Pseudoaneurysms of the ascending aorta are a rare complication of cardiac surgery. However, the poor prognosis associated with this condition if untreated makes early diagnosis and treatment important.
We present the case of a 66-year-old woman who had undergone mitral valvuloplasty 12 days previously, who was admitted with a diagnosis of new-onset atrial fibrillation.
The transthoracic echocardiogram showed a thrombus in the right atrium and anticoagulation was initiated, followed by antibiotic therapy.
After further investigation, the patient was diagnosed with a pseudoaneurysm of the ascending aorta and underwent surgical repair, followed by six weeks of antibiotic therapy.
She was readmitted six months later for an abscess of the lower sternum and mediastinum. After a conservative approach with antibiotics and local drainage failed, recurrence of a large pseudoaneurysm compressing the superior vena cava was documented. A third operation was performed to debride the infected tissue and to place an aortic allograft. There were no postoperative complications.
O pseudoaneunisma da aorta ascendente é uma complicação rara da cirurgia cardíaca. A sua elevada mortalidade torna importante o seu diagnóstico atempado e intervenção precoce.
Os autores apresentam o caso de uma doente do sexo feminino, submetida a valvuloplastia mitral 12 dias antes, internada com o diagnóstico de fibrilhação auricular com resposta ventricular rápida.
O ecocardiograma transtorácico inicial mostrou imagem sugestiva de trombo na aurícula direita, iniciou-se anticoagulação, seguida de terapêutica antibiótica.
Investigação adicional com recurso a TC de tórax com contraste endovenoso permitiu concluir que se tratava de um pseudoaneurisma da aorta ascendente, pelo que a doente foi submetida a correção cirúrgica do mesmo, seguida de seis semanas de terapêutica antibiótica dirigida.
A doente foi reinternada seis meses depois por abcesso na porção inferior do externo e mediastino. Após falha da terapêutica conservadora, com antibiótico e drenagem local, com agravamento clínico da doente, documentou-se reaparecimento de pseudoaneurisma de grandes dimensões com compressão da veia cava superior. Foi então submetida a terceira intervenção cirúrgica com desbridamento do tecido infetado e implantação de homoenxerto aórtico. O pós-operatório decorreu sem intercorrências.
Pseudoaneurysms of the ascending aorta are a rare complication of cardiac surgery. The seriousness of this condition is demonstrated not only by its potentially fatal consequences but also by the complexity and frequent complications of surgical repair.1
The authors present a case that illustrates the diagnostic challenge of aortic pseudoaneurysm in the absence of typical symptoms following a surgical procedure rarely associated with this complication.
Case reportA 66-year-old woman came to the emergency department (ED) due to sudden onset of dizziness, tachycardia and hypotension. She had a history of severe mitral regurgitation and congestive heart failure, and had undergone mitral valve repair with rigid ring annuloplasty and pericardial closure 12 days previously. The immediate postoperative period had been uneventful except for a self-limited episode of atrial fibrillation with rapid ventricular rate, and the patient was discharged on the seventh day after surgery under oral anticoagulation (initiated two days after surgery). Transthoracic echocardiography (TTE) after the operation and chest X-ray at discharge showed no abnormalities.
In the ED, the patient was diagnosed with atrial fibrillation with rapid ventricular rate (120 bpm). She remained asymptomatic, and was medicated with intravenous amiodarone, resulting in conversion to atrial flutter with a ventricular rate of 105 bpm.
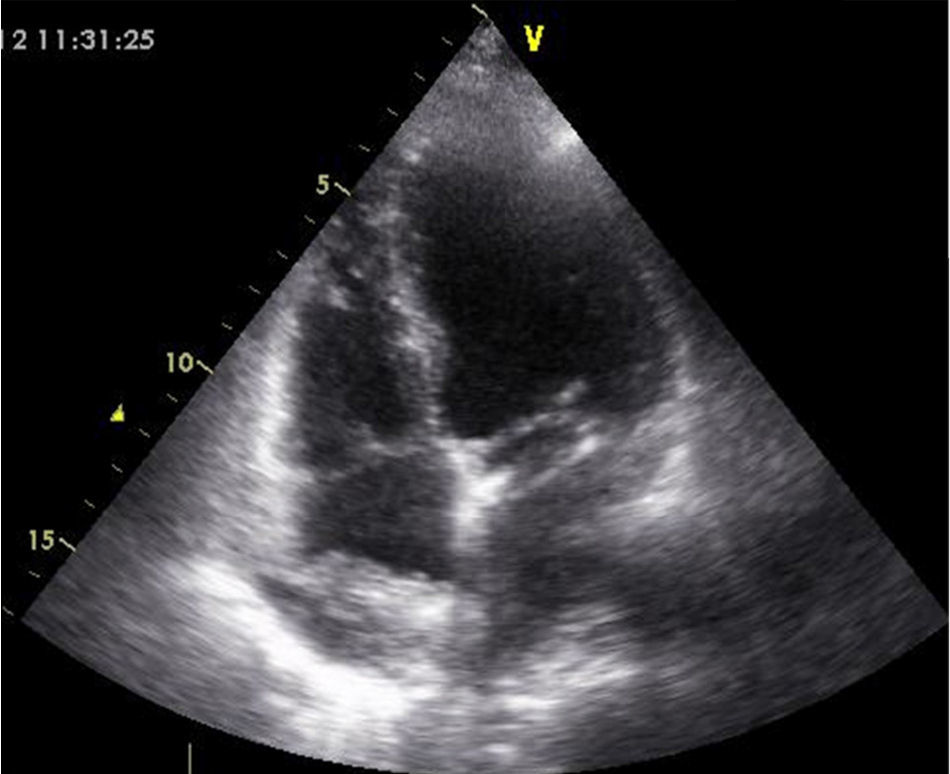
TTE (Figure 1) excluded mitral ring dysfunction or residual regurgitation, and showed good global systolic function; a hyperechogenic image was observed on the right atrial roof measuring 3.3cm×2cm, which was interpreted as a thrombus.
