The authors describe the case of a renal transplant patient who developed late infective endocarditis associated with an intracardiac fragment of a catheter inserted 16 years before. Clinical presentation was anemia of undetermined cause and weight loss. Three blood cultures were positive for Burkholderia cepacia. Transesophageal echocardiography revealed a foreign body in the right atrium and right ventricle, confirmed by computed tomography. The patient underwent intravenous antibiotic therapy, followed by cardiac surgery to remove the foreign body. There were no postoperative complications, with improvement of anemia and stabilization of renal function.
Os autores descrevem o caso de paciente com transplante renal que desenvolveu endocardite infecciosa tardiamente associada com fragmento de cateter intracardíaco implantado 16 anos antes. A apresentação clínica foi anemia de causa indeterminada e perda de peso. Três hemoculturas foram positivas para Burkholderia cepacia. O ecocardiograma transesofágico revelou um corpo estranho no átrio e ventrículo direitos, que foi confirmado por tomografia computadorizada. A paciente foi submetida a antibioticoterapia intravenosa e posterior cirurgia cardíaca, com remoção do corpo estranho. Evoluiu sem complicações pós‐operatórias, com correção da anemia e estabilização da função renal.
Peripherally inserted central catheters (PICCs) are used in clinical practice for administration of fluids or drugs that cannot be administered via the peripheral veins and are generally safe.1 However, catheter fragments that enter the circulation can cause embolisms, the most frequently affected locations being the right atrium, the superior vena cava and the left pulmonary artery.1,2 There is one report of an intracardiac foreign body that remained in place for 17 years without causing complications,3 but such material should be removed as soon as possible to avoid the risk of arrhythmias, myocardial perforation, septicemia or endocarditis.1–4 Infective endocarditis is relatively uncommon in the general population, although its incidence is increasing in patients with PICCs; in‐hospital mortality ranges from 9.6% to 26%.5Burkholderia cepacia (formerly Pseudomonas cepacia) belongs to the B. cepacia complex, which is currently divided into 10 genomic species.6 It rarely causes endocarditis in the absence of predisposing conditions, which include immunodeficiency, intravenous drug use, prosthetic valves and indwelling catheters.5,6 It can contaminate water supplies and disinfectant, antiseptic and anesthetic solutions, as well as intravenous fluids.6
The aim of this case report is to raise the index of suspicion regarding this rarely described condition.
Case reportA 40‐year‐old white woman was admitted for general malaise, anorexia, and weight loss (5 kg in two months), together with stomach pain and postprandial vomiting that had begun the day before. Her daily medication included immunosuppressants (azathioprine 100 mg, tacrolimus 4 mg and prednisone 5 mg) and antihypertensives (atenolol 100 mg and clonidine 0.4 mg).
At the age of 24, she had been diagnosed with hypertension and stage 5 chronic renal disease of undetermined cause, and chronic hemodialysis was begun. Four months later she became pregnant, and a cesarean section was performed in the eighth gestational month due to severe preeclampsia. In the postpartum period, she suffered severe gynecological bleeding, septicemia and shock. She remained in the intensive care unit for 15 days, with a PICC. Following progressive improvement in her clinical condition, the patient returned to her regular hemodialysis program.
Eight years later, the patient underwent renal transplant from a cadaver donor, but developed acute steroid‐resistant rejection, which was treated with OKT3. She was discharged 30 days after transplantation, clinically well, with creatinine stabilized at 2.0 mg/dl. Her renal function remained normal during outpatient follow‐up, but she developed late complications (under treatment for herpetic eye infection for the last seven years and for thrombophlebitis of the arteriovenous fistula for the last three years). No other PICC was inserted during the transplant procedure or in the immediate or late postoperative period.
On admission, the patient was in reasonable general health, pale and apyretic, with a body weight of 65.5 kg. Pulmonary auscultation revealed no abnormalities; her blood pressure was 110/60 mmHg and heart rate 108 bpm, with normal regular heart sounds and a faint non‐radiating systolic murmur in the right parasternal region. There was no palpable visceromegaly, and the extremities were well perfused, with no edema. Initial laboratory tests showed low hemoglobin, unexplained by gastrointestinal or gynecological blood loss, hematocrit 22%, hemoglobin 7 g/dl, mean corpuscular volume 93 fl, mean corpuscular hemoglobin concentration 32%, white cell count 2.7×103/mm3 (neutrophils 64%, eosinophils 3%, lymphocytes 24%, monocytes 8%) and platelet count 238×103/mm3. Creatinine (2.1 mg/dl) and urea (73 mg/dl) were elevated, with normal electrolyte levels; C‐reactive protein (6.8 mg/dl) and ferritin (1043 μg/l) were also elevated. Prothrombin time (13.4 s), prothrombin activity (81.9%) and INR (1.14) were normal. Urine analysis showed no significant alterations and urine cultures were negative. Blood cultures (on three samples) identified B. cepacia sensitive to meropenem and trimethoprim (TMP) with sulfamethoxazole (SMZ) only. The latter combination was administered intravenously (TMP 160 mg and SMZ 800 mg every 12 hours).
