all-cause mortality (defined as death from any cause); cardiovascular mortality (defined as death associated with CVD); and ACS (defined as the occurrence of angina or angina equivalent at rest with electrocardiographic changes and/or rise or fall in myocardial necrosis markers). When percutaneous coronary intervention (PCI) or coronary artery bypass grafting was performed during follow-up unrelated to the reason for initial admission, myocardial revascularization was included. Admission for heart failure was defined as hospitalization due to the onset or worsening of symptoms or signs of heart failure. Readmission was defined as cardiovascular if the patient had previously been admitted for cardiovascular symptoms, acutely or electively. Stroke/transient ischemic attack (TIA) was defined as the occurrence of new-onset neurological deficit. A composite of cardiac and cerebrovascular events (all-cause mortality, ACS, myocardial revascularization, stroke/TIA or heart failure admission) was also analyzed. The medical records of patients with events was analyzed in order to confirm the event and to classify it correctly, and if necessary further information was requested from the patient. These events were compared among patients with and without CAD and in those with and without MS. The study population was thus divided into four groups.
All subjects provided their written informed consent to take part in the study, which is in accordance with the Declaration of Helsinki.
Statistical analysisContinuous variables are reported as mean and standard deviation. Normality was tested using the Kolmogorov-Smirnov test. Continuous variables were compared using analysis of variance. Categorical variables are expressed as percentages and were compared with the chi-square test or Fisher's test, as appropriate.
Estimates of event-free survival in follow-up were calculated by the Kaplan-Meier method and the curves were compared using the log-rank test. Cox proportional hazards analysis was used to determine the influence of MS and of angiographically significant CAD on the long-term occurrence of events and was adjusted for variables with significant impact on prognosis. Estimates of the association between predictors and events are presented as hazard ratios (HR) with 95% confidence intervals.
IBM SPSS version 19.0.0.2 was used for the statistical analysis. A p-value <0.05 was considered statistically significant.
ResultsThe initial study included 300 patients, four of whom were lost during follow-up. Of the 296 patients included in this analysis, 59% were male, mean age 65±9 years (38-86 years). The prevalence of MS was 55.7% and the most common component of MS was hypertension, followed by abdominal obesity, high blood glucose, low HDL cholesterol and high triglycerides (Table 1). Angiographically significant CAD was detected in only 41.6% of subjects.
Demographic and clinical characteristics of the study population.
| Without MS/without CAD (n=73) | Without MS/with CAD (n=58) | With MS/without CAD (n=100) | With MS/with CAD (n=65) | Total (n=296) | p | |
|---|---|---|---|---|---|---|
| Age, years | 63±10 | 64±9 | 64±9 | 67±8 | 64±9 | 0.063 |
| Male, % | 54.8 | 91.4 | 42.0 | 63.1 | 59.6 | <0.001 |
| BMI (kg/m2) | 27.0±3.6 | 25.3±2.3 | 30.3±4.3 | 29.6±4.1 | 28.1±4.0 | <0.001 |
| Risk factors, % | ||||||
| Hypertension | 72.6 | 81.0 | 92.0 | 95.4 | 85.8 | <0.001 |
| Smoking | 8.2 | 19.0 | 2.0 | 12.3 | 9.1 | 0.003 |
| Dyslipidemia | 58.9 | 72.4 | 75.0 | 72.3 | 69.9 | 0.122 |
| Diabetes | 11.0 | 24.1 | 22.0 | 30.8 | 21.6 | 0.040 |
| MS components, % | ||||||
| Hypertension | 72.6 | 81.0 | 92.0 | 95.4 | 85.8 | <0.001 |
| High blood glucose | 27.4 | 39.7 | 64.0 | 81.5 | 54.1 | <0.001 |
| High triglycerides | 1.4 | 13.8 | 28.0 | 43.1 | 22.0 | <0.001 |
| Low HDL | 15.1 | 19.0 | 71.0 | 78.5 | 48.6 | <0.001 |
| High WC | 35.6 | 10.3 | 91.0 | 75.4 | 58.1 | <0.001 |
| Multivessel disease, % | 0 | 43.1 | 0 | 40.0 | 7.4 | <0.001 |
| Revascularization, % | 0 | 81.0 | 0 | 70.8 | 31.8 | <0.001 |
BMI: body mass index; CAD: coronary artery disease; MS: metabolic syndrome; WC: waist circumference.
