Giant cell arteritis (GCA) is a systemic large vessel vasculitis, with extracranial arterial involvement described in 10–15% of cases, usually affecting the aorta and its branches. Patients with GCA are more likely to develop aortic aneurysms, but these are rarely present at the time of the diagnosis.
We report the case of an 80-year-old Caucasian woman, who reported proximal muscle pain in the arms with morning stiffness of the shoulders for eight months. In the previous two months, she had developed worsening bilateral arm claudication, severe pain, cold extremities and digital necrosis. She had no palpable radial pulses and no measurable blood pressure.
The patient had normochromic anemia, erythrocyte sedimentation rate of 120 mm/h, and a negative infectious and autoimmune workup. Computed tomography angiography revealed concentric wall thickening of the aorta extending to the aortic arch branches, particularly the subclavian and axillary arteries, which were severely stenotic, with areas of bilateral occlusion and an aneurysm of the ascending aorta (47 mm). Despite corticosteroid therapy there was progression to acute critical ischemia. She accordingly underwent surgical revascularization using a bilateral carotid-humeral bypass. After surgery, corticosteroid therapy was maintained and at six-month follow-up she was clinically stable with reduced inflammatory markers.
GCA, usually a chronic benign vasculitis, presented exceptionally in this case as acute critical upper limb ischemia, resulting from a massive inflammatory process of the subclavian and axillary arteries, treated with salvage surgical revascularization.
A arterite de células gigantes (ACG) é uma vasculite de grandes vasos, com envolvimento extracraniano em 10-15% dos casos, afetando preferencialmente a aorta e os seus ramos. Os aneurismas da aorta ascendente são mais frequentes em doentes com ACG, mas são raros no momento do diagnóstico.
Apresentamos o caso de uma doente, caucasiana, com 80 anos de idade, que descrevia dor muscular nos membros superiores, com rigidez matinal dos ombros, desde há oito meses. Nos últimos dois meses referia claudicação intermitente de agravamento progressivo, dor intensa, extremidades frias e o aparecimento de úlceras digitais. Ao exame objetivo não se palpavam pulsos radiais ou cubitais, nem se registavam valores de pressão arterial.
Laboratorialmente, destacava-se anemia normocíticanormocrómica, VS de 120 mm/h e estudo autoimune e infeccioso negativos. A tomografia computorizada com contraste revelou espessamento concêntrico da parede da aorta e dos seus ramos, notoriamente artéria subclávia e axilar, que apresentavam áreas de estenose e oclusão bilaterais e uma dilatação aneurismática da aorta ascendente (47 mm). Apesar da instituição imediata de corticoterapia, verificou-se uma progressão para isquemia crítica aguda dos membros superiores. Consequentemente, foi submetida com sucesso a revascularização cirúrgica através de um bypass carótido-umeral. A doente manteve corticoterapia e ao 6.° mês de follow-up encontrava-se clinicamente estável, com regressão dos parâmetros inflamatórios.
A ACG é habitualmente descrita como uma patologia indolente e benigna. No entanto, apresentou-se neste caso como uma isquemia crítica aguda dos membros superiores, secundária à intensa resposta inflamatória das artérias subclávias e axilares, obrigando à revascularização cirúrgica.
Giant cell arteritis (GCA) is a systemic medium and large vessel vasculitis, with a wide spectrum of presentations, most frequently secondary to involvement of the cranial arteries, the typical symptoms being headache, jaw claudication, visual loss and stroke. Extracranial arterial involvement is described in 10–15% of cases,1,2 usually presenting as upper or lower extremity claudication, and rarely with acute critical ischemia as the primary finding.
We report a severe and sudden case of acute critical ischemia of the arms with digital necrosis as the presenting features of GCA, successfully treated by salvage revascularization surgery. Only large vessels were involved, mainly the subclavian and axillary arteries, with no involvement of the carotid or cranial arteries.
Case reportAn 80-year-old Caucasian woman with a history of hypertension described proximal muscle pain in the arms with morning stiffness of the shoulders and neck, for the past eight months. In the previous two months, she had developed worsening bilateral arm claudication, severe pain with restricted mobility, cold extremities and digital necrosis. She had no palpable radial or cubital pulses and no measurable blood pressure. There were no clinical signs of cranial or lower limb artery involvement and no constitutional symptoms were reported.
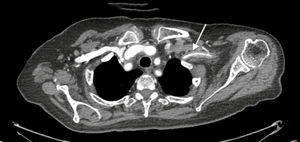
InvestigationThe patient presented normochromic anemia, elevated erythrocyte sedimentation rate (ESR) (120 mm/h) and C-reactive protein (CRP) (123 mg/l), and negative infectious and autoimmune workup. Contrast computed tomography angiography (CTA) in the arterial phase (Figures 1–3) revealed concentric wall thickening of the aorta extending to the aortic arch branches, particularly the subclavian and axillary arteries, which were severely stenotic with areas of bilateral luminal occlusion, and no involvement of the carotid branches; an aneurysm of the ascending aorta 47 mm in diameter was also detected.
