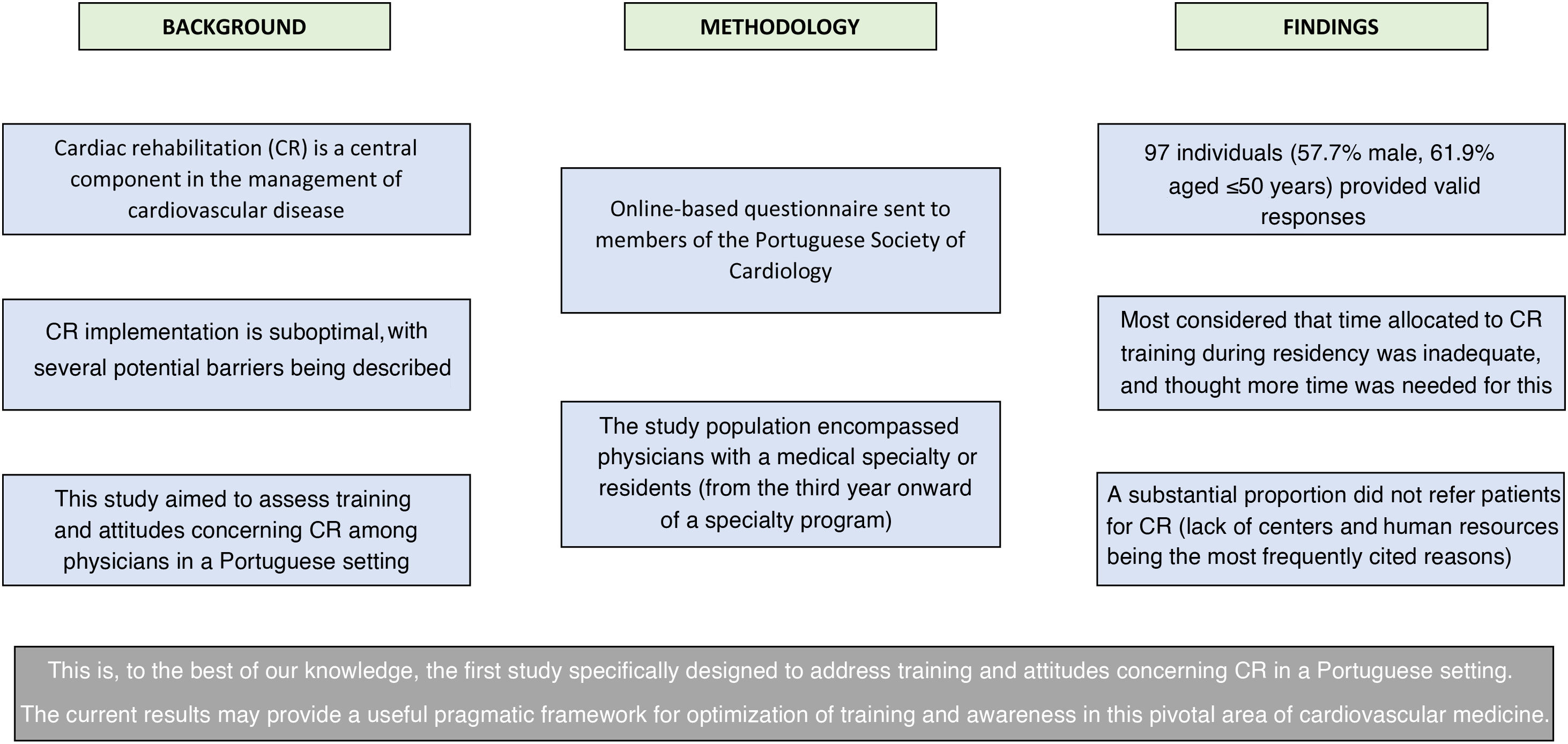
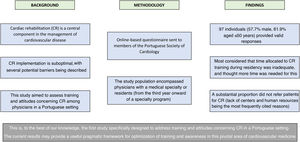
Cardiac rehabilitation (CR) is a central component in the management of cardiovascular disease. While its potential benefits have been extensively explored and confirmed, its implementation is still suboptimal, due to various possible barriers. This study aimed to assess training and attitudes concerning CR among physicians in a Portuguese setting.
MethodsAn online questionnaire structured in three parts (participant characteristics, training and attitudes concerning CR, and a brief general knowledge assessment) was developed and sent to members of the Portuguese Society of Cardiology. The study population encompassed physicians with a medical specialty or residents from the third year onward of a specialty program.
ResultsA total of 97 individuals (57.7% male, 61.9% aged ≤50 years) presented valid answers. CR was available at the workplace of 54.6% of participants. Most of them considered that the time allocated to CR training during residency was inadequate, and thought that more time was needed for this purpose. Most had not dedicated (or intended to dedicate) time for CR training, with lack of time being the most frequently attributed reason. In terms of referral, a substantial proportion of subjects did not refer patients, with lack of CR centers and human resources being the most frequent reasons.
