Previous follow-up studies of patients with symptoms and/or non-invasive tests suggestive of ischemia or an acute coronary syndrome and a normal coronary angiogram have reported a good prognosis.
ObjectivesThe aim of this study was to evaluate the clinical characteristics and outcome of a cohort of patients with suspected ischemic heart disease and normal coronary arteries.
MethodsA clinical follow-up was performed of 607 patients (mean age 62±11 years) with symptoms or non-invasive tests suggestive of ischemia (544) or myocardial infarction (63) and normal coronary angiography. The occurrence of major cardiac events or of readmission due to chest pain was recorded during a mean follow-up of 33.6±9.5 months after angiography.
ResultsPatients with myocardial infarction were older (65.4±11.1 vs. 61.9±10.7, p=0.05), and the majority were women (68.3%). Hypertension was reported by 65.5% of patients, diabetes by 17.9%, dyslipidemia by 58.6%, smoking by 14% and family history of coronary artery disease in 11%. During follow-up no patient died from cardiovascular causes; three patients (0.5%) suffered myocardial infarction and 50 (8.3%) had recurrent chest pain leading to emergency admission. Patients with myocardial infarction had more events (20.6%) than those referred for angiography due to symptoms and/or positive non-invasive tests for ischemia (7.4%) (log-rank chi-square test: 13.6, p<0.0005).
ConclusionThe incidence of risk factors was high. Our data suggest that patients with a normal angiogram had a good prognosis in spite of their baseline clinical presentation. A significant number of patients showed persistence of symptoms.
Estudos prévios de seguimento de doentes com sintomas e/ou testes não invasivos sugestivos de isquemia ou com síndrome coronária aguda e coronariografia normal têm revelado um bom prognóstico.
ObjetivosAvaliar as características clínicas e o resultado de um grupo de doentes com suspeita de doença cardíaca isquémica e coronariografia normal.
MétodosSeguimento clínico de 607 doentes (idade média 62±11 anos) com sintomas e/ou testes não invasivos sugestivos de isquemia (544) ou enfarte agudo do miocárdio (EAM) (63) e coronariografia normal. Registou-se a ocorrência de eventos cardíacos major ou a readmissão por dor torácica durante um período médio de seguimento de 33,6±9,5 meses após a angiografia.
ResultadosOs doentes com EAM eram mais velhos (65,4±11,1 versus 61,9±10,7, p=0,05) e a maioria mulheres (68,3%). 65,5% dos indivíduos tinham história de hipertensão, referiam diabetes 17,9%, dislipidemia 58,8%, tabagismo 14% e história familiar de doença coronária 11%. Durante o seguimento, nenhum doente morreu de causas cardiovasculares, 3 tiveram EAM (0,5%) e 50 tiveram recorrência de dor torácica causando readmissão no serviço de urgência (8,3%). Doentes com EAM tiveram mais eventos (20,6%) do que os referenciados para angiografia devido aos sintomas e/ou teste não invasivo positivo para isquemia (7,4%) (logrank chi-square=13,6, p<0,0005).
ConclusãoA incidência de fatores de risco nesta população é elevada. Os nossos resultados sugerem que doentes com coronariografia normal, independentemente da apresentação inicial, têm bom prognóstico. Um número significativo de doentes tem persistência dos sintomas.
Angina, and even acute coronary syndromes (ACS) are not always associated with the detection of angiographic lesions in epicardial coronary vessels.
The etiology of chest pain is always a clinical challenge. It can have various causes, including cardiac ischemia due to coronary atherosclerotic disease, aortic stenosis, hypertrophic cardiomyopathy or coronary vasospasm, non-ischemic cardiac conditions including pericarditis, aortic dissection or Takotsubo cardiomyopathy, and non-cardiac conditions (pulmonary embolism, musculoskeletal causes, reflux esophagitis, esophageal spasm, gastritis or psychosomatic pain). A detailed clinical history and physical examination associated with appropriate diagnostic procedures are essential for correct diagnosis and risk stratification in evaluating patients presenting with acute or chronic chest pain.
