A 31-year-old woman was referred to Cardiology due to abnormal electrocardiogram (ECG) and Holter findings, after experiencing frequent paroxysms of palpitations. She reported no other symptoms. Her physical examination was unremarkable.
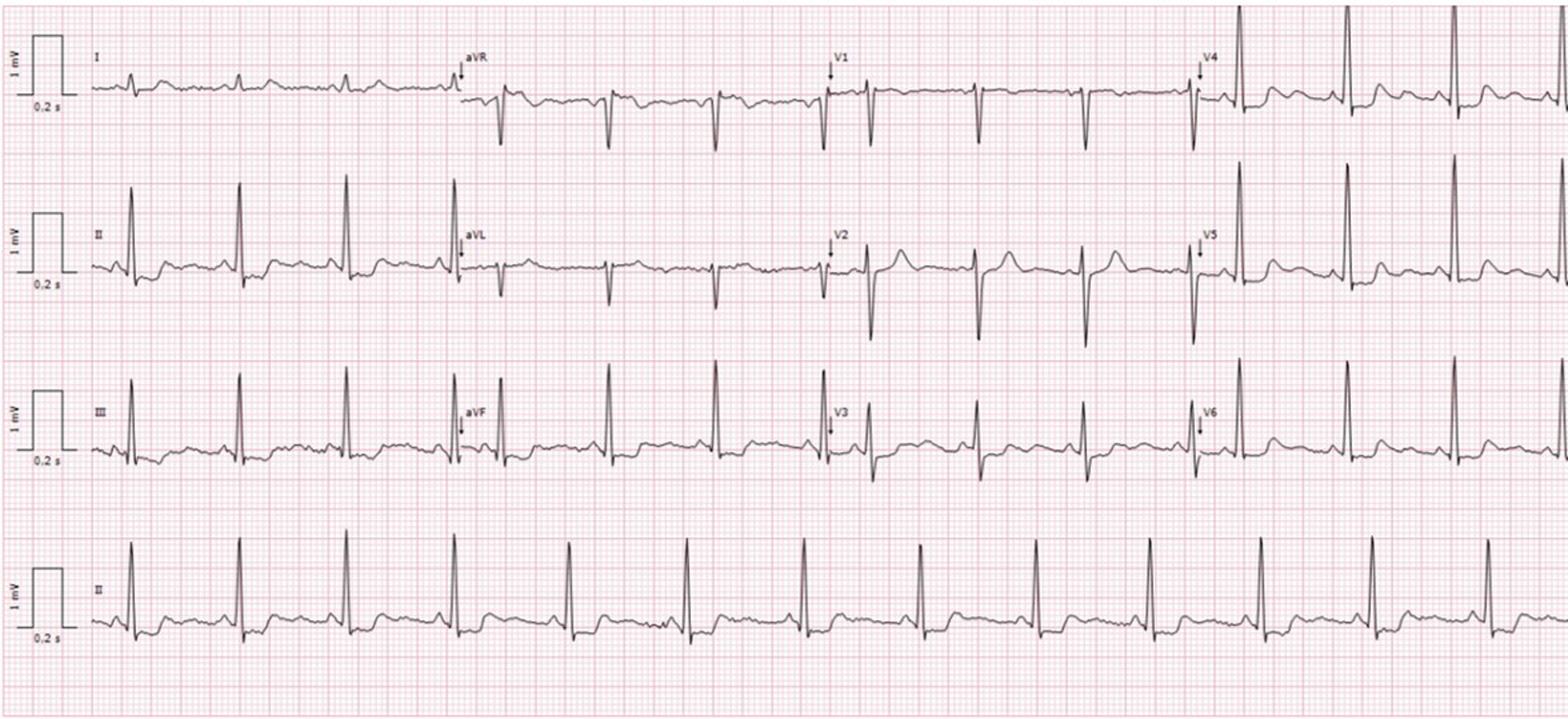
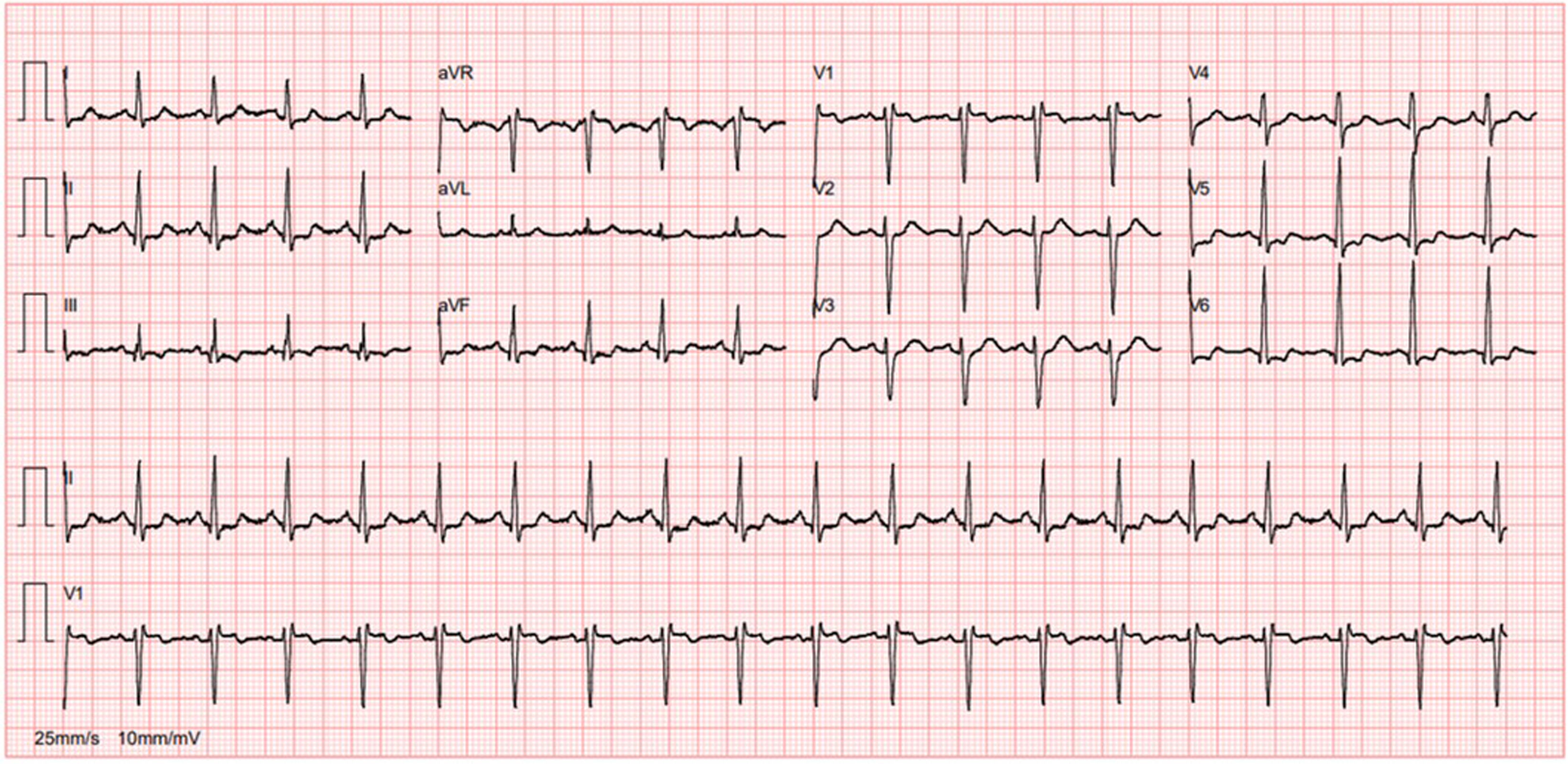
Her 12-lead ECG demonstrated sinus rhythm (SR) with concave-upward ST-segment depression in multiple leads and ST-segment elevation >0.1 mV in aVR (Figure 1). A 24-hour Holter showed SR, premature ventricular contractions (PVCs) and episodes of accelerated idioventricular rhythm.
12-Lead ECG of the patient when she was first referred to Cardiology. ECG demonstrated SR with concave-upward ST-segment depression in leads II, III, aVF, V3-6 and ST-segment elevation >0.1 mV in aVR, normal PR (120 milliseconds [ms]) and corrected QT (368 ms) intervals, normal QRS configuration and duration (73 ms).
The patient had no comorbidities, no family history of coronary artery disease (CAD) or sudden cardiac death. She was not taking any medication or drugs.