ConclusionsThis survey provides contemporary data on CR training and attitudes, highlighting areas of potential improvement, such as time allocated to training in this area. These results could provide a useful pragmatic framework for optimization of training and awareness in this pivotal field of cardiovascular medicine.
A reabilitação cardíaca (RC) é um componente central da abordagem da doença cardiovascular. Apesar dos seus potenciais benefícios terem sido extensamente explorados e confirmados, a sua aplicação é ainda subótima, sendo descritas várias possíveis barreiras. Este estudo pretendeu avaliar a formação e perspetivas referentes à RC entre médicos num contexto português.
MétodosUm questionário online estruturado em três partes (características de participantes, formação e perspetivas em RC, breve avaliação geral de conhecimentos) foi desenvolvido e enviado para membros da Sociedade Portuguesa de Cardiologia. A população em estudo englobou especialistas ou internos a partir do terceiro ano de programa de formação específica.
Resultados97 indivíduos (57,7% sexo masculino, 61,9% ≤50 anos de idade) apresentaram respostas válidas. A RC estava disponível no local de trabalho de 54,6% dos participantes. A maioria considerava que o tempo dedicado à formação em RC durante o internato foi inadequada, considerando que mais tempo seria necessário. A maioria não tinha dedicado (ou pretendia dedicar) tempo para a formação em RC, sendo a falta de tempo a razão mais frequentemente atribuída. Em termos de referenciação, uma proporção substancial de indivíduos não referenciava doentes, sendo a falta de centros de RC e recursos humanos os motivos mais frequentes.
ConclusõesEste inquérito fornece dados contemporâneos referentes ao treino e perspetivas acerca da RC, nomeadamente algumas áreas de potencial melhoria como o tempo alocado à formação. Estes resultados poderão fornecer uma base útil e pragmática para a otimização da formação e conhecimento neste campo fundamental da medicina cardiovascular.
Cardiac rehabilitation (CR) is one of the cornerstones of the contemporary management of cardiovascular disease (CVD).1,2 This intervention has progressively evolved over the years, currently comprising comprehensive multidisciplinary programs aimed at tackling various components ranging from exercise training and physical activity counseling to cardiovascular risk factor management, nutritional and psychosocial counseling, smoking cessation, educational sessions, and other aspects of CVD.3–5 Data show the benefits of these programs on different endpoints, further reinforcing its scope across various points of the cardiovascular continuum.6–9 These effects underscore the value of CR, which is echoed in current guidelines for heart diseases ranging from acute and chronic coronary syndromes to heart failure (HF), for which it is a class I indication.1,3,10,11
While the benefits of CR have been extensively explored, there are still several obstacles to its application in different patient populations.4,12,13 The availability of CR differs widely in terms of geographical areas, with referral rates often below ideal levels.14–16 The ESC-EORP EUROASPIRE V cross-sectional survey encompassing data on 8261 patients with coronary artery disease (CAD), conducted in 27 countries, showed that fewer than half of them were advised to participate in CR.17 In a Portuguese setting, a recent national survey on the use of CR also illustrated this point, reporting a suboptimal level of use (below 10% after an acute coronary syndrome [ACS]), reinforcing the need to optimize overall CR uptake.18 In a review by Chindhy et al., among the various potential barriers to CR use, apart from patient-related factors (such as comorbidities, psychological and socioeconomic factors, age, and gender), both physician- and system-related factors appeared to be of importance.13 While various issues (such as knowledge, endorsement, and availability of resources) could be related to these factors, and the fact that their relative impact has not been fully ascertained, they may have a relevant influence on CR use.13,19–21 Interestingly, some data show that physician knowledge on this area may be suboptimal, while a recent pilot study (albeit, as acknowledged by the authors, with a small sample and derived from a single center) reported that this can improve after an educational and training intervention.22–24
ObjectivesThe aim of the present study was to assess possible limitations and barriers to training in CR among physicians, and to provide insights on interest and attitudes concerning this field. This is, to the best of our knowledge, the first study specifically designed to address these issues in a Portuguese setting.