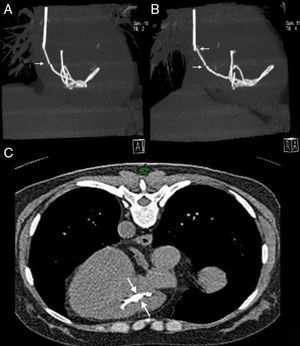
The chest X‐ray was normal, but transesophageal echocardiography revealed the presence of a foreign body in the right atrium and ventricle. Thoracic computed tomography (CT) showed a dense, elongated image extending from the right atrium through the tricuspid valve into the right ventricle, ending in tangled loops within the ventricular cavity (Figure 1A and B). The incorrectly positioned, and probably fragmented, catheter was removed percutaneously. However, control CT showed a dense intracardiac image (Figure 1C); further noninvasive procedures were not attempted, since the fragment appeared to be attached to the chamber wall, the result of the length of time it had been in place, and could have caused embolisms. On the 16th day of antibiotic therapy, cardiotomy confirmed the presence of a catheter fragment firmly attached to the endocardium, which was successfully removed. The postoperative period was uneventful, with normal hemogram and renal function, and the patient was discharged on the 17th postoperative day. Antibiotic therapy was continued orally for a further four weeks, and she remains asymptomatic in outpatient follow‐up consultations.
Thoracic computed tomography. (A) and (B) Dense, elongated image extending from the right atrium to the right ventricle, ending in tangled loops within the ventricular chamber, and apparent fragmentation (arrows); (C) control exam after removal of the catheter, showing what appears to be an intracardiac fragment (arrows).
PICCs are increasingly used in clinical practice, particularly in intensive care units.1,5,6 US health institutions use around 150 million of these devices every year for intravenous administration of fluids, drugs, blood products and parenteral nutrition.5,6 However, various complications have been associated with these devices, particularly infection.1,5,6 PICC rupture is now rare, with an incidence between 0.01% and 1%,2,7,8 although Loughran and Borzatta9 reported a prevalence of 9.7% of such ruptures in a retrospective study in a hospital in California, involving 322 patients with PICCs. Some Brazilian studies indicate complication rates between 4% and 15.4%.1,10–12 Catheter fragmentation and migration to the systemic circulation, followed by embolization, occurs in 0.6% of cases,1 and can cause arterial occlusion, arrhythmias, thrombosis, septicemia, endocarditis or death.1–4 The overall incidence of endocarditis ranges between 2 and 10 cases per 100 000 person‐years,5 with a higher prevalence of Gram‐positive agents when associated with PICCs.6,13 A higher prevalence of Gram‐negative agents and fungi is associated with intravenous drug use and immunodeficiency.13
In the case presented, blood cultures revealed a Gram‐negative bacterium of the Burkholderiaceae family, B. cepacia,6 a major infective agent in patients with cystic fibrosis or chronic granulomatous diseases, but one not usually associated with PICC infection or endocarditis.6,14,15B. cepacia complex can be transmitted between humans, both in and outside the hospital environment,6,16 and contaminated intravenous solutions and drugs are common sources of hospital infection by these bacteria.6 Infection by B. cepacia complex is difficult to control due to its high resistance to most antibiotics.6,14,15 TMP/SMZ is the treatment of choice,6,14 and was successful in the present case.
The clinical consequences of an intracardiac foreign body may be immediate or late, and range from absence of symptoms to severe hemodynamic instability, and it may only be detected as an incidental finding during investigation of other clinical conditions.16 In the case presented, the chest X‐ray did not reveal the presence of an intracardiac foreign body, due to superimposition of images. Transesophageal echocardiography, the diagnostic exam of choice in suspected endocarditis, revealed a metal foreign body in our patient, although the corresponding images were not made available for this case report. Even in asymptomatic patients, the risk of serious complications is an indication for removal of the foreign body in most cases.2 Patients who present with infection, arrhythmia or cerebrovascular events should undergo surgical removal of the foreign body, irrespective of its location.16 Our patient had positive blood cultures, and once the presence of an intracardiac foreign body was confirmed, she underwent cardiotomy and the catheter fragment was successfully removed.
Given this patient's long medical history, the precise mechanism of infection is difficult to determine, but it is noteworthy that the presence of an intracardiac foreign body did not produce clinical complications for many years. The prosthetic material used was not infected prior to implantation, but over time it was colonized by bacteria that entered the circulation. The most likely reason is immunosuppressive therapy, which made the patient more vulnerable to infections.
In the latest hospitalization, there was no delay in diagnosis, since the established protocol for treating renal transplant patients includes investigation of possible infection even in the absence of fever. Such patients may exhibit clinical settings that differ from the traditional pattern, particularly when there is an infection of cardiovascular origin that is not apparent.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Falcão Pedrosa Costa A, Castelo Branco Cavalcanti F, Modesto dos Santos V. Endocardite por Burkholderia cepacia e corpo estranho intracardíaco. Rev Port Cardiol. 2014;33:117.e1–117.e4.