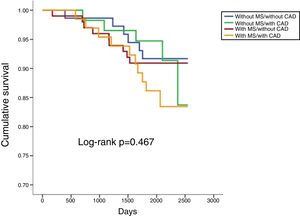
In a mean follow-up of 6.9±2.2 years, 10.1% of the population suffered all-cause death, 3.7% cardiovascular death, 14.2% cardiovascular readmission and 22.0% composite outcomes (Table 2). There were no statistically significant differences between any of the four groups in terms of all-cause or cardiovascular mortality (Table 2; Figures 1 and 2). However, cardiovascular readmissions and composite outcomes were more frequent in the CAD groups (Table 2; Figures 3 and 4). This difference was largely due to a higher incidence of ACS in the group with MS and CAD (Table 2). Both CAD groups presented more frequent PCI and cardiovascular readmission (Table 2), and CAD was associated with more events. Cardiovascular readmissions and composite outcomes were significantly more frequent in patients with CAD both in subjects without MS (log-rank p=0.001 and p=0.004, respectively) and in those with MS (log-rank p=0.007 and p=0.002, respectively). In patients with CAD, the concomitant presence of MS was associated with a tendency for higher all-cause mortality (log-rank p=0.382) and more composite outcomes (log-rank p=0.365) (Figures 1 and 4). There was also a higher incidence of ACS, although without reaching statistical significance (log-rank p=0.094) but with a clear tendency for more events. The groups with MS had fewer admissions for heart failure. The incidence of cancer was similar in the presence or absence of MS.
Events in follow-up.
| (%) | Without MS/without CAD (n=73) | Without MS/with CAD (n=58) | With MS/without CAD (n=100) | With MS/with CAD (n=65) | Total (n=296) | p |
|---|---|---|---|---|---|---|
| All-cause mortalitya | 8.2 | 8.6 | 9.0 | 15.4 | 10.1 | 0.467 |
| Composite outcomesb | 12.3 | 27.6 | 16.0 | 36.9 | 22.0 | 0.001 |
| Cardiovascular mortality | 2.7 | 5.2 | 3.0 | 4.6 | 3.7 | 0.843 |
| ACSc | 1.4 | 1.7 | 3.0 | 10.8 | 4.1 | 0.019 |
| PCI | 1.4 | 12.1 | 1.0 | 13.9 | 6.1 | <0.001 |
| CABG | 0 | 3.4 | 0 | 0 | 0.7 | 0.041 |
| Stroke/TIA | 2.7 | 0 | 3.0 | 3.1 | 2.4 | 0.622 |
| Cardiovascular admission | 6.8 | 22.4 | 9.0 | 23.1 | 14.2 | 0.005 |
| Heart failure admissiond | 5.5 | 8.6 | 2.0 | 0 | 3.7 | 0.049 |
| Cancere | 11.0 | 5.2 | 14.0 | 12.3 | 11.1 | 0.391 |
ACS: acute coronary syndrome; CABG: coronary artery bypass grafting; CAD: coronary artery disease; MS: metabolic syndrome; PCI: percutaneous coronary intervention; TIA: transient ischemic attack.
Comparisons among patients with CAD in the presence or absence of MS:
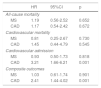
In multivariate analysis, only CAD was an independent predictor of cardiovascular admission and composite outcomes, but it did not predict mortality (Table 3). MS was not an independent predictor of any of the events considered. Age was an independent predictor of all-cause death (HR 1.1, p<0.001), cardiovascular death (HR 1.13, p=0.002), cardiovascular readmission (HR 1.05, p=0.020) and composite outcomes (HR 1.07, p<0.001). Diabetes was an independent predictor of all-cause death (HR 3.11, p=0.004) and composite outcomes (HR 1.97, p=0.012).