MethodsA 32-item online open questionnaire in Portuguese was developed specifically for this national cross-sectional study aiming to assess physicians’ training and attitudes concerning CR. Prior studies provided background information assessed when structuring the survey, which was developed considering recommendations for designing questionnaires and the Checklist for Reporting Results of Internet E-Surveys (CHERRIES).22,23,25–27
The final version of the questionnaire was divided into three sections. The first section included nine items addressing participant characteristics, including demographic data such as age, gender, medical specialty, years of work experience and workplace features (such as the presence of a CR program, as well as interventional cardiology and cardiac surgery). The second section contained 18 items encompassing training in the field of CR and aimed at addressing subjects’ attitudes toward this topic (particularly in terms of patient referral for different indications). The third section included five items providing a brief assessment of individuals’ general knowledge of CR, based on current guidelines and position statements.1–3,10,11
The questionnaire was developed by an expert panel that included members of the Portuguese Society of Cardiology (SPC)’s Working Group on Exercise Pathophysiology and CR, which approved its final version. This was then made available online to the SPC's mailing list, with answers being collected from October 20, 2022 to December 31, 2022. This was an anonymous and voluntary survey, and no financial compensation was provided for participation. The population under study comprised physicians with a medical specialty, most of them cardiologists, or residents (of different specialties) from the third year onward of a specialty program (this cut-off being chosen to allow for prior contact with different areas of cardiovascular medicine, namely CR). Informed consent was provided at the beginning of the questionnaire.
The results are presented as descriptive statistics, with categorical variables given as total numbers and percentages (n/%).
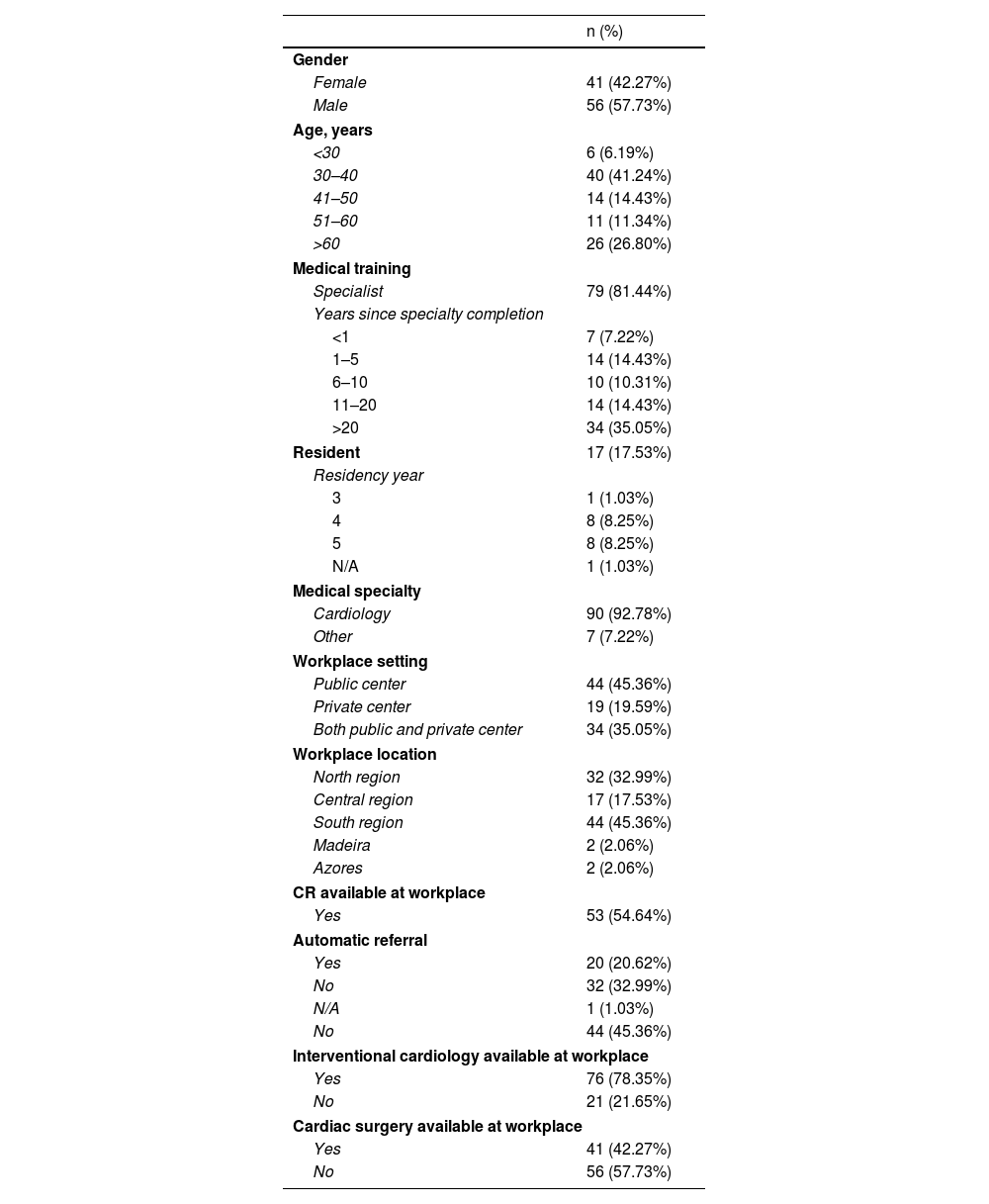
ResultsThe SPC's mailing list included 1276 potential participants. Over the time period of the survey a total of 97 individuals provided valid answers (7.6% response rate). Most of the respondents were male (57.7%) and the majority (61.9%) were ≤50 years old. Most were specialists (81.4%), with cardiology being the most frequent medical specialty represented. Among individuals in whose workplace CR was available, 75.5% reported having phase I, 84.9% phase II, and 47.2% phase III programs. Of those who reported not having CR available at their workplace, 25% reported referring patients to other centers. Overall participant characteristics are depicted in Table 1.
