Patient selection for percutaneous coronary intervention (PCI) in chronic total occlusions (CTOs) is crucial to procedural success. Our aim was to identify independent predictors of success in CTO PCI in order to create an accurate score.
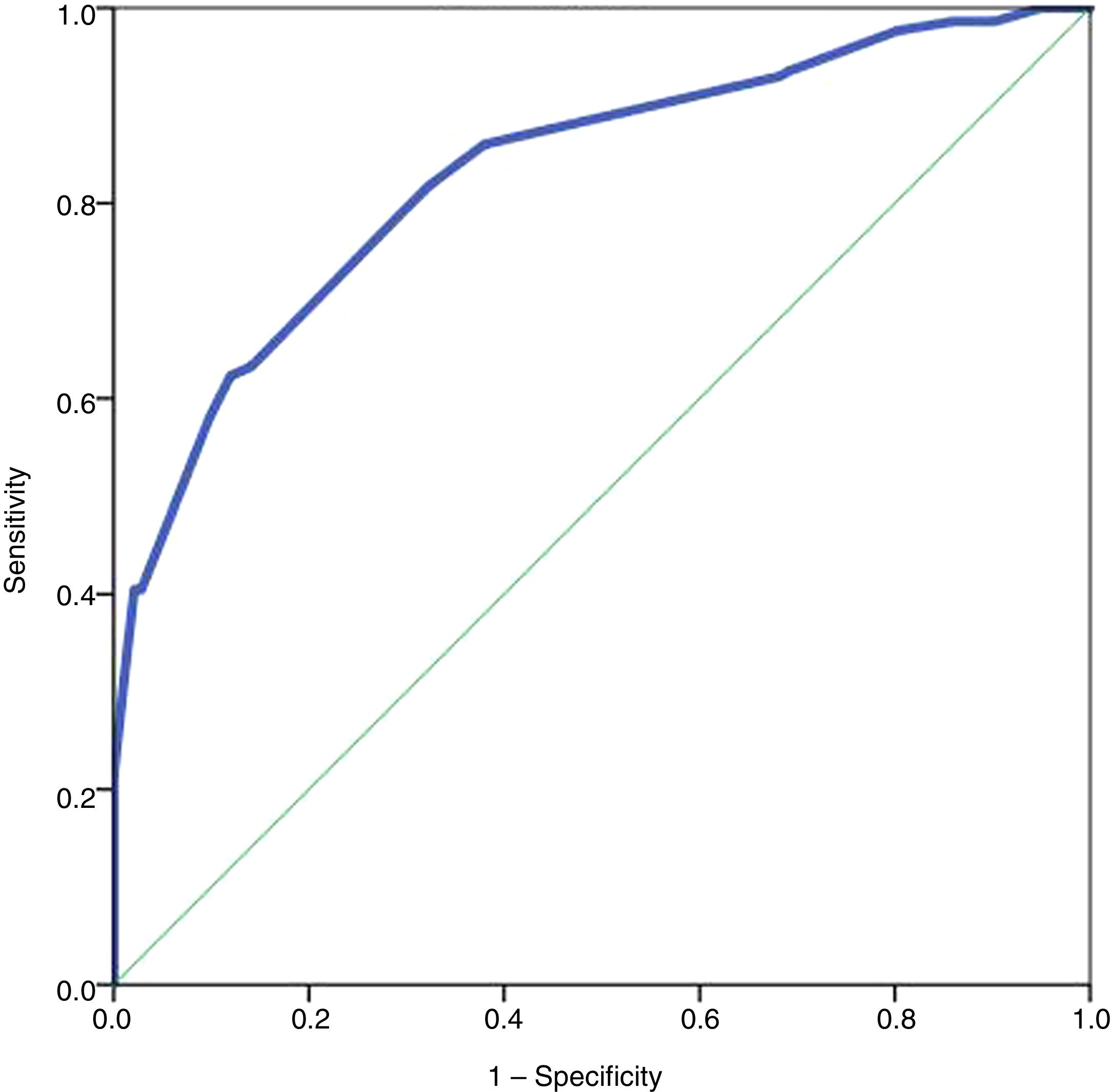
MethodsIn a single-center observational registry of CTO PCI, demographic and clinical data and anatomical characteristics of coronary lesions were recorded. Linear and logistic regression analysis were used to identify predictors of success. A score to predict success was created and its accuracy was measured by receiver operating curve analysis.