Anticoagulation was initiated with enoxaparin (60 mg twice daily) and the dosage of acenocoumarol was titrated to achieve an INR of 2–3 (INR was below therapeutic levels at admission).
Twelve days later, the patient developed a fever, accompanied by elevation of inflammatory parameters. Following etiological investigation she was medicated with piperacillin–tazobactam on the basis of a presumed diagnosis of mediastinitis.
Serial TTE continued to show similar results, and so thoracic computed tomography (CT) was performed, which revealed a pseudoaneurysm (4.5cm×4.5cm×8cm) on the anterior wall of the ascending aorta, probably originating at the cannulation site (Figure 2).
The patient underwent surgical repair of the pseudoaneurysm with femorofemoral cardiopulmonary bypass (CPB) and cooling to 16°C, followed by median resternotomy. Suture dehiscence was observed at the site of previous aortic cannulation, contained by the pericardium and posterior sternal wall, together with a probable local infectious process. Under circulatory arrest, the pseudoaneurysm was resected and the aorta was closed with a pericardial xenograft.
The postoperative period was again uneventful, inotropic support being discontinued and the patient being extubated 12 hours after the procedure.
Microbiological analysis of the pseudoaneurysm isolated Pseudomonas aeruginosa but all blood cultures before and after the surgical intervention were negative. Intravenous antibiotic therapy was initiated and continued for six weeks, after which the patient was discharged clinically well, with no radiological or echocardiographic abnormalities.
She remained asymptomatic until six months after the second operation, when she was readmitted for osteomyelitis and an abscess of the lower third of the sternum. Thoracic CT with intravenous contrast revealed a heterogeneous collection in the prevascular space, of inflammatory appearance, extending to the anterior chest wall, where a further collection was detected on the anterior sternum. Recurrence of the pseudoaneurysm, although small, was also considered a possibility.
Analysis of the fluid collection again isolated P. aeruginosa, and antibiotic therapy was begun with gentamicin and piperacillin–tazobactam.
Since labeled leukocyte scintigraphy suggested that the infectious process was confined to the distal third of the sternum, a conservative approach with antibiotics and drainage was adopted. The patient developed superior vena cava syndrome, and so CT angiography was repeated; this revealed a giant pseudoaneurysm in the process of rupture but contained by the sternum (Figure 3).
A third operation was performed, again with femorofemoral CPB and hypothermia. Since it was impossible to perform the sternotomy without rupturing the aneurysm, when this occurred, the solution of continuity in the aorta was identified and a 24-mm catheter was introduced toward the descending aorta as an aortic endoclamp to stabilize the patient's circulation. The brachiocephalic trunk and left carotid arteries were then cannulated to ensure continuous cerebral perfusion. Intraoperatively, the pseudoaneurysm was confirmed to be in the process of rupturing, the blood being contained by adherences resulting from the two previous interventions. Access to the cardiac structures was hindered by fibrous tissue composed of adherences and organized hematomas. The infected tissue was debrided and the infected aortic orifice was enlarged, and the entire area was cleaned. This time, the aorta was closed using an allograft over the native vessel.
The postoperative period was uneventful, ventilatory support being withdrawn after three days. A further six-week cycle of antibiotic therapy was begun, resulting in marked improvement in inflammatory parameters. Magnetic resonance imaging was not performed due to artifacts caused by the sutures, but thoracic CT with intravenous contrast showed ascending aortic dilatation (47 mm×49 mm) but no evidence of a solution of continuity or pseudoaneurysm (Figure 4).
The patient remains under medical follow-up, with aortic re-evaluation scheduled in six months, followed by annual imaging assessment.