Participant characteristics.
| n (%) | |
|---|---|
| Gender | |
| Female | 41 (42.27%) |
| Male | 56 (57.73%) |
| Age, years | |
| <30 | 6 (6.19%) |
| 30–40 | 40 (41.24%) |
| 41–50 | 14 (14.43%) |
| 51–60 | 11 (11.34%) |
| >60 | 26 (26.80%) |
| Medical training | |
| Specialist | 79 (81.44%) |
| Years since specialty completion | |
| <1 | 7 (7.22%) |
| 1–5 | 14 (14.43%) |
| 6–10 | 10 (10.31%) |
| 11–20 | 14 (14.43%) |
| >20 | 34 (35.05%) |
| Resident | 17 (17.53%) |
| Residency year | |
| 3 | 1 (1.03%) |
| 4 | 8 (8.25%) |
| 5 | 8 (8.25%) |
| N/A | 1 (1.03%) |
| Medical specialty | |
| Cardiology | 90 (92.78%) |
| Other | 7 (7.22%) |
| Workplace setting | |
| Public center | 44 (45.36%) |
| Private center | 19 (19.59%) |
| Both public and private center | 34 (35.05%) |
| Workplace location | |
| North region | 32 (32.99%) |
| Central region | 17 (17.53%) |
| South region | 44 (45.36%) |
| Madeira | 2 (2.06%) |
| Azores | 2 (2.06%) |
| CR available at workplace | |
| Yes | 53 (54.64%) |
| Automatic referral | |
| Yes | 20 (20.62%) |
| No | 32 (32.99%) |
| N/A | 1 (1.03%) |
| No | 44 (45.36%) |
| Interventional cardiology available at workplace | |
| Yes | 76 (78.35%) |
| No | 21 (21.65%) |
| Cardiac surgery available at workplace | |
| Yes | 41 (42.27%) |
| No | 56 (57.73%) |
CR: cardiac rehabilitation; N/A: not available.
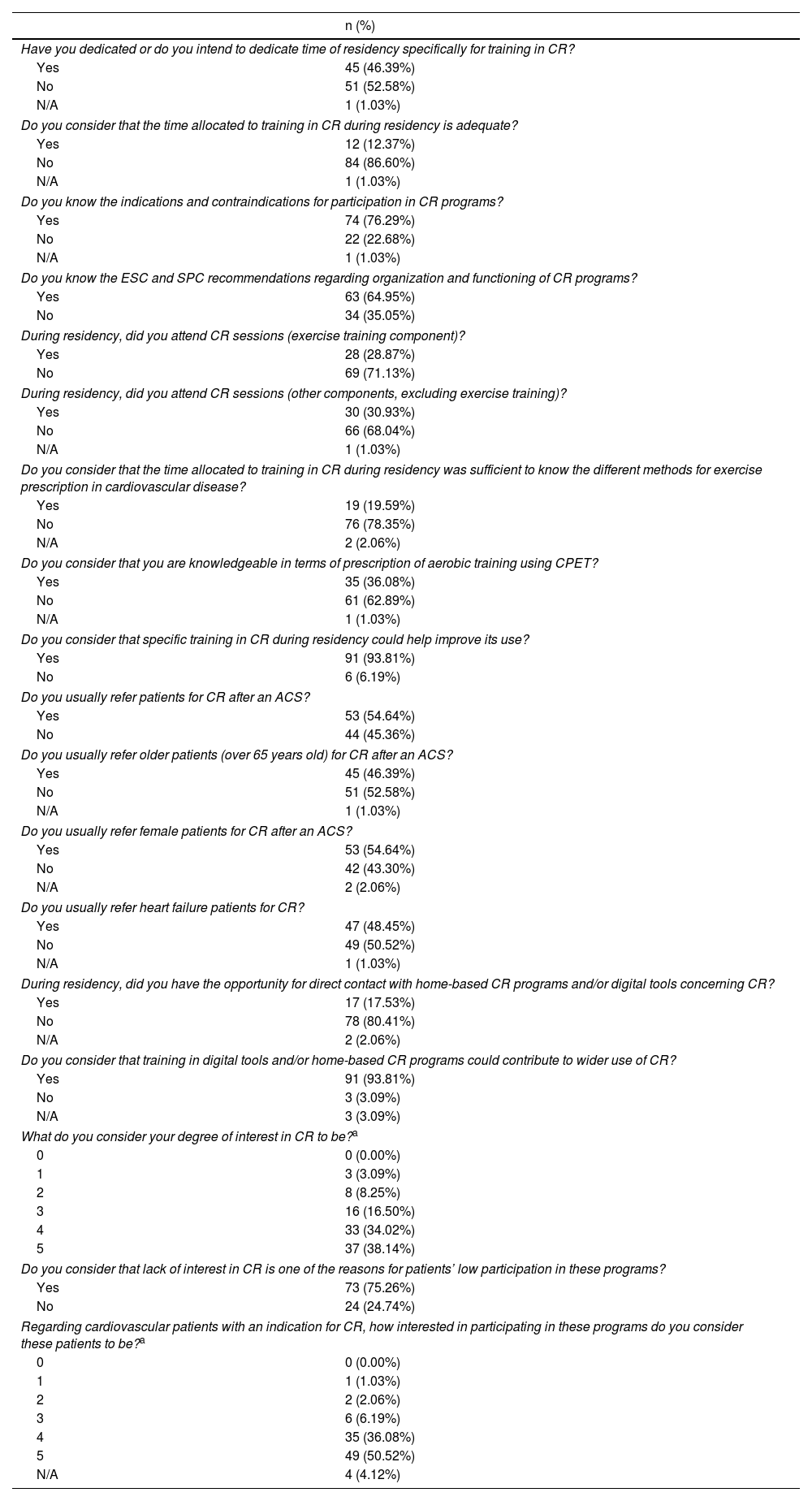
An overview of the second part of the questionnaire is presented in Table 2. More than half of participants (52.6%) reported not having dedicated or not intending to dedicate residency time specifically for the purpose of training in CR. When addressing the reasons for this, 51.0% reported lack of time, 25.5% lack of interest, 19.6% lack of recognition (namely in terms of certification by medical societies), 2.0% financial reasons and 2.0% other reasons. Most subjects (86.6%) considered that the time allocated to CR training during residency was inadequate. When these were asked whether more or less time was needed for this purpose, 100% responded the former; when asked how this training should be incorporated, 69.0% proposed a dedicated rotation. Most survey respondents did not attend CR sessions during residency (Table 2). When considering some of the CR components, 28.9% reported having attended sessions dedicated to exercise training, 25.8% sessions on cardiovascular risk factors or functional assessment, 25.8% sessions on cardiovascular risk factor control, 15.5% educational sessions, 9.3% sessions on smoking cessation interventions, 6.2% sessions on nutritional interventions and 3.1% sessions on psychological or social interventions.
Training and attitudes concerning cardiac rehabilitation.
| n (%) | |
|---|---|