Cox multivariate analysis of the predictive effect of metabolic syndrome and/or coronary artery disease for the occurrence of events.
| HR | 95%CI | p | |
|---|---|---|---|
| All-cause mortality | |||
| MS | 1.19 | 0.56-2.52 | 0.652 |
| CAD | 1.17 | 0.54-2.42 | 0.672 |
| Cardiovascular mortality | |||
| MS | 0.81 | 0.25-2.67 | 0.730 |
| CAD | 1.45 | 0.44-4.79 | 0.545 |
| Cardiovascular admission | |||
| MS | 0.93 | 0.50-1.73 | 0.818 |
| CAD | 3.21 | 1.66-6.21 | 0.001 |
| Composite outcomes | |||
| MS | 1.03 | 0.61-1.74 | 0.901 |
| CAD | 2.41 | 1.44-4.02 | 0.001 |
Adjusted for age, diabetes, coronary artery disease, and metabolic syndrome.
CAD: coronary artery disease; CI: confidence interval; HR: hazard ratio; MS: metabolic syndrome
The association between MS and cardiovascular events has been demonstrated in meta-analyses, mostly including patients in primary prevention.4–7 This association remains even after adjustment for other risk factors, proving that the increased risk is real and of epidemiological importance. The presence of MS doubles the risk of CVD, cardiovascular mortality, myocardial infarction and stroke, and increases overall mortality by 50%.6 The risk for cardiovascular events in MS is thus greater than for overall mortality. Even in the absence of diabetes, MS is associated with a higher risk of cardiovascular mortality, myocardial infarction and stroke, although not significantly higher for overall mortality.6
In the VALSIM study, MS was independently associated with CAD (defined as angina and/or history of myocardial infarction) and even more strongly with diabetes, which confirms its importance in the epidemiology of CVD in Portugal.8 Hypertension was the MS component most strongly associated with the occurrence of CVD, although high blood glucose was also an important factor.
Studies on MS in secondary prevention have shown conflicting results, some demonstrating an association with the occurrence of events and others no effect, but the follow-up in most of these studies was no longer than 36 months.9,10
An intracoronary ultrasound study showed that in subjects with MS there is a high prevalence of plaques with high lipid content that are more likely to become unstable, and that MS is an independent predictor of this type of plaque.17,18 However, more intensive pharmacological therapy in secondary prevention, particularly with statins, is known to reduce events by stabilizing atherosclerotic plaques.
However, MS is a heterogeneous entity that varies according to the particular risk factors analyzed. In the MESYAS study in Spain, the risk of CVD varied depending on the component analyzed, with some MS components in isolation conferring different levels of risk.19 The authors concluded that the risk associated with MS is fully explained by its individual components considered independently. Hypertriglyceridemia was the component that was associated with the greatest risk. By contrast, obesity as assessed by body mass index was not an independent risk factor for CVD, and even appeared to be protective. The cardiovascular overload associated with obesity thus appears to be mainly dependent on other metabolic risk factors such as hyperglycemia, atherogenic dyslipidemia and hypertension. Bearing in mind that MS consists of a cluster of at least three risk factors, there is considerable variation in levels of risk in patients with MS, depending on the diagnostic criteria used. If there is obesity, only two other risk factors are needed. However, in the absence of obesity, three other components are required, which represents much more significant cardiovascular risk. The particular combination of components may therefore influence the risk of developing CAD, especially if they include both high blood glucose and atherogenic dyslipidemia.
Longitudinal studies have found a similar incidence of cardiovascular events in both metabolically benign obese individuals (those without metabolic syndrome or diabetes) and normal weight individuals, in contrast to the high cardiovascular risk of high-risk obese patients with clustering of cardiometabolic risk factors.20 Analysis of data from three large studies (the Framingham Offspring Study, Atherosclerosis Risk In Communities and the Cardiovascular Health Study) showed that the presence of MS components, MS itself or diabetes is associated with a 2-5-fold increase in the risk of coronary events or stroke in a mean follow-up of eight years, even after adjusting for abdominal obesity,21 suggesting that metabolic abnormalities are a considerably stronger predictor of cardiovascular events than abdominal obesity.