Differential diagnosisThe differential diagnosis included causes of ST-segment depression and ventricular arrhythmias, including CAD, cardiomyopathies, metabolic and pharmacological causes and primary arrhythmia syndromes.
AssessmentAn integrated sequential assessment was undertaken:
- 1.
Transthoracic echocardiogram: Normal cardiac structure and function.
- 2.
Blood tests, including electrolytes, thyroid function, and brain natriuretic peptide: Normal.
- 3.
Cardiac magnetic resonance (CMR): Excluded structural heart disease, fibrosis and scarring.
- 4.
CT coronary angiography: Excluded CAD.
- 5.
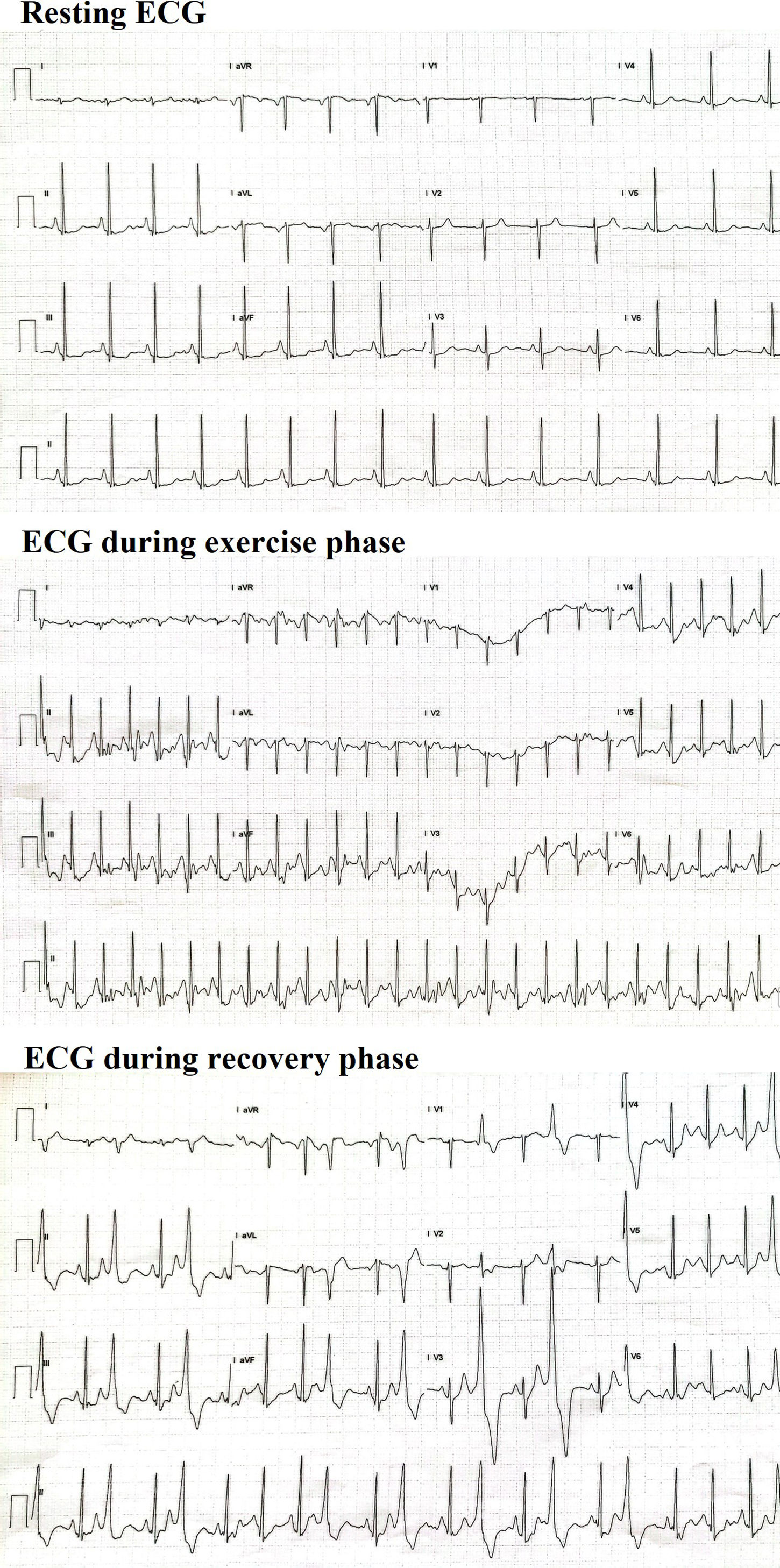
Treadmill exercise test: Dynamic accentuation of the preexisting ST-segment depressions during exercise and frequent monomorphic PVCs in recovery stage (Figure 2).