| Have you dedicated or do you intend to dedicate time of residency specifically for training in CR? | |
| Yes | 45 (46.39%) |
| No | 51 (52.58%) |
| N/A | 1 (1.03%) |
| Do you consider that the time allocated to training in CR during residency is adequate? | |
| Yes | 12 (12.37%) |
| No | 84 (86.60%) |
| N/A | 1 (1.03%) |
| Do you know the indications and contraindications for participation in CR programs? | |
| Yes | 74 (76.29%) |
| No | 22 (22.68%) |
| N/A | 1 (1.03%) |
| Do you know the ESC and SPC recommendations regarding organization and functioning of CR programs? | |
| Yes | 63 (64.95%) |
| No | 34 (35.05%) |
| During residency, did you attend CR sessions (exercise training component)? | |
| Yes | 28 (28.87%) |
| No | 69 (71.13%) |
| During residency, did you attend CR sessions (other components, excluding exercise training)? | |
| Yes | 30 (30.93%) |
| No | 66 (68.04%) |
| N/A | 1 (1.03%) |
| Do you consider that the time allocated to training in CR during residency was sufficient to know the different methods for exercise prescription in cardiovascular disease? | |
| Yes | 19 (19.59%) |
| No | 76 (78.35%) |
| N/A | 2 (2.06%) |
| Do you consider that you are knowledgeable in terms of prescription of aerobic training using CPET? | |
| Yes | 35 (36.08%) |
| No | 61 (62.89%) |
| N/A | 1 (1.03%) |
| Do you consider that specific training in CR during residency could help improve its use? | |
| Yes | 91 (93.81%) |
| No | 6 (6.19%) |
| Do you usually refer patients for CR after an ACS? | |
| Yes | 53 (54.64%) |
| No | 44 (45.36%) |
| Do you usually refer older patients (over 65 years old) for CR after an ACS? | |
| Yes | 45 (46.39%) |
| No | 51 (52.58%) |
| N/A | 1 (1.03%) |
| Do you usually refer female patients for CR after an ACS? | |
| Yes | 53 (54.64%) |
| No | 42 (43.30%) |
| N/A | 2 (2.06%) |
| Do you usually refer heart failure patients for CR? | |
| Yes | 47 (48.45%) |
| No | 49 (50.52%) |
| N/A | 1 (1.03%) |
| During residency, did you have the opportunity for direct contact with home-based CR programs and/or digital tools concerning CR? | |
| Yes | 17 (17.53%) |
| No | 78 (80.41%) |
| N/A | 2 (2.06%) |
| Do you consider that training in digital tools and/or home-based CR programs could contribute to wider use of CR? | |
| Yes | 91 (93.81%) |
| No | 3 (3.09%) |
| N/A | 3 (3.09%) |
| What do you consider your degree of interest in CR to be?a | |
| 0 | 0 (0.00%) |
| 1 | 3 (3.09%) |
| 2 | 8 (8.25%) |
| 3 | 16 (16.50%) |
| 4 | 33 (34.02%) |
| 5 | 37 (38.14%) |
| Do you consider that lack of interest in CR is one of the reasons for patients’ low participation in these programs? | |
| Yes | 73 (75.26%) |
| No | 24 (24.74%) |