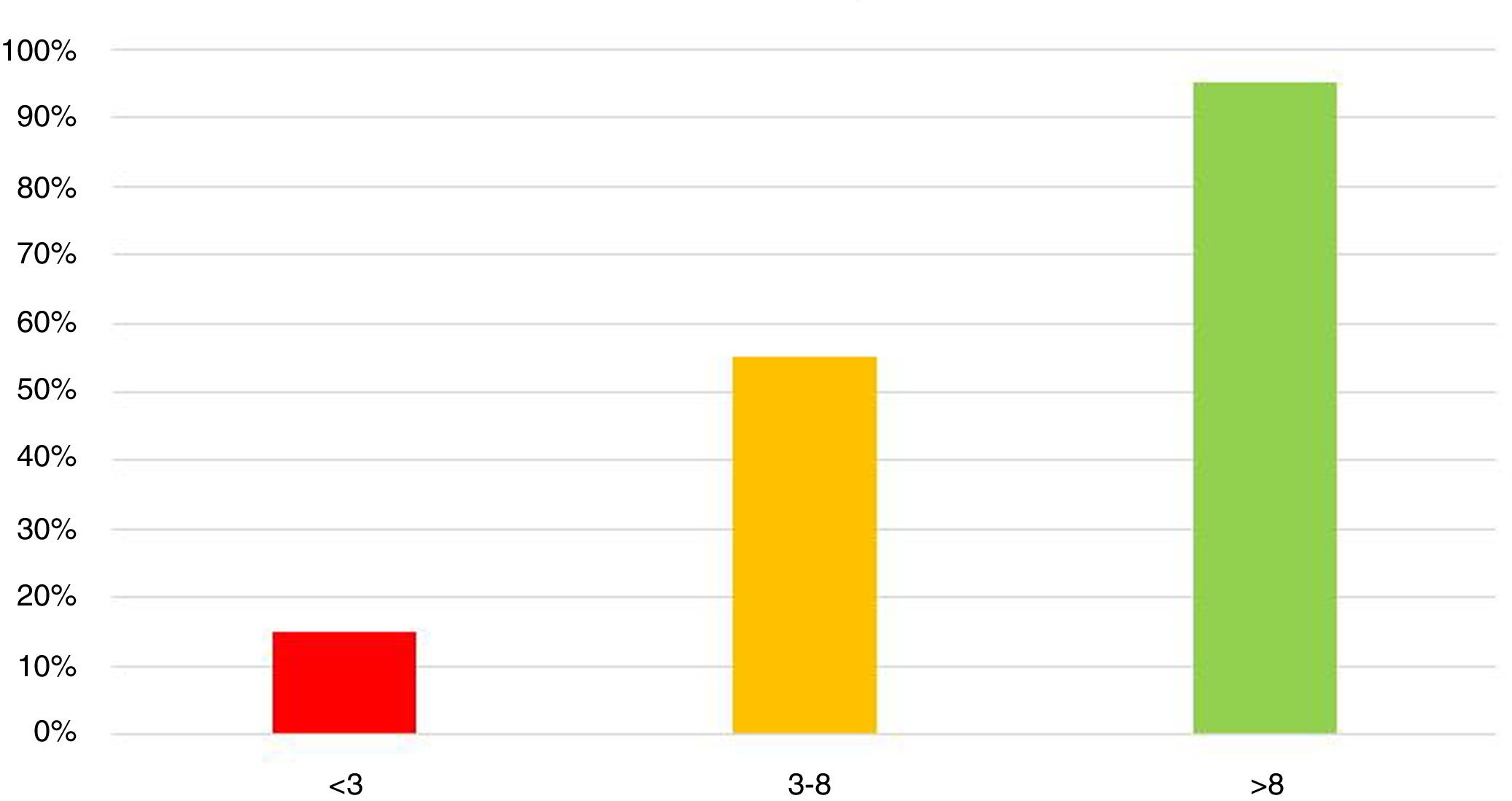
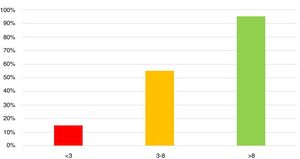
ResultsA total of 377 interventions were performed (334 patients, age 68±11 years, 75% male). The success rate was 65% per patient and 60% per procedure. Predictors of success in univariate analysis were absence of active smoking (OR 2.02, 95% CI 1.243-3.29; p=0.005), presence of tapered stump (OR 5.2, 95% CI 2.7-10.2; p<0.001), absence of tortuosity (OR 6.44; 95% CI 3.02-13.75; p<0.001), absence of bifurcation (OR 1.95; 95% CI 1.08-3.51; p=0.026), absence of calcification (OR 3.1; 95% CI 3.10-5.41; p<0.001), LAD as target vessel (OR 1.9, 95% CI 1.0-3.5; p=0.048), and CTO length <20 mm (OR 3.00, 95% CI 1.69-5.3; p<0.001). Only anatomical factors were independent predictors of success, and an anatomical score (0-11 points) with high accuracy (area under the curve 0.831) was subsequently created. A score <3 was associated with low probability of success (15%), 3-8 with intermediate probability (55%), and >8 with high probability (95%).