Symptoms associated with myocardial ischemia are due to an imbalance between myocardial oxygen supply and demand, which is frequently the result of coronary artery disease (CAD), characterized by significant epicardial stenosis on angiography.1 Nevertheless, the presence of normal coronary arteries does not exclude myocardial ischemia. Careful investigation may reveal other causes of myocardial oxygen imbalance and angina, such as coronary microvascular dysfunction. Although myocardial infarction (MI) is usually related to CAD, its association with normal coronary arteries is well known, with a prevalence ranging from 8 to 12%.2–9 The differences in prevalence of MI with normal coronary arteries in published studies are partly due to differences in the characteristics of the study population, such as type of MI (ST or non-ST elevation) or the inclusion of patients with near-normal coronary arteries (<50% lesions). The etiology and pathogenesis of MI with angiographically normal coronary arteries are still a matter of debate. The possible mechanisms involved include coronary vasospasm, thrombosis, embolization and inflammation, alone or in combination. Endothelial dysfunction may be an underlying common feature predisposing to the acute event.10 The endothelium plays a key role in the maintenance of vascular homeostasis, and cardiovascular risk factors promote the development of endothelial dysfunction through impairment of endothelium-dependent vasodilation and pro-coagulant/pro-inflammatory endothelial activity.11 MI with normal coronary arteries is therefore likely to be the result of multiple pathogenic mechanisms without a simple cause–effect relationship, and although most studies report a good outcome of angina and even MI in patients with normal coronary vessels, prognosis may vary according to the main underlying mechanism.10
The purpose of this study was to evaluate the clinical characteristics and outcome of a large cohort of patients with symptoms or non-invasive test results suggestive of ischemia, or admitted for myocardial infarction, with normal epicardial coronary arteries on coronary angiography.
MethodsThis was a retrospective longitudinal study based on the database of consecutive patients referred for coronary angiography in Coimbra University Hospital between January 1, 2007 and December 31, 2008.
Inclusion criteria were referral for coronary angiography for suspected CAD (angina and/or positive ischemia results on non-invasive tests) or referral for coronary angiography for suspected ACS and a normal coronary angiogram (no arterial stenosis and normal ventricular function).
Patients referred for angiography for suspected myocardial ischemia and found to have other causes of angina such as valvular disease or hypertrophic cardiomyopathy, those with coronary lesions detected on angiography, those with an initial diagnosis of ACS which was not confirmed (for example with myocarditis), and those referred for angiography due to conditions other than suspected ischemia (such as known CAD), were excluded.
Suspected ischemic myocardial disease was defined as symptoms suggestive of ischemia (angina) and/or positive results on non-invasive ischemia tests (exercise testing, myocardial perfusion scintigraphy or stress echocardiography). ACS was defined as emergency admission due to myocardial infarction or unstable angina, and myocardial infarction as symptoms and increased troponin I, with or without ST elevation on the ECG.
Patients were characterized based on age, gender, presence of cardiovascular risk factors (hypertension, diabetes, dyslipidemia, smoking, family history of CAD), history of ACS and/or ischemic stroke, and therapy before angiography. Patients who suffered MI were compared with patients with suspected CAD. Follow-up, performed by consulting medical records and/or through telephone contact, ran from the time of angiography until November 30, 2010 (mean 33.6±9.5 months).
The evaluated end-points were death and myocardial infarction (major events), revascularization procedures and hospital admission due to chest pain.
Statistical analysisQuantitative variables were expressed as mean±standard deviation and compared using ANOVA or the non-paired Student's t test. Categorical variables were expressed as frequencies and compared using the chi-square test with Fisher's exact correction.
Kaplan–Meier survival analysis was used to assess differences between event rates in the two groups.
ResultsDuring the study period 4471 coronary angiograms were performed for suspected chronic CAD and 1110 (24.8%) for suspected ACS. In accordance with the inclusion and exclusion criteria 607 (13.6%) patients were selected: 544 (12.2%) for suspected ischemia, and 63 (1.4% of the total exams and 5.7% of those performed for suspected ACS) for myocardial infarction.
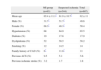
The total population had a mean age of 62±11 years, without significant differences between sexes. The MI group had a higher mean age (65.4±11.1 vs. 61.9±10.7, p=0.05) and a preponderance of females (68.3% vs. 48.3%, p=0.05) (Table 1).
Clinical characteristics of the study population.
| MI group | Suspected ischemia | Total | |
| (n=63) | (n=544) | (n=607) | |
| Mean age | 65.4±11.1* | 61.9±10.7* | 62±11 |
| Male (%) | 31.7* | 51.7* | 49.6 |
| Female (%) | 68.3* | 48.3* | 50.4 |
| Hypertension (%) | 68 | 64.9 | 65.5 |
| Diabetes (%) | 19 | 17.6 | 17.9 |
| Dyslipidemia (%) | 52 | 58.5 | 58.2 |
| Smoking (%) | 12 | 14.5 | 14 |
| Family history of CAD (%) | 6* | 11.8* | 11 |
| Previous ACS (%) | 9.5 | 5.1 | 5.6 |
| Previous ischemic stroke (%) | 3.2 | 1.7 | 1.8 |
ACS: acute coronary syndrome; CAD: coronary artery disease; MI: myocardial infarction.