| Regarding cardiovascular patients with an indication for CR, how interested in participating in these programs do you consider these patients to be?a | |
| 0 | 0 (0.00%) |
| 1 | 1 (1.03%) |
| 2 | 2 (2.06%) |
| 3 | 6 (6.19%) |
| 4 | 35 (36.08%) |
| 5 | 49 (50.52%) |
| N/A | 4 (4.12%) |
ACS: acute coronary syndrome; CPET: cardiopulmonary exercise testing; CR: cardiac rehabilitation; ESC: European Society of Cardiology; N/A: not available; SPC: Portuguese Society of Cardiology.
A total of 45.4% of survey participants reported that they did not usually refer patients for CR after an ACS. Among these, 81.8% reported lack of CR centers in their region, 70.5% lack of human resources (in their center) for these programs, 13.6% that they considered patients would not attend, 4.5% lack of time to discuss this issue with patients, 2.3% their doubts about the benefits of CR, and 2.3% their doubts about the cost-effectiveness of these programs. With regard to older patients (aged over 65 years) after an ACS, 52.6% of participants reported not usually referring these individuals for CR. Among these, 72.5% reported lack of CR centers in their region, 74.5% lack of human resources (in their center) for these programs, 11.8% that they considered patients would not attend, 5.9% lack of time to discuss this issue with patients, and 2.0% their doubts about the benefits of these programs. When addressing female patients after an ACS, 43.3% of participants reported not usually referring these patients for CR. Concerning the reasons for this lack of referral, 76.2% cited lack of CR centers in their region, 76.2% lack of human resources (in their center) for these programs, 7.1% that they considered patients would not attend, 7.1% lack of time to discuss this issue with patients, and 2.4% their doubts about the benefits of these programs. When asked about referral of HF patients, 50.5% of respondents reported not usually referring these for CR. As reasons for this, 73.5% cited lack of CR centers in their region, 71.4% lack of human resources (in their center) for these programs, 6.1% that they considered patients would not attend, 10.2% lack of time to discuss this issue with patients, and 4.1% their doubts about the safety of these programs, while 2.0% had doubts about their cost-effectiveness. Most participants had not had direct contact with home-based CR (HBCR) programs or digital tools in this field. Despite this, most (93.8%) considered that training in HBCR models and/or digital tools could help to widen use of this intervention.
Most participants (72.2%) reported being either interested or very interested in CR; of note, however, most also considered that lack of interest in these programs was one of the reasons for patients’ low participation (Table 2).
