Acute myocardial infarction (AMI) is a condition that affects 12000 Portuguese individuals annually. In Portugal, disease management foresees three levels of services according to the Cardiology Referral Network. This study aims to characterize the path taken by AMI patients in Portugal after hospital treatment, at the different hospital levels. Subsequently, it aims to propose recommendations for improvements. A Steering Committee, composed of cardiology experts in AMI was responsible for the project methodology. A literature review was performed to systematize national and international AMI guidelines, followed by structured interviews of stakeholders involved in the management of these patients in seven hospitals different levels in Portugal. The study ended with a consensus meeting to analyze the results and develop recommendations. Regarding communication and liaison between hospitals in the referral network: a clear distinction was observed between hospitals in urban areas with a relatively small referral area for level 2 services versus inland hospitals, to which patients from broader areas were referred. From the point of view of communication between professionals regarding the patient's clinical information, only in level 3 hospitals in the referral network was there a greater interconnection of systems and consequent greater ease in information flows. The latter had structured cardiac rehabilitation programs, which included the integration of in-house and community facilities, in line with European Society of Cardiology recommendations. Finally, regarding the frequency of post-discharge hospital follow-up and the professionals involved, in most hospitals, follow-up was reported with the first visit at three months post-discharge, and then repeated, on average, every six months for a period between one and two years in non-atypical patients. There is high variability in the support and practices implemented to promote secondary prevention of AMI at different hospitals levels in Portugal. There is a need to review the patient pathway considering follow-up by Cardiology in the referring hospital until discharge from the consultation to a General Practitioner; implementation of Smoking Cessation Programs; Nutrition; Psychology and Physical Therapy, adjusted to the different hospital levels. Implementation of a cardiac rehabilitation program is key.
O enfarte agudo do miocárdio (EAM) afeta 12.000 pessoas anualmente, em Portugal. A nível nacional, a gestão desta doença prevê três níveis de cuidados, de acordo com a Rede de Referenciação Hospitalar de Cardiologia. Este estudo tem como objetivo caracterizar a realidade do percurso dos doentes com EAM após internamento hospitalar, nos diferentes nível de cuidados. O estudo apresenta ainda um conjunto de recomendações para a sua otimização. Foi criado um steering committee, composto por especialistas em EAM, responsável pela definição da metodologia do projeto. O estudo iniciou com uma revisão da literatura para sistematizar as diretrizes nacionais e internacionais para gestão do EAM, seguida de entrevistas estruturadas aos stakeholders envolvidos na gestão destes doentes em sete hospitais em Portugal. Terminou com o desenvolvimento de uma reunião de consenso para analisar os resultados e desenvolver recomendações. Relativamente à referenciação foi observada uma clara distinção entre hospitais urbanos, com uma área de referênciação relativamente pequena quando comparada com hospitais do interior, cujos doentes eram referenciados de zonas mais distantes. Do ponto de vista da partilha de informações clínicas dos doentes, apenas nos hospitais de nível 3 foi identificada uma maior interconexão e interoperabilidade de sistemas informáticos e consequente maior facilidade nos fluxos de informação. Estes hospitais tinham programas estruturados de reabilitação cardíaca que compreendiam um acompanhamento hospitalar comunitário, em linha com as recomendações da ESC. Finalmente, em relação à frequência do acompanhamento hospitalar pós-alta e aos profissionais envolvidos, na maioria dos hospitais, foi relatada a realização duma primeira visita