Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a rare genetic disease, characterized by the replacement of the myocardium with fibro-fatty tissue. Although ARVC encompasses a wide range of symptoms, the most common form of presentation is sudden cardiac death (SCD) due to ventricular arrhythmias. We present three patients with ARVC and different clinical presentations, all viewed and analyzed from a common vantage point: cardiac magnetic resonance (CMR). Genetic testing for ARVC was not performed.
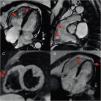
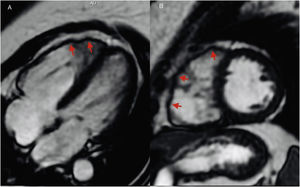
A 45-year-old female patient with no health issues presented to the emergency room for syncope during exertion. The electrocardiogram (ECG) showed negative T waves V1-V3; the laboratory tests and echocardiography were normal. A CMR scan was performed which revealed the following: thin right ventricular (RV) free wall with hypokinesia and multiple microaneurysms, RV end-diastolic volume (RVEDV) of 105 mL/m2 and RV ejection fraction (RVEF) of 32% (Figure 1). Based on the Task Force Criteria for ARVC diagnosis, the patient fulfilled two major criteria and was scheduled for intracardiac defibrillator (ICD) implantation.1 The T wave inversion in the right precordial leads other than V1-V2 should be investigated for underlying structural heart disease that might lead to SCD.2
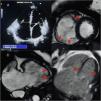
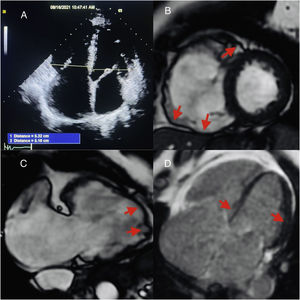
A 54-year-old female patient known to have hypothyroidism presented to the ambulatory care complaining of palpitations. The ECG recorded negative T waves in V1-V4. The two-dimensional echocardiogram showed a dilated RV. The 24-h Holter ECG highlighted frequent polymorphic ventricular extrasystoles and two episodes of non-sustained ventricular tachycardia. CMR revealed the following: dilated RV with RVEDV of 119 mL/m2, regional RV free wall akinesia with inflow, apex and outflow tract bulging (Figure 2). These sites are considered pathognomonic features of ARVC (the “triangle of dysplasia”).3 Axial black blood images showed irregularities between epicardial fat and anterior RV free wall, suggestive of fatty infiltration (Figure 2). Late gadolinium enhancement (LGE) was seen toward the RV apex and in the mid-epicardial layer of the apical left ventricular (LV) lateral wall (Figure 2). The diagnosis was ARVC with LV involvement.
(A) Cardiac magnetic resonance (CMR) horizontal long-axis CINE right ventricular (RV) anterior wall aneurysms; (B) CMR CINE RV outflow tract aneurysms; (C) axial black blood T1 RV free wall irregularities (fat infiltration); (D) RV apical and LV apical lateral wall late gadolinium enhancement.
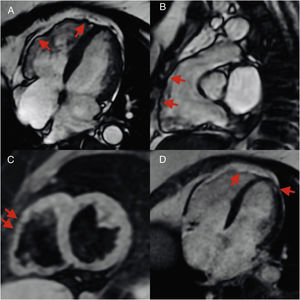
A 62-year-old female patient with no history of cardiovascular disease was admitted to our cardiology ward with acute heart failure. N-terminal proB-type natriuretic peptide was 8789 pg/mL. Echocardiography showed an RV/LV ratio >1, LV global hypokinesia with 30% EF (Figure 3). The computed tomography pulmonary angiogram was normal. CMR revealed regional RV free wall hypokinesia with aneurysms (Figure 3), RVEDV of 179 mL/m2 with 24% RVEF, epicardial LV posterolateral wall LGE, basal mid-septum LGE and RV free wall LGE (Figure 3). The final diagnosis was biventricular arrhythmogenic cardiomyopathy. The management of the patient included angiotensin-converting enzyme inhibitors, beta-blockers, diuretics and ICD implantation. Numerous studies have confirmed a high prevalence of LV involvement among ARVC patients with a range from 61% to 76% of cases.4,5
We illustrate three different presentations of ARVC, in which CMR was crucial for the diagnosis as it identified major imaging criteria. In fact, with high spatial resolution and tissue characterization sequences, CMR is the ideal methodology to functionally and structurally assess the RV and thus avoid invasive methods such as biopsy.
FundingThis work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestThe authors have no conflicts of interest to declare.