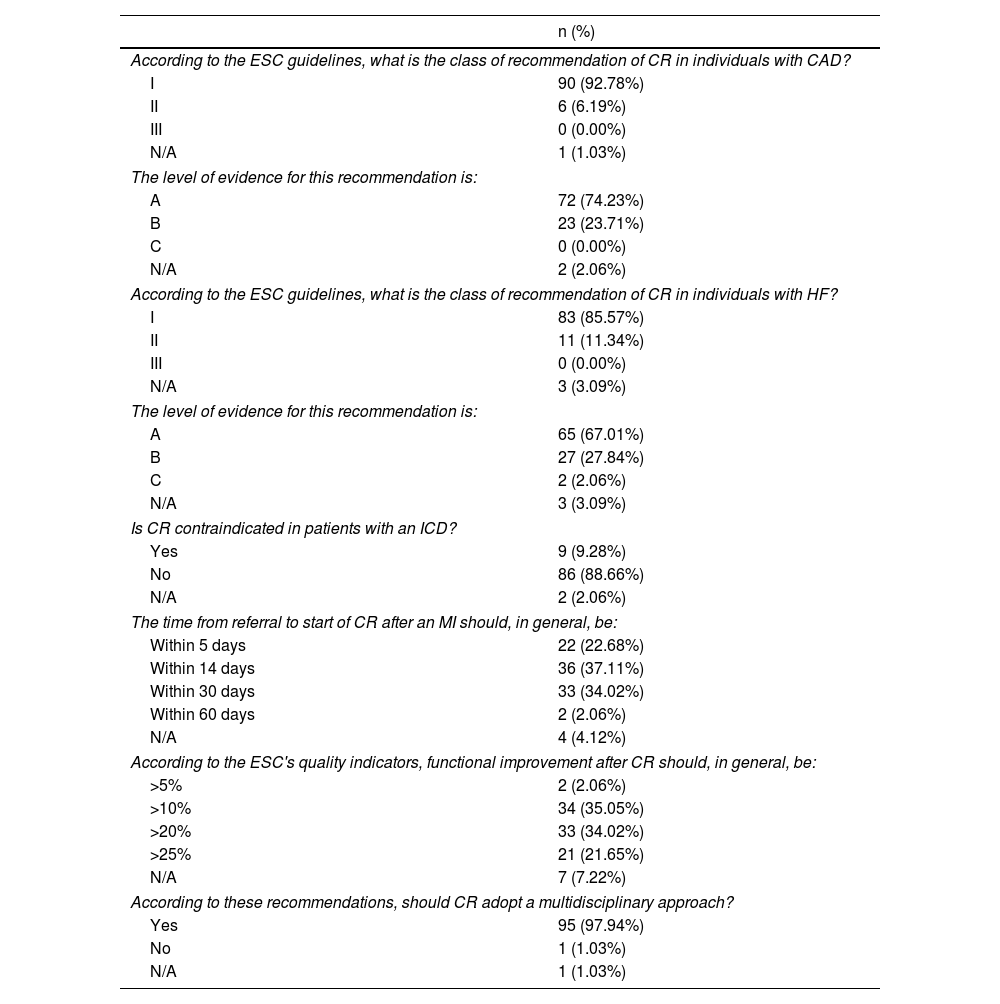
An overview of the third part of the questionnaire (assessing general knowledge of CR) is depicted in Table 3. Most survey respondents were knowledgeable in terms of the indications for CR and its multidisciplinary approach. In terms of general quality indicators, however, most did not respond correctly to questions regarding waiting time from referral to start of CR after a myocardial infarction (MI) and functional improvement.3
Assessment of general knowledge of cardiac rehabilitation.
| n (%) | |
|---|---|
| According to the ESC guidelines, what is the class of recommendation of CR in individuals with CAD? | |
| I | 90 (92.78%) |
| II | 6 (6.19%) |
| III | 0 (0.00%) |
| N/A | 1 (1.03%) |
| The level of evidence for this recommendation is: | |
| A | 72 (74.23%) |
| B | 23 (23.71%) |
| C | 0 (0.00%) |
| N/A | 2 (2.06%) |
| According to the ESC guidelines, what is the class of recommendation of CR in individuals with HF? | |
| I | 83 (85.57%) |
| II | 11 (11.34%) |
| III | 0 (0.00%) |
| N/A | 3 (3.09%) |
| The level of evidence for this recommendation is: | |
| A | 65 (67.01%) |
| B | 27 (27.84%) |
| C | 2 (2.06%) |
| N/A | 3 (3.09%) |
| Is CR contraindicated in patients with an ICD? | |
| Yes | 9 (9.28%) |
| No | 86 (88.66%) |
| N/A | 2 (2.06%) |
| The time from referral to start of CR after an MI should, in general, be: | |
| Within 5 days | 22 (22.68%) |
| Within 14 days | 36 (37.11%) |
| Within 30 days | 33 (34.02%) |
| Within 60 days | 2 (2.06%) |
| N/A | 4 (4.12%) |
| According to the ESC's quality indicators, functional improvement after CR should, in general, be: | |
| >5% | 2 (2.06%) |
| >10% | 34 (35.05%) |
| >20% | 33 (34.02%) |
| >25% | 21 (21.65%) |
| N/A | 7 (7.22%) |
| According to these recommendations, should CR adopt a multidisciplinary approach? | |
| Yes | 95 (97.94%) |
| No | 1 (1.03%) |
| N/A | 1 (1.03%) |
CAD: coronary artery disease; CR: cardiac rehabilitation; ESC: European Society of Cardiology; HF: heart failure; ICD: implantable cardioverter-defibrillator; MI: myocardial infarction; N/A: not available.
In this national survey on CR, in which cardiology was the most frequent medical specialty represented (92.8%) and in which CR was available at the workplace of 54.6% of participants, most individuals reported that the time allocated to CR training during residency was inadequate, and thought that more time was needed for this purpose. Just over half of subjects (52.6%) had not dedicated (or intended to dedicate) time of residency specifically for the purpose of training in CR. Importantly, among these, lack of time was the most frequently attributed reason, while lack of interest and recognition were the second and third most frequently chosen factors, respectively. Also, as depicted in Table 2, most respondents had not attended CR sessions during residency. In terms of patient referral for some of the most frequent CR indications (after ACS and HF), a substantial proportion of individuals did not refer these patients, with lack of CR centers and human resources being among the most frequently cited reasons for this (Figure 1).
Since its inception, CR has consistently shown benefits in different clinical contexts.2,7,28 Nevertheless, evidence also shows that participation in these programs has been suboptimal across different timepoints.4,13,14 This notion has been explored in a landmark study by Bjarnason-Wehrens et al. based on the European Cardiac Rehabilitation Inventory, which showed marked heterogeneity across regions.29 Moreover, a recent survey of post-MI management conducted in physicians in different European countries also showed important variations in rates of CR referral.30 These findings agree with the present results, showing a substantial gap in terms of referrals. While, as previously mentioned, a plethora of factors could influence this uptake, limitations related to availability of facilities and staff have also been previously described.16,31,32
In parallel with major breakthroughs in cardiovascular medicine, CR has also experienced significant advances.4,8,28,33 This highly specialized field has incorporated inputs from a wide range of areas, reflecting the diverse aspects tackled by this intervention.3,33 This specialization also resonates with several of the points in the core curriculum in preventive cardiology recently proposed by the European Association of Preventive Cardiology.34 Furthermore, beyond classical indications such as CAD and HF, rapidly evolving areas such as cardio-oncology rehabilitation, CR in recipients of cardiac implantable electronic devices and following valvular interventions (both surgical and percutaneous), continue to expand the horizons of these programs.2,35,36 Interestingly, most survey participants reported that more time was needed for CR training (during residency), with most reporting a preference for a dedicated rotation. In this regard, it should be recalled that among those who did not dedicate specific time for CR training during residency, lack of time was the most frequently reported factor. Moreover, most individuals reported not considering that time allocated to CR during residency allowed for knowledge of the different methods of exercise prescription, with most (62.9%) also reporting limitations in terms of aerobic training prescription using cardiopulmonary exercise stress testing. Finally, in terms of general knowledge assessment (Table 3), while most correctly answered questions regarding some of the indications for CR, there was substantial variation when addressing the final two questions of the questionnaire. These points could, at least partially, support the idea that specific training in this area is needed, in order to improve overall knowledge in this pivotal field.
The application of various novel methodologies in CR is a focus of increasing interest, as a potential way to mitigate some of the barriers to these programs.4,32,37 In this regard, HBCR programs and the use of digital tools have been among the strategies considered over the years, with this expansion having been significantly influenced by the recent COVID-19 pandemic.4,37–40 Although most subjects had not had direct contact with these tools, most nonetheless considered that they could aid in the wider use of CR, reflecting the current notion that adapting prior paradigms for its provision could streamline its application to a broader population.4,41 While this idea is promising, however, it should be noted that various issues, namely those related to patient selection and preferences, should also be considered before its potential generalization.4,38,42
Some limitations should be taken into consideration when assessing the present data. Firstly, the number of participants in this survey was relatively low, with the response rate being lower than that reported in other areas.43,44 Although several factors could have contributed to this, the low response rate, coupled with the fact that among those who responded, most considered that low interest in CR could be one of the reasons for patients’ low participation, should be taken into consideration. Indeed, as novel approaches to CR delivery continue to appear, knowledge and motivation could have a crucial role in process optimization.4,21,45,46 Despite this, the participation of individuals from different locations and work settings (particularly in terms of CR availability) should be considered a positive aspect of this survey. Secondly, the present survey was sent to the mailing list of the SPC. Data collection was thus limited to members of this society. Furthermore, the survey specifically addressed physicians’ training and attitudes in CR. Given the multidisciplinary nature of this intervention, future studies should aim to address these aspects across other fields of practice integrating these programs.3,33 In addition, to our knowledge, data on the number of members who were first- or second-year residents (as well as those not fulfilling criteria specified in the Methods section) were not available. As such, a projected number of potential participants was considered. Finally, the fact that those who responded to this survey may tend to be more interested and active in this area should also be noted, as discussed in other studies.44,47 While these limitations should be acknowledged, the present pragmatic study provides important and novel data on training and attitudes concerning CR in physicians in a Portuguese setting. Given the lack of data in this field, we believe these inputs could provide a useful framework for future studies on this topic, with the aim of increasing interest in, optimizing training for and improving overall access to CR.
ConclusionsThis national survey on CR training and attitudes in a Portuguese setting highlights some of the hurdles and potential areas for further improvement in this field. Most subjects considered the time allocated to training in this area to be suboptimal. As CR programs become increasingly personalized, to address the myriad challenges associated with CVD, these results could provide useful insights to improve overall training and awareness in this pivotal area of cardiovascular medicine.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to thank all the participants in the present survey for their valuable time and contributions. The authors would also like to thank the SPC for their continuing support in this endeavor.