DiscussionA false aneurysm, or pseudoaneurysm, of the aorta is caused by rupture of at least one layer of the aortic wall, which is surrounded and contained by the remaining aortic walls and adjacent mediastinal structures.2 A rare complication of manipulation of the aorta during surgery (estimated to occur in less than 0.5% of cardiac surgeries), it is a major cause of death and was reported to be responsible for 3% of late mortality in a series of 1000 consecutive coronary artery bypass graft (CABG) procedures.3
Pseudoaneurysms of the ascending aorta normally arise at the site of disruption of the aortic wall resulting from such procedures as aortotomy for aortic valve replacement, proximal anastomosis of venous grafts in CABG, needle puncture for pressure measurement or administration of cardioplegic solutions, or aortic cannulation to institute CPB as in the case presented.3
This complication has accordingly been reported mainly after CABG, aortic valve surgery or surgical procedures involving the ascending aorta such as repair of type A dissection.1,3 Although aortic cannulation for induction of CPB was initially described as the procedure most commonly associated with the development of pseudoaneurysms,3 aortic surgery using conduits appears to be more frequently linked to this complication in more recent series.2,4 It is rare following mitral valve surgery.
Many different forms of clinical presentation have been described, a significant proportion of patients (53%) being asymptomatic,2,4 as initially found in the case presented. As the pseudoaneurysm increases in size, symptoms may appear, mainly due to compression of adjacent structures; these can include chest pain, dyspnea, superior vena cava syndrome or acute coronary syndrome, or the patient may develop low cardiac output and a setting resembling tamponade due to right ventricular compression. It can also manifest as a pulsatile mass or peripheral embolism, aortic regurgitation, mediastinitis or sepsis.1,2,4
Although the etiology of this complication is not fully understood, predisposing factors include surgical repair of native aortic dissection, aortic wall degeneration, aortic cannulation, technical problems with the anastomosis, preoperative hypertension and infection (which may be manifested as postoperative fever with no identifiable focus of infection, mediastinitis, or infection of the surgical wound).1,2,4,5 Most authors report concomitant infection as the main etiological factor,1–3 although the presence of a leak at the site of previous cannulation was also a major factor in one series.4 Both these mechanisms were found in the case presented: a leak played an important role in the first hospitalization, and recurrence of the pseudoaneurysm was probably due to infection which persisted after initial treatment and was responsible for the worsening clinical setting.
As stated above, infection is often associated with this condition, as shown by a review in which it was present or suspected in 18 of 31 cases of ascending aorta pseudoaneurysm.2 Various microorganisms have been implicated, including P. aeruginosa. There have been other reports of bacterial agents being isolated from a pseudoaneurysm but with consistently negative blood cultures, as in our patient.1
This case illustrates the importance of multiple cardiac imaging techniques for diagnosis. CT played a central role in establishing the diagnosis, characterizing the pseudoaneurysm and determining its point of origin. CT and aortography are considered the best imaging techniques in this context, not only to confirm the diagnosis but also to characterize the pseudoaneurysm before surgery, thus aiding surgical planning.2
There have been advances in the management of this condition, particularly endovascular treatment, but this is limited by anatomical features and is reserved for small, non-infected pseudoaneurysms.5 Surgical treatment, with CPB via the femoral veins (as in the case presented) or a combination of the subclavian artery and the femoral veins, followed by hypothermia with low cardiac output or circulatory arrest prior to sternotomy, is considered the best approach in most cases.2,4–6
Allografts or Dacron conduits should be used for surgical repair, as this is the most common technique in the literature, used in 70% of cases and recommended by the respective authors.1,2,4 It is particularly suitable for large pseudoaneurysms and those associated with infection. Local repair using a pericardial patch can be performed for smaller defects or those with localized infection after thorough debridement of infected tissue, although this technique is associated with a higher risk of recurrence, particularly in cases of infected pseudoaneurysms,1,2,4 as illustrated by the case presented above. Irrespective of the surgical technique chosen, the procedure should be followed by six weeks of systemic antibiotic therapy, or even longer if conduits are used.1,2
Most studies published on this condition are case reports or small series, and so the mortality associated with surgical repair is difficult to determine; while some older series report in-hospital mortality between 14.2% and 46%,3,5 more recent series report 6.7–6.9%.2,4 Pseudoaneurysms more than 55 mm in diameter, emergency surgery and sepsis during surgery are associated with worse outcomes.5,6 Survival at one year after hospital discharge is over 90%, and freedom from reoperation is around 70% at five and 10 years.2,4
Some authors advocate annual follow-up with contrast-enhanced thoracic CT for patients who have undergone aortic surgery with a view to early detection of this complication, thus enabling surgical repair in optimal conditions and a better prognosis.2
In conclusion, pseudoaneurysms of the ascending aorta are a rare but serious complication of cardiothoracic surgery and are associated with high mortality. Prompt diagnosis by appropriate imaging techniques, enabling surgical treatment to be performed on a non-emergency basis and in optimal conditions, is an important factor in the prognosis of these patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe author has no conflicts of interest to declare.
Please cite this article as: Almeida S, Bico P, Almeida AR, Laranjeira Santos Á, Banazol N, Fragata J, et al. Pseudoaneurisma iatrogénico da aorta ascendente: uma complicação esquecida. Rev Port Cardiol. 2014;33:113.e1-113.e5.