ConclusionIn our sample only anatomical characteristics were predictors of success. The creation of a score to predict success, with good accuracy, may enable selection of cases that can be treated by any operator, those in which a dedicated operator will be desirable, and those with an extremely low probability of success, which should be considered individually for conservative management, surgical revascularization or PCI by a team experienced in CTO.
Selecionar os doentes para angioplastia (ICP) de oclusão crónica (CTO) é crucial para o êxito do procedimento. Pretende-se identificar preditores independentes de sucesso na ICP de CTOs para criação de um score de boa acuidade.
MétodosRegisto observacional unicêntrico de ICP em CTOs. Registaram-se características demográficas, clínicas e características anatómicas das lesões. Identificados preditores de sucesso por regressão linear e logística, posterior construção de score preditor de sucesso cuja acuidade foi aferida por análise com curva ROC.
ResultadosRealizaram-se 377 intervenções (334 doentes, 68±11 anos, 75% homens); taxa de sucesso por doente: 65%, por procedimento: 60%. Em análise univariada, foram preditores de sucesso: ausência de tabagismo (OR 2,02; 95%CI 1,243–3,29; p=0,005); coto afilado (C) (OR 5,2; 95%CI 2,7–10,2; p<0,001), ausência de tortuosidade intraoclusão (To) (OR 6,44; 95%CI 3,02–13,75; p<0,001), ausência de bifurcação (aB) (OR 1,95; 95%CI 1,08–3,51; p=0,026), ausência de calcificação (C) (OR 3,1; 95%CI 3,10–5,41; p<0,001), vaso-alvo descendente anterior (D) (OR 1,9; 95%CI 1,0–3,5; p=0,048), extensão<20 mm(E) (OR 3,00; 95%CI 1,69–5,3; p<0,001). Apenas os fatores anatómicos foram preditores independentes de sucesso. Com base nestes dados criou-se um score anatómico, entre 0-11, com elevada acuidade (AUC 0,831). Um score <3 associou-se a probabilidade de sucesso reduzida (15%), entre 3-8 a probabilidade intermédia (55%) e>8 a probabilidade elevada (95%).
ConclusãoNesta amostra, apenas as características anatómicas foram preditoras de sucesso. Um score de sucesso poderá permitir selecionar casos passíveis de intervenção por qualquer operador, aqueles que requerem operador dedicado a oclusões e aqueles com probabilidade de sucesso reduzida onde se considere individualmente manejo conservador, revascularização cirúrgica ou ICP por equipa experiente/dedicada.
Percutaneous coronary intervention (PCI) has evolved significantly since its introduction over 40 years ago, in 1977, and has now reached a level of technical sophistication that enables the revascularization of highly complex lesions. PCI in chronic total occlusions (CTOs) is often described as the last frontier of interventional cardiology, due to its difficulty and the high degree of technical skill required.
Studies and meta-analyses suggest that CTO PCI can lead to improvements in symptoms and quality of life,1,2 global systolic function3 and prognosis.4 However, the European guidelines on myocardial revascularization still only give the technique a class IIa recommendation,5 due to the lack of randomized clinical trials unequivocally demonstrating the benefit of the intervention. The overall results of the DECISION CTO trial6 were neutral in this regard, and the EURO-CTO trial7 showed no effect on prognosis, only on quality of life. However, these trials had various methodological limitations, and it is widely acknowledged that it is difficult to carry out clinical trials with sufficient statistical power to obtain clinically significant results in this setting.
Given the highly complex nature and not inconsiderable risk of CTO PCI and the other limitations described above, it would be useful to have simple and objective criteria that would facilitate the selection of patients who would benefit from it. These criteria could be combined in a simple and objective score, like those used in other clinical settings, such as acute coronary syndrome8 or atrial fibrillation.9,10
The only widely used score for CTOs is the J-CTO score, which was designed to grade the complexity of CTO lesions for PCI. However, it was not intended to aid decision-making or for stratifying patients who might benefit from the procedure; its only endpoint is successful guidewire crossing within 30 minutes via an anterograde approach, and it is thus basically useful only for dedicated operators.11
In the present study, the authors aimed to identify predictors of success in CTO PCI based on data from the registry of a high-volume center and to bring them together in an easy-to-use score. Such a score may be used to select the best strategy for each case, identifying patients in whom CTO PCI can be attempted with a reasonable chance of success, and indicating the level of technical skill required by the operator, thereby optimizing resources and minimizing risks.