Figure 2.Treadmill exercise stress test with accentuation of preexisting ST-depressions. The preexisting ST-depressions in leads II, III, aVF, V3–V6 showed dynamic accentuation during exercise, returning to basal during recovery phase. The preexisting ST-segment elevation in aVR was also accentuated during exercise. Frequent monomorphic PVCs in the recovery stage were recorded.
(0.73MB).
Further inquiry revealed that the patient's mother had presented in the emergency department five years earlier, aged 49, complaining of palpitations and tachycardia. Her ECG showed widespread ST-segment depression, isolated PVCs, and episodes of non-sustained ventricular tachycardia. She was initially diagnosed with acute coronary syndrome due to elevated troponin levels, but coronary angiography and CMR were normal. The mother was later diagnosed with atrioventricular nodal reentrant tachycardia, which was treated successfully with catheter ablation. The follow-up ECG showed the less pronounced (but similar to her daughter's) ST-segment deviations (Figure 3).
Mother's ECG. The ECG of the patient's mother in 2017, when she attended the emergency department with palpitations, showed SR, rSr’ in lead V1, ST-depression in leads II, III, aVF, V3–V6 with reciprocal changes in aVR and V1. Follow-up ECG shows the less pronounced (but similar to her daughter's) ST-segment deviations.
Recognition of specific ECG patterns and detailed family history are crucial for diagnosing inherited arrhythmia syndromes. Bundgaard et al. described the newest one in 2018,1 familial ST-segment depression syndrome (FSTD), which is characterized by persistent, nonischemic ST-segment deviation in multiple leads, in the absence of structural heart disease, predisposing the patient to arrythmias and heart failure. Most affected individuals are asymptomatic for decades before arrhythmias occur.2–4
Familial ST-segment depression syndrome presents as persistent ECG changes, except during exercise when ST-segment deviations may worsen.1–4
Widespread ST-depression is not uncommon in clinical practice; patients will typically undergo a routine work-up including biochemistry, echocardiography, and coronary imaging. However, following normal findings, the ECG changes may be considered nonspecific and no further clinical action taken. On this basis, the above-described FSTD may have been misdiagnosed in the past, but the persistence of this pattern should prompt further investigation and family screening.3 Cases have been described in Denmark, the UK, and the Netherlands.1–4 Since optimal clinical management is still unclear, these patients should be maintained in follow-up and their symptoms treated according to general recommendations.5
