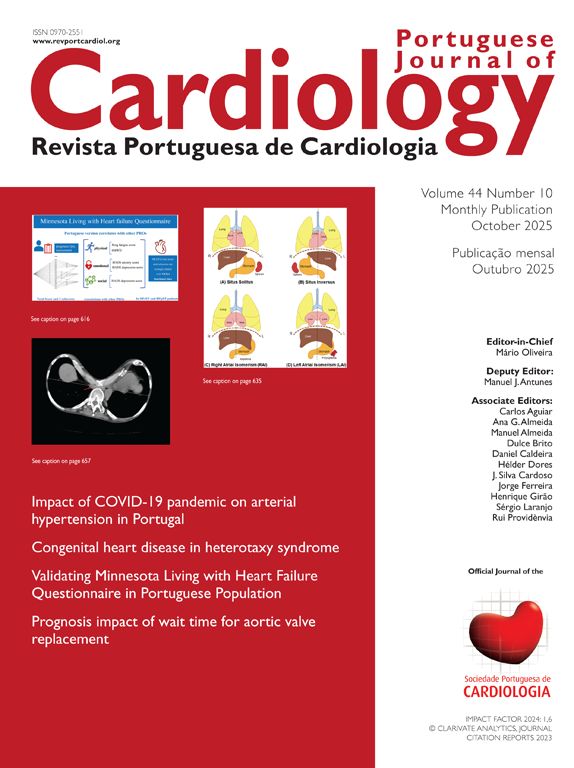
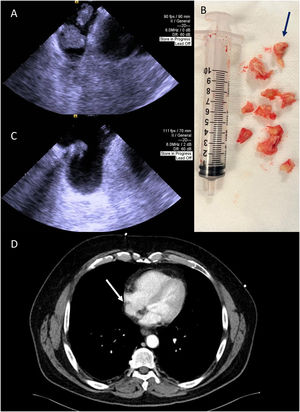
We present the case of a 60-year-old asymptomatic male patient with a medical history of rectal adenocarcinoma under chemotherapy, with a totally implantable venous access port (TIVAP). A staging computed tomography scan showed an intracardiac mass (Figure 1, Panel A) and the transesophageal echocardiography confirmed the presence of two extremely mobile masses in the right atrium, adherent to the tip of the TIVAP, the larger of the two measuring 20 mm × 20 mm (Figure 1, Panel B). Due to the patient's high risk of bleeding, anticoagulation with enoxaparin was started and, after one week, the thrombus was re-evaluated; it maintained the same dimensions and mobile appearance. After discussion in the heart team, we decided to perform a mechanical thrombectomy, with extracorporeal membrane oxygenation prepared, if needed.
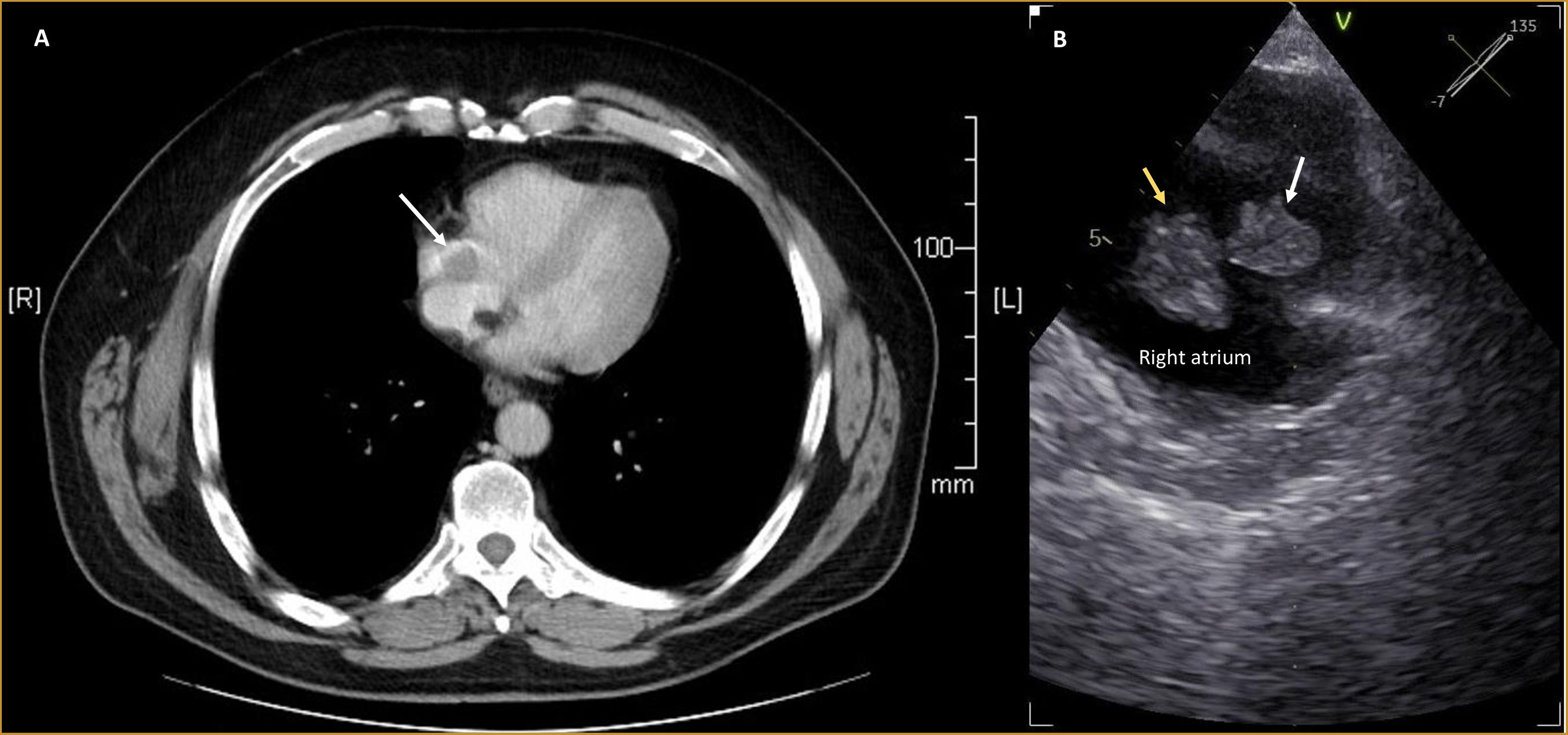
Intracardiac echocardiography (ICE) was selected to guide mechanical aspiration with the FlowTriever 24Fr System,1 as it obviates the need for transesophageal echocardiography, which may carry sedation-related hemodynamic risks.2 It was possible to remove the shorter mass and almost the totality of the larger mass, that was severely attached to the terminal part of the TIVAP (Figure 2, Panels A and B and Supplementary Videos 1–3). At the end of the procedure, a pulmonary angiography did not reveal significant perfusion defects or pulmonary hypertension. ICE showed residual thrombus attached to the terminal part of TIVAP, confirmed by