MethodsThe study is based on an observational registry of consecutive patients who underwent CTO PCI in a single center between 2015 and 2018. CTO was defined as a coronary artery lesion with TIMI flow 0 for at least three months. Procedural success was defined as PCI with stent placement resulting in TIMI flow 3. All procedures performed were analyzed, regardless of the operator or technique, or whether or not the procedure was part of a CTO treatment program.
Patients’ demographic and clinical data, anatomical characteristics of coronary lesions, and technical details of the procedure were recorded.
Statistical analysisThe chi-square test was used to analyze associations between results and categorical variables and the Student's t test for associations between results and quantitative variables.
To identify predictors of success, linear regression analysis was used for quantitative variables and logistical regression for categorical variables.
Multivariate analysis was used to identify independent predictors. The relative contribution of each predictor, expressed by the corresponding odds ratio (OR), was used to create a score to predict success, categorized as high, intermediate or low probability of success. Its accuracy was measured by receiver operating curve analysis.
The statistical analysis was performed using IBM SPSS Statistics® version 24.
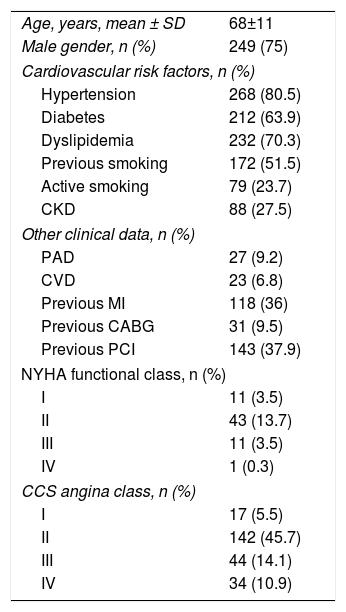
ResultsOverall findingsA total of 377 interventions were performed on 334 patients. Mean age was 68±11years and 75% were male. Detailed results are displayed in Tables 1–4.
Demographic and clinical characteristics of the study population.
| Age, years, mean ± SD | 68±11 |
| Male gender, n (%) | 249 (75) |
| Cardiovascular risk factors, n (%) | |
| Hypertension | 268 (80.5) |
| Diabetes | 212 (63.9) |
| Dyslipidemia | 232 (70.3) |
| Previous smoking | 172 (51.5) |
| Active smoking | 79 (23.7) |
| CKD | 88 (27.5) |
| Other clinical data, n (%) | |
| PAD | 27 (9.2) |
| CVD | 23 (6.8) |
| Previous MI | 118 (36) |
| Previous CABG | 31 (9.5) |
| Previous PCI | 143 (37.9) |
| NYHA functional class, n (%) | |
| I | 11 (3.5) |
| II | 43 (13.7) |
| III | 11 (3.5) |
| IV | 1 (0.3) |
| CCS angina class, n (%) | |
| I | 17 (5.5) |
| II | 142 (45.7) |
| III | 44 (14.1) |
| IV | 34 (10.9) |
CABG: coronary artery bypass grafting; CCS: Canadian Cardiovascular Society; CKD: chronic kidney disease; CVD: cerebrovascular disease; MI: myocardial infarction; NYHA: New York Heart Association; PAD: peripheral arterial disease; PCI: percutaneous coronary intervention; SD: standard deviation.
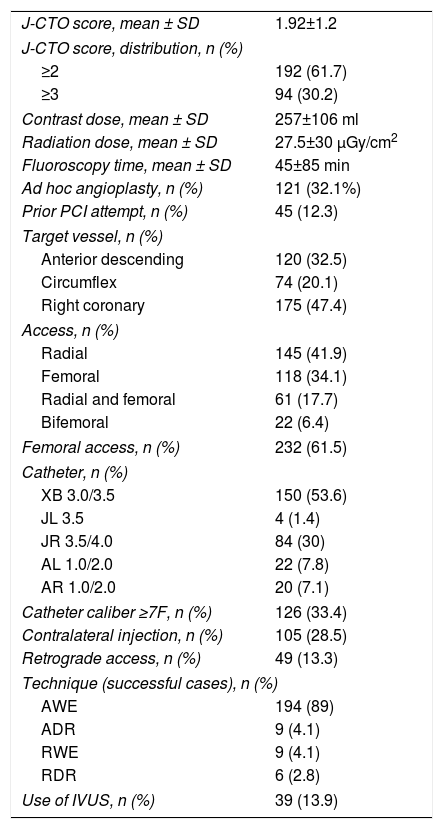
Procedural characteristics.
| J-CTO score, mean ± SD | 1.92±1.2 |
| J-CTO score, distribution, n (%) | |
| ≥2 | 192 (61.7) |
| ≥3 | 94 (30.2) |
| Contrast dose, mean ± SD | 257±106 ml |
| Radiation dose, mean ± SD | 27.5±30 μGy/cm2 |
| Fluoroscopy time, mean ± SD | 45±85 min |
| Ad hoc angioplasty, n (%) | 121 (32.1%) |
| Prior PCI attempt, n (%) | 45 (12.3) |
| Target vessel, n (%) | |
| Anterior descending | 120 (32.5) |
| Circumflex | 74 (20.1) |
| Right coronary | 175 (47.4) |
| Access, n (%) | |
| Radial | 145 (41.9) |
| Femoral | 118 (34.1) |
| Radial and femoral | 61 (17.7) |
| Bifemoral | 22 (6.4) |
| Femoral access, n (%) | 232 (61.5) |
| Catheter, n (%) | |
| XB 3.0/3.5 | 150 (53.6) |
| JL 3.5 | 4 (1.4) |
| JR 3.5/4.0 | 84 (30) |
| AL 1.0/2.0 | 22 (7.8) |
| AR 1.0/2.0 | 20 (7.1) |
| Catheter caliber ≥7F, n (%) | 126 (33.4) |
| Contralateral injection, n (%) | 105 (28.5) |
| Retrograde access, n (%) | 49 (13.3) |
| Technique (successful cases), n (%) | |
| AWE | 194 (89) |
| ADR | 9 (4.1) |
| RWE | 9 (4.1) |
| RDR | 6 (2.8) |
| Use of IVUS, n (%) | 39 (13.9) |
ADR: antegrade dissection re-entry; AWE: antegrade wire escalation; IVUS: intravascular ultrasound; PCI: percutaneous coronary intervention; RDR: retrograde dissection re-entry; RWE: retrograde wire escalation; SD: standard deviation.
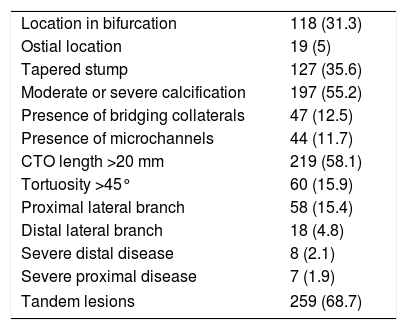
Anatomical characteristics of coronary lesions.
| Location in bifurcation | 118 (31.3) |
| Ostial location | 19 (5) |
| Tapered stump | 127 (35.6) |
| Moderate or severe calcification | 197 (55.2) |
| Presence of bridging collaterals | 47 (12.5) |
| Presence of microchannels | 44 (11.7) |
| CTO length >20 mm | 219 (58.1) |
| Tortuosity >45° | 60 (15.9) |
| Proximal lateral branch | 58 (15.4) |
| Distal lateral branch | 18 (4.8) |
| Severe distal disease | 8 (2.1) |
| Severe proximal disease | 7 (1.9) |
| Tandem lesions | 259 (68.7) |
Values are n (%).
CTO: chronic total occlusion.
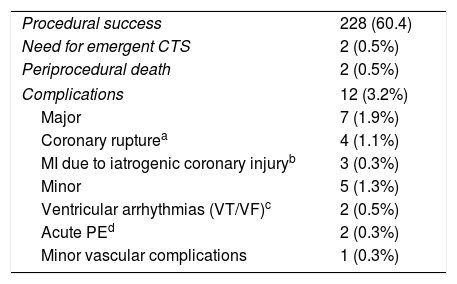
Outcomes and complications by procedure.
| Procedural success | 228 (60.4) |
| Need for emergent CTS | 2 (0.5%) |
| Periprocedural death | 2 (0.5%) |
| Complications | 12 (3.2%) |
| Major | 7 (1.9%) |
| Coronary rupturea | 4 (1.1%) |
| MI due to iatrogenic coronary injuryb | 3 (0.3%) |
| Minor | 5 (1.3%) |
| Ventricular arrhythmias (VT/VF)c | 2 (0.5%) |
| Acute PEd | 2 (0.3%) |
| Minor vascular complications | 1 (0.3%) |
The mean J-CTO score per procedure was 1.92±1.2. The success rate was 65% per patient and 60% per procedure.
The only demographic variable associated with success was presence of active smoking, but not previous smoking (chi-square=21.5; p<0.001). No clinical variable was associated with either success or failure, including the presence of diabetes, age or gender.
Anatomical variables associated with success were intervention in the left anterior descending artery (LAD) vs. other vessels (chi-square=5.088; p=0.024), presence of tapered stump (chi-square=41.5; p<0.001), absence of bifurcation (chi-square=21.5; p<0.001), absence of significant calcification (chi-square=22.14; p<0.001), length of occlusion <20 mm (chi-square=39.7; p<0.001), absence of significant CTO tortuosity (chi-square=30.5; p<0.001). The presence of a proximal or distal lateral branch, microchannels or disease proximal or distal to the occlusion were not associated with procedural success.
Regarding technical factors associated with procedural success, mean catheter caliber was greater in successful than in unsuccessful procedures (6.6±1.1 vs. 6.3±1.0; p=0.032), but the use of a catheter with caliber ≥7F was not associated with success. The use of intravascular ultrasound (IVUS) was associated with success (chi-square=11.1; p=0.001), but was not a predictor when adjusted for variables of coronary anatomy. There were no associations between other technical variables and success rates, including access route or the use of contralateral contrast injection or of support catheters.
Predictors of successThe following were found to be predictors of success in univariate analysis: absence of active smoking (OR 2.02, 95% confidence interval [CI] 1.243-3.29; p=0.005); presence of tapered stump (OR 5.2, 95% CI 2.7-10.2; p<0.001); absence of significant tortuosity (OR 6.44; 95% CI 3.02-13.75; p<0.001); absence of bifurcation (OR 1.95; 95% CI 1.08-3.51; p=0.026); absence of significant calcification (OR 3.1; 95% CI 3.10-5.41; p<0.001); LAD as target vessel (OR 1.9, 95% CI 1.0-3.5; p=0.048); and CTO length <20 mm (OR 3.00, 95% CI 1.69-5.3; p<0.001).
In multivariate analysis, only anatomical factors, not clinical variables, were independent predictors of success: presence of tapered stump (OR 5.67; 95% CI 2.9-10.9; p<0.001); absence of significant tortuosity (OR 6.1; 95% CI 2.09-12.09; p<0.001); absence of bifurcation (OR 2.05; 95% CI 1.1-3.7; p=0.016); absence of significant calcification (OR 3.0; 95% CI 1.8-5.2; p<0.001); LAD as target vessel (OR 2.0; 95% CI 1.1-3.6; p=0.022); and CTO length <20 mm (OR 3.0; 95% CI 1.7-5.4; p<0.001).
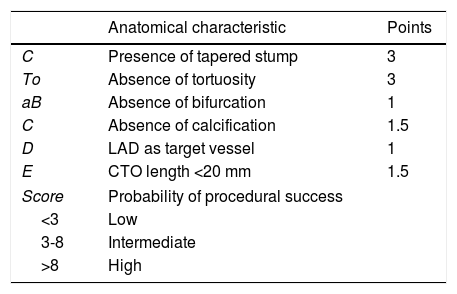
These independent predictors – tapered stump (C), absence of tortuosity (To), absence of bifurcation (aB), absence of calcification (C), LAD as target vessel (D), and CTO length (E) – were then used to create an anatomical score, the CTo-aBCDE score (Table 5).
Parameters and scoring of the CTo-aBCDE score.
| Anatomical characteristic | Points | |
|---|---|---|
| C | Presence of tapered stump | 3 |
| To | Absence of tortuosity | 3 |
| aB | Absence of bifurcation | 1 |
| C | Absence of calcification | 1.5 |
| D | LAD as target vessel | 1 |
| E | CTO length <20 mm | 1.5 |
| Score | Probability of procedural success | |
| <3 | Low | |
| 3-8 | Intermediate | |
| >8 | High | |
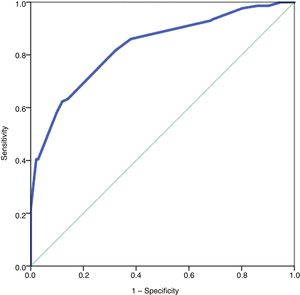
The score thus ranges from 0 to 11. It showed a high level of accuracy for predicting procedural success with a score of >5 (area under the curve [AUC] 0.831, S=79%, E=70%) (Figure 1).
A score <3 was associated with low probability of success (15%), 3-8 with intermediate probability (55%), and >8 with high probability (95%) (Figure 2).
Although it was not designed for this purpose, the J-CTO score also showed good accuracy for predicting procedural success with scores <3 (AUC 0.80, S=60%, E=86%), although inferior to the CTo-aBCDE score.12
ComplicationsThe rate of complication was 3.2% (n=12), including two deaths. Details are shown in Table 4. There was a higher risk of complications in intervention on the left coronary artery than on the right coronary artery (5% vs. 1.1%; chi-square=4.7; p=0.03), particularly for major complications (3.6% vs. 0%; chi-square 6.4; p=0.011). No other factors were associated with complications, including age, technical difficulty (as assessed by the J-CTO score), access route, type or caliber of catheters, or use of contralateral contrast injection.
DiscussionThe results of this study identified predictors of success in CTO PCI. When adjusted in multivariate analysis, only anatomical characteristics of the underlying disease were independent predictors of success. On the basis of these variables, we were able to create an easy-to-use and highly accurate score that categorizes the probability of success as high, intermediate or low.
From a methodological standpoint, it should be noted that this score was designed on the basis of data from a real-world registry in which procedures were performed by both dedicated and non-dedicated operators. As a result, femoral access, large-caliber catheters (≥7F), IVUS and contralateral contrast injection were not widely used. The possibility cannot be excluded that these factors, particularly the last, may have influenced the success rate and thereby potentially compromised the applicability of the CTo-aBCDE score.
We used statistical techniques to assess the contribution of these factors to procedural outcome. However, only the use of large-caliber catheters and of IVUS showed a slight association with success. Even cases in which contralateral injection was used had only a marginally superior success rate (61.9% vs. 59.5%; p=0.666), without statistical significance. There are several possible reasons for these findings. Cases with low anatomical complexity, almost 40% of the sample, had high success rates and were mainly performed by non-dedicated operators; support catheters, IVUS and contralateral injection are not generally used and are thus irrelevant in such cases. Furthermore, when such techniques are used, it is mainly in procedures performed by dedicated operators in cases of high complexity and hence lower success rates. Finally, anatomical characteristics were shown to be the most important factors, and so the influence of the techniques in question is considerably reduced in multivariate analysis that also includes anatomical variables. The use of contralateral injection and support catheters would thus have been more important in less simple cases, and when not used, may have played a role in lack of success (although in general anatomical factors were the main key to procedural success). It should also be noted that the overall success and complication rates were similar to those in the literature in similar circumstances.13
In view of the above, our results simply reflect the actual conditions of a real-world registry and can only be generalized to other interventional cardiology centers as a whole, rather than specifically to a CTO program. This is important, since the results can be applied not only in specific cases but in a wider context to help a center to optimize resources, maximize success and minimize complications, thereby improving clinical practice in a field in which the evidence is still limited.
Thus, a patient whose CTo-aBCDE score shows a high probability of success will, if clinically suitable, be a good candidate for intervention and the procedure can be performed by an operator who is not dedicated to treating CTOs, since the probability of success is, in a general context of an intervention unit, high with any operator.
A patient with an intermediate score may be a candidate for intervention; however, since the overall probability of success is around 50%, the procedure should preferably be performed by a dedicated operator.
Finally, a patient with a CTo-aBCDE score showing a low probability of success should be considered for conservative management, PCI by a team experienced in CTO, or surgical revascularization.
The score most widely used on a daily basis in this setting is the J-CTO score, which is also based solely on the anatomical characteristics of the lesion.14 Some of the variables used in this score are also used in the CTo-aBCDE score. Some authors suggest that the J-CTO score is a good indicator of probability of procedural success,12,15 and many operators use it to stratify risk and to aid in the decision whether to proceed with intervention. In our registry, we also saw a strong association between a J-CTO score of >2 and procedural failure.
However, the J-CTO score has several limitations. It was designed to help with the technical planning of CTO PCI, on the basis of anatomical complexity, not to assess the probability of success; the original criterion of success was guidewire crossing within 30 minutes, which is less clinically relevant than successful revascularization. It was also designed to be used in the context of a specialist CTO program, and the narrow spectrum of scoring tends to provide only a binary classification of probability (high or low), which is a limitation. In addition, the CTo-aBCDE score had better diagnostic accuracy for predicting success in our registry. For these reasons, the J-CTO score is complementary to the CTo-aBCDE score, not an alternative to it.