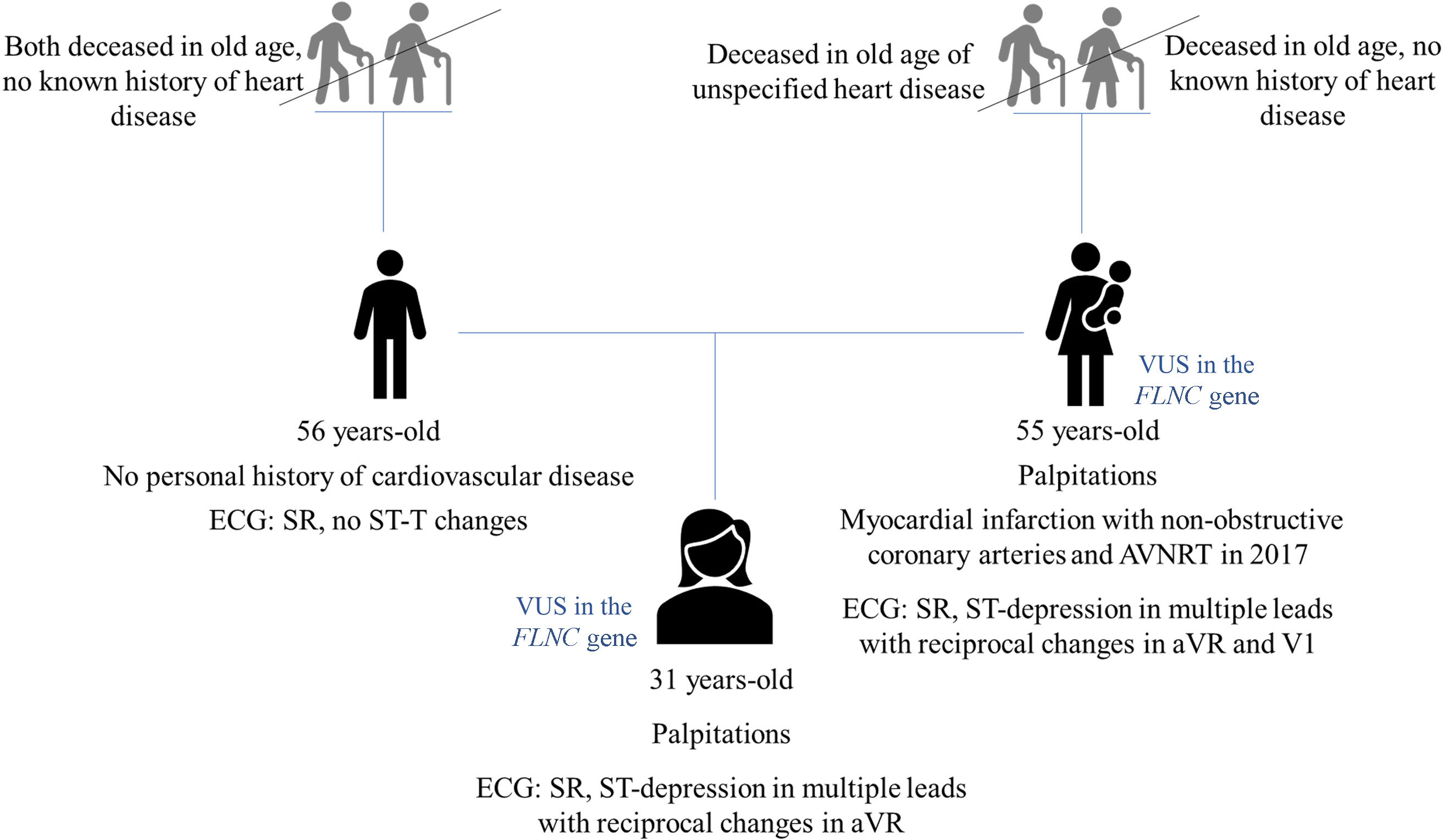
Management and follow-upOur patient has been in regular follow-up and remains less symptomatic with bisoprolol. The ECG pattern remains unchanged. Genetic testing of our patient revealed a variant of unknown significance in the FLNC gene. Her mother is a carrier of the same variant (Figure 4).
Family tree. A detailed family history revealed that the patient's mother experienced palpitations and tachycardia several years ago. Her ECG demonstrated sinus rhythm, ST-depression across multiple leads, and reciprocal changes in aVR and V1, like her daughter's findings. The maternal grandfather passed away at an advanced age due to heart disease, though specific details about his condition are unavailable. The patient is an only child, with no family history of coronary artery disease or sudden cardiac death at a young age. Both the patient and her mother share a variant of unknown significance in the FLNC gene.
This is a clinical case – ethical committee approved not required. Written consent has been obtained from all patients for publication of the clinical case.
FundingThe authors state that there was no funding.
Conflicts of interestThe authors have nothing to disclose.


![12-Lead ECG of the patient when she was first referred to Cardiology. ECG demonstrated SR with concave-upward ST-segment depression in leads II, III, aVF, V3-6 and ST-segment elevation >0.1 mV in aVR, normal PR (120 milliseconds [ms]) and corrected QT (368 ms) intervals, normal QRS configuration and duration (73 ms). 12-Lead ECG of the patient when she was first referred to Cardiology. ECG demonstrated SR with concave-upward ST-segment depression in leads II, III, aVF, V3-6 and ST-segment elevation >0.1 mV in aVR, normal PR (120 milliseconds [ms]) and corrected QT (368 ms) intervals, normal QRS configuration and duration (73 ms).](https://static.elsevier.es/multimedia/08702551/unassign/S0870255125001829/v1_202506270433/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9znTMwFdb/TnkS0koegILxs=)