Hypertension was reported by 65.5% of patients, diabetes by 17.9%, dyslipidemia by 58.6%, smoking by 14% and a family history of CAD by 11%. There were no differences in the prevalence of cardiovascular risk factors between the groups except for the presence of a family history of CAD.
The prevalence of a history of ACS was 5.6% and 1.8% had had an ischemic stroke, with no statistically significant differences between MI patients and those with suspected disease (Table 1).
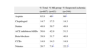
The therapy prescribed to patients before coronary angiography was also evaluated. Patients referred for angiography due to suspected cardiac ischemia were more medicated than those referred due to MI, although this difference was only significant for aspirin and nitrates (Table 2).
Therapy prescribed before coronary angiography.
| % Total | % MI group | % Suspected ischemia | |
| (n=607) | (n=63) | (n=544) | |
| Aspirin | 63.9 | 46* | 66* |
| Clopidogrel | 14.7 | 17.5 | 14.3 |
| Statins | 48.8 | 39.7 | 49.8 |
| ACE inhibitors/ARBs | 50.6 | 42.9 | 51.5 |
| Beta-blockers | 39.9 | 31.7 | 40.8 |
| CCBs | 14.8 | 14.3 | 14.9 |
| Nitrates | 20.7 | 7.9* | 22.2* |
ACE: angiotensin-converting enzyme; ARBs: angiotensin receptor blockers; CCBs: calcium channel blockers; MI: myocardial infarction.
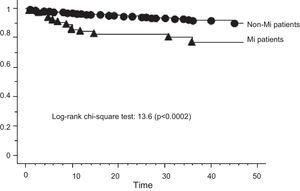
In a mean follow-up of 33.6±9.5 (max. 47) months after angiography, no patient died from cardiovascular causes, three patients had MI (0.5%) and 50 patients (8.3%) had recurrent worsening chest pain leading to emergency admission (Table 3).
Events during follow-up (mean 33.6±9.5 months).
| Total | MI group | Suspected ischemia | |
| (n=607) (%) | (n=63) (%) | (n=544) (%) | |
| Cardiac death | 0 | 0 | 0 |
| MI | 3 (0.5) | 0 | 3 (0.6) |
| Revascularization (without MI) | 0 | 0 | 0 |
| Emergency admission for chest pain | 50 (8.3) | 13 (20.6)* | 37 (6.8)* |
| Total events | 53 (8.7) | 13 (20.6)* | 40 (7.4)* |
MI: myocardial infarction.
Overall, patients with MI and a normal angiogram had more events (20.6%) than those referred because of symptoms and/or positive non-invasive ischemia tests (7.4%) (log-rank chi-square test: 13.6, p<0.0002) (Figure 1).
DiscussionAccording to our results, the outcome of patients with angiographically normal epicardial coronary arteries was generally good. In a mean follow-up of 33.6±9.5 months only three patients (0.5%) suffered MI, and none suffered other major events. However, the prevalence of chest pain and suspected myocardial ischemia leading to emergency admission was 8.3% overall and 20.6% for the MI group, suggesting considerable consumption of health care resources.
Previous studies assessing the prognosis of these patients, even bearing in mind the variability in inclusion criteria and outcomes, have generally reported excellent prognosis.
Kaski et al. studied 99 patients with microvascular angina and reported no death, MI or changes in ventricular function during a follow-up of 7±4 years.12 In a study of 160 patients, Foussas et al. reported only one sudden cardiac death and two non-fatal myocardial infarctions.13
Fournier et al. conducted a prospective study in which the clinical characteristics and evolution of a small group of patients diagnosed with MI with normal coronary arteries (n=12) were compared to those of patients with MI and significant CAD (n=75). After a mean follow-up of 41±23 months, no patient died or had a second MI in the group with normal coronary arteries, while four patients died in the group with CAD.14
The APPROACH study evaluated 9796 patients with MI who underwent angiography. Patients were divided into five subgroups according to severity of CAD: normal coronary arteries/no coronary stenosis, minor disease/<50% diameter stenosis, low-risk disease (1- or 2-vessel disease with stenoses >50%), high-risk disease (2-vessel disease with proximal left anterior descending artery or 3-vessel disease) and left main disease. Patients with normal coronary angiography (n=273, 2.8% of the population) had a mortality of 1.8% at 30 days and 4% at one year. One-year mortality was similar to the group with <50% stenosis (n=452, 2.9% mortality), but significantly lower than in the high-risk group (n=3430, 9.4% mortality) and in the group with left main disease (n=699, 19.2% mortality).15
Although our study demonstrated that this patient group has a good prognosis, it is important to bear in mind certain aspects of the study population and diagnostic procedures before angiography in patients with chronic angina.
One important point is that a significant percentage of patients (65.5%) had a diagnosis of hypertension, with implications for the results of conventional stress tests. Hypertension is one of the most common risk factors for CAD in patients undergoing exercise stress testing,16 and although imaging techniques have been shown to be more accurate than exercise tests for the diagnosis of CAD,17 myocardial perfusion abnormalities may be observed in hypertensive patients without significant epicardial CAD.18–20 Such abnormalities may not necessarily represent a false positive diagnosis of myocardial ischemia, as they may reflect microvascular disease, impaired vasodilator reserve, and increased myocardial oxygen demand in a subset of hypertensive patients.18–23 Furthermore, imaging techniques, particularly myocardial perfusion scintigraphy, can give false positive results for ischemia, especially in obese and female patients, because of attenuation artifacts, which will obviously increase the population referred for angiography.24
Inaccuracies not only in diagnostic tests but also in clinical history (failure to identify non-cardiac ischemic causes of chest pain) may influence the number of normal coronary angiograms and unnecessary exams.
One of the major concerns in patients with angina and normal coronary arteries is poor response to medical therapy. Although this analysis was not included in the present study, it is worth considering the current evidence. Kaski et al. showed that symptoms lessened in only 11% of patients, remained unchanged in 64.6%, and worsened in 24.2%.12 Lichtlen et al. demonstrated that chest pain persisted in 81% of patients and disappeared in only 19%.25 In the present study, 35.3% of patients had chest pain during follow-up leading to emergency admission. Some studies suggest the use of calcium antagonists to treat angina, because of their vasodilator effect on the microcirculation, potentially reducing cardiac work26–28 and thereby decreasing myocardial oxygen consumption. Beta-blockers have been reported to be efficacious in relieving symptoms and ST-segment depression. In a study comparing the efficacy of atenolol, amlodipine and nitrates on anginal symptoms in microvascular angina, Lanza et al. showed that only atenolol significantly reduced the number of anginal episodes.29 The effects of beta-blockers resulted in reduced myocardial oxygen demand and improved subendocardial diastolic blood flow. A pilot randomized, double-blind, placebo-controlled, crossover trial was conducted in 20 women with angina, no obstructive CAD, and ≥10% ischemic myocardium on adenosine stress cardiac magnetic resonance (CMR) imaging to evaluate the impact of ranolazine. Participants were assigned to ranolazine or placebo for 4 weeks separated by a 2-week washout. The Seattle Angina Questionnaire and CMR were evaluated after each treatment. The trial concluded that ranolazine improves angina and myocardial ischemia may also improve.30
The ideal therapy for these patients is still under investigation but effective control of risk factors with appropriate vasodilator effect on the microvascular territory will probably contribute to better quality of life.
LimitationsThis was a retrospective single-center study with all the inherent limitations. The number of patients with a diagnosis of MI was small and considering the low rate of major events, there should have been a longer follow-up period. The therapeutic measures adopted after angiography were not included in the analysis and could have improved the follow-up data.
ConclusionsThe incidence of risk factors, especially hypertension and dyslipidemia, in the study population was high. Our data suggest that patients with a normal angiogram had a good prognosis in spite of their baseline clinical presentation. However, a significant number of patients showed persistence or worsening of symptoms, indicating that morbidity remains high in these patients, despite the reassurance of a normal-appearing coronary angiogram. This is especially obvious in patients referred for angiography due to myocardial infarction. Despite the evidence of good prognosis it seems wise to control risk factors aggressively in patients with normal coronary arteries and ischemia, on the assumption that endothelial dysfunction would improve, preventing the recurrence and worsening of symptoms and disease progression. Further studies are warranted to identify the underlying pathophysiology of myocardial ischemia in the presence of normal coronary arteries and the long-term prognosis of these patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.