The PROGRESS CTO score is another well-known score used for CTO PCI and is more recent than J-CTO.14 It was specifically designed to predict technical success and was constructed using clinical and angiographic parameters. In multivariate analysis, only anatomical variables were shown to be independent predictors of success: presence of collaterals, non-ambiguous proximal cap, absence of moderate or severe tortuosity, intervention in arteries other than the circumflex, and no prior PCI. The accuracy of the PROGRESS CTO score in the validation cohort was no better than that of the J-CTO score. This fact, together with the partial overlap between the variables used in the two scores, means that the main advantage of the PROGRESS CTO score is that it was originally designed to predict success rather than procedural difficulty.
Notwithstanding the similarities between the PROGRESS CTO and CTo-aBCDE scores, there are important differences between them. The former was designed in the context of a prospective CTO registry in which the success rate was 92.9%, which limits its usefulness in the context of a general interventional cardiology center, and like the J-CTO score, it tends to provide a binary result (high or low probability of success), which reduces its stratification ability.
An analysis of the results of the CASTLE score was recently published.16 This score was derived from EuroCTO, a large European CTO registry. Although it includes two non-anatomical variables (previous coronary artery bypass grafting [CABG] and age >70 years), most predictors of procedural success were anatomical (tortuosity, extent of calcification, occlusion length and stump morphology). In addition, although one point was given for each anatomical and non-anatomical factor, the authors revealed the relative weight that each had in predicting success, and anatomical factors were of greater importance. This study thus supports the findings of the present registry, in which anatomical factors were the major predictors of success in CTO PCI.
It should also be noted that unlike CTo-aBCDE, the CASTLE score was based on a registry of CTO procedures performed at high-volume centers specializing in CTOs, and is therefore less applicable to more general centers, a limitation it shares with the other scores described above.
The clinical and lesion-related score (CL-score)17 was derived from 1671 consecutive cases of CTO PCI at a French center, performed by 14 operators and only considering first attempts. This score is methodologically the most similar to the CTo-aBCDE score, since the patient cohort did not include only cases from a specialist CTO PCI program and accordingly also demonstrated a lower success rate.
The CL-score identified two clinical characteristics associated with procedural failure, previous CABG and previous myocardial infarction (MI), as well as four anatomical predictors of failure that are common to the CTo-aBCDE score: calcification, blunt stump, non-LAD target vessel, and lesion length ≥20 mm. The presence of tortuosity was also a predictor of failure in the study on which the CL-score was based, but was not included in the model due to its lower statistical significance. The association with bifurcations was not analyzed and was therefore also not included in the score. It cannot therefore be excluded that if these two factors had been included in multivariate analysis, the weight of the clinical factors would remain significant. However, the CL-score is heavily weighted in favor of anatomical variables, and thus supports the findings on which the CTo-aBCDE score was based.
A recent large meta-analysis18 of 61 studies with almost 70 000 patients also identified predictors of success in CTOs. Although these included clinical variables (history of MI, PCI, CABG, stroke or peripheral arterial disease), anatomical variables had higher predictive value. Factors associated with procedural failure in this meta-analysis were non-LAD target vessel, moderate to severe calcification, tortuous vessel, >45° vessel angulation, blunt stump, ostial lesions, multivessel disease, and presence of bridging collaterals. These factors are very similar to those used for the CTo-aBCDE score. However, the meta-analysis does not specify whether the studies analyzed were in specialized CTO centers, and there was considerable variability in the methodology used, particularly when defining success.
The above evidence on the various scores for predicting success in CTO PCI shows that all they have in common is the inclusion of anatomical factors. The CL-score was the only one not to have been developed in the setting of a center specializing in CTOs, but it also includes non-anatomical variables, the predictive value of which is not consistently demonstrated in the various studies and meta-analyses. The results of the CTo-aBCDE score are thus overall in agreement with the existing evidence, with the advantage of being generalizable to all interventional cardiology centers.
LimitationsThis study has several limitations. It is an observational study and therefore investigator bias cannot be ruled out; it is based on a single center, which limits the sample size; and the resulting score has not been applied to a validation cohort, and so the extent to which it can be extrapolated remains to be established. We aim to advance to this stage in the near future.
Finally, as pointed out above, it cannot be excluded that technical aspects of the procedure may have contributed to success and failure rates.
ConclusionIn patients undergoing CTO PCI, only anatomical characteristics of the lesions were independent predictors of success. The CTo-aBCDE score demonstrated good accuracy and stratification ability. It may enable selection of cases that can be treated by any operator, those in which a dedicated operator will be desirable, and those with an extremely low probability of success, which should be considered individually for conservative management, surgical revascularization or PCI by a team experienced in CTO.
Conflicts of interestThe authors have no conflicts of interest to declare.