In a study by Anderson et al. in patients with established CAD, high blood glucose, but not the presence of MS itself or of the other components of MS, predicted death or myocardial infarction in follow-up.22 Other authors, by contrast, showed that when there is CAD, MS affects mortality and coronary events in the medium and long term.23,24 However, the latter studies were performed on non-contemporary populations (in the 1980s and 1990s), with different therapeutic approaches from those currently used and on ethnically different populations (mostly Japanese), and also used older definitions of MS. More recent studies reveal that the controversy over the influence of MS on the occurrence of events continues.9,10
In the present study, in which the treatment of CAD reflects contemporary methods, we demonstrated that MS in patients with CAD does not affect cardiovascular mortality or cardiovascular readmission. However, clear trends are apparent toward higher frequency of the composite outcomes and ACS in follow-up and fewer heart failure admissions. Age and the presence of diabetes are the predictive factors with the greatest impact.
The findings on heart failure were somewhat surprising, but the literature reveals similar examples, particularly in the response to cardiac resynchronization therapy, which is better in individuals with MS.25–28 Firstly, the proportion of women in the groups with MS was greater, and previous studies report that the negative impact of MS on the survival of heart failure patients is seen mainly in men and is not observed in women.28 Secondly, the effect on survival in heart failure is largely due to the presence of diabetes and hypertension and therefore depends on the particular cluster of risk factors found in the individual patient, which varies considerably, as pointed out above.28 Finally, in subjects with heart failure and obesity and/or MS, it is not clear which mechanisms are at play.28 Some authors suggest that the balance between anabolic and catabolic burden is altered in these patients, leading to better prognosis.28 The presence of a condition that counterbalances the effects of inflammation and protein malnutrition, like overweight or moderate obesity, may be beneficial in patients with heart failure. However, the inverse association between obesity or MS and prognosis in HF described by other authors, and also seen in our study, may be the result of bias, since obese patients and/or MS patients represent a selected subgroup of heart failure patients in whom the confounding risk factors associated with worse prognosis may be less represented. In addition, the fact that these patients report symptoms and signs resulting from obesity may lead to earlier cardiac assessment and hence earlier identification of heart failure, followed by more aggressive and timely treatment, and hence better prognosis.28
An important issue is that of the definition of MS, which has varied over the years, not only hampering comparisons between studies, but also with significant implications for estimates of the prevalence of the entity.29 However, the risk of cardiovascular events is similar for all the different definitions, irrespective of the criteria used.29 In 2009, the main medical societies involved in research into MS jointly published the harmonized definition which was used in this study.16
It should also be noted that in our study only 41.6% of the sample had angiographically significant CAD. This finding is in agreement with data from other countries, such as a study based on the US National Cardiovascular Data Registry CathPCI Registry, which includes a large and representative sample of patients without previously known cardiac disease undergoing elective coronary angiography, in which this figure is even lower than in our sample.30 In this study, only 37.6% of those who underwent coronary angiography presented obstructive coronary disease, defined as ≥50% stenosis of the left main coronary artery or ≥70% stenosis of a major epicardial vessel. These results demonstrate the limitations of clinical assessment in general as well as of non-invasive ischemia testing in particular.
Finally, it is noteworthy that there was no apparent association with cancer in MS patients in long-term follow-up, unlike reports in previous studies.
LimitationsA major limitation of the study is that the sample size is relatively small for the follow-up period and the number of events observed was also small, so the study lacked the statistical power to confirm the trends seen in the results presented. This also means that the influence of each MS component on the occurrence of cardiovascular events could not be analyzed in more detail. However, the data presented open the way for more extensive studies.
ConclusionsIn long-term follow-up, the presence of CAD had a strong impact on the occurrence of events, but the presence of MS did not, which calls into question the impact of obesity and of MS in secondary prevention. However, further studies are required on larger populations, with longer follow-up and a larger number of events, in order to obtain more solid conclusions.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Timóteo AT, Mota Carmo M, Soares C, et al. Será a síndrome metabólica um marcador de prognóstico em doentes com elevado risco cardiovascular? Um estudo de coorte a longo-prazo. Rev Port Cardiol. 2019;38:325–332.