The patient immediately started corticosteroid therapy (prednisone 1 mg/kg daily) and aspirin (100 mg daily), but there was incomplete resolution of the symptoms with progression of digital ulceration, necrosis and paresthesia, features of acute critical ischemia. Surgical revascularization using a bilateral carotid-humeral bypass was accordingly performed.
After surgery, corticosteroid therapy was maintained (slowly tapered to 40 mg/day), and at the six-month follow-up appointment, there was no arm claudication and on physical examination there were palpable radial and cubital pulses and systolic blood pressure of 135 mmHg. Laboratory exams revealed a sustained reduction of serum inflammatory markers, and follow-up CTA (Figure 4) showed adequate permeability of the bypassed vessels and stability of the aneurysm. The histological result of the biopsied artery showed a transmural inflammatory infiltrate.
DiscussionGiant cell arteritis is a chronic inflammatory systemic disease, affecting medium and large arteries. The most common symptoms arise from the preferential involvement of the cranial arteries, especially branches of the external carotid such as the temporal or ophthalmic artery.
In 10–15% of patients there is involvement of aortic arch branches, particularly the subclavian and axillary arteries.1,2 This involvement is rarely the presenting feature of the disease, usually resulting from progression or relapse after discontinuation or tapering of corticosteroid therapy.1 One study reported a period of eleven months between diagnosis of temporal artery GCA and the appearance of symptoms resulting from involvement of the upper limb arteries.3 The most common symptom of such involvement is arm claudication and pain (68%), but in rare cases it can evolve into critical ischemia, digital ulceration and gangrene.1
Unlike for temporal artery GCA, there are no validated independent criteria for the diagnosis of GCA with involvement of the upper limb arteries, so this relies on clinical suspicion, supported by laboratory and imaging studies. An ESR of over 50 mm/h was one of the first inflammatory markers associated with the disease, and is part of the American College of Rheumatology criteria for GCA diagnosis (86.5% sensitivity and 47.7% specificity).4 Some studies of GCA with upper or lower limb involvement found lower ESR values compared with temporal artery GCA.1 CRP level was observed to be a more sensitive marker of disease activity, and is especially useful to access disease relapse.2 The European League Against Rheumatism guidelines for the management of GCA recommend a temporal artery biopsy in all patients whenever a diagnosis is suspected (level of evidence 3, strength of recommendation C).5 Nevertheless, Brack et al. reported negative temporal artery biopsy in 42% of patients with large-vessel GCA.6 Assie et al. also observed a lower rate of positive temporal artery biopsy in patients with temporal artery GCA compared to those with involvement of upper and lower limb arteries (69% vs. 95%).7 Biopsy of the affected artery is generally only available if revascularization procedures take place, so the diagnosis and treatment strategy of large-vessel GCA are frequently decided before histological results are available. The biopsy may reveal transmural inflammatory infiltrate with fragmentation of the elastic lamina with or without giant cells in a focal and segmental distribution. False negatives are possible depending on the sample size (ideally 1–2 cm), duration of previous corticosteroid therapy and the presence of skip lesions. CTA is an excellent non-invasive exam to assess vessel wall thickness and regularity, also revealing luminal defects such as stenosis, occlusion, dilation and aneurysms.
As a systemic inflammatory disease the first-line treatment advocated in most guidelines is corticosteroid therapy (1 mg/kg/day, maximum 60 mg daily), with some authors suggesting high-dose methylprednisolone bolus before oral corticosteroid therapy. Nonetheless, there is scant evidence supporting this strategy in GCA patients with upper limb artery involvement. Our patient immediately started prednisone 60 mg/d, and showed a slight clinical improvement within days. However, the bilateral occlusion of both subclavian arteries was remarkably severe, and progression to critical ischemia was inevitable. The vascular surgery team performed a bilateral carotid-humeral bypass as a salvage revascularization procedure to assure blood flow and limb viability. She continued corticosteroid therapy with slow dose tapering. Surgical intervention in such patients is rarely indicated because of the chronic nature of the disease. Nonetheless, when the occlusion is abrupt there is no time to develop collateral circulation to assure tissue viability and the response to corticosteroids can be inadequate, especially in cases of large vessel involvement.8 There are some small series reporting the use of balloon angioplasty as a minimally invasive revascularization procedure, with excellent immediate results but with 50% recurrence of stenosis after a median of five months.9
Follow-up in these patients is mainly based on the response to corticosteroid therapy, as assessed by clinical evolution, reduction in inflammatory markers and, in some cases, imaging studies. A treatment course of one to two years is often required, but some patients have a more chronic or relapsing course of the disease and require longer treatment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.