CT angiography (Figure 2, Panels C and D), which also revealed fragmental thrombus in the lower lobe of the left pulmonary artery. Histological analyses confirmed the presence of chronic organized thrombus. The post-procedure course was free of complications, and the patient was discharged after four days. Anticoagulation was maintained.
Panel A: Intracardiac echocardiography used to guide mechanical aspiration showing the two masses. Panel B: The fragmented thrombus that was aspirated from the right atrium – predominantly white, compatible with the presence of fibrin (blue arrow). Panel C: Post-procedural intracardiac echocardiography image demonstrating a residual thrombus. Panel D: Thoracic CT angiography performed after the procedure showing small residual thrombus in the right atrium (white arrow).
There is a lack of consensus regarding the optimal management of right heart thrombus, especially without concurrent pulmonary embolism.3–5 Our case demonstrates that in patients considered to be at high surgical risk, large-bore aspiration thrombectomy, when guided by appropriate imaging modalities, can be technically feasible and generally safe. However, it may still be associated with potential complications, including thrombus fragmentation and embolization and incomplete thrombectomy, as demonstrated in this clinical case.
Ethical approvalOur institution does not require ethical approval for reporting individual cases or case series.
Conflicts of interestThe authors have no conflicts of interest to declare.
The following are the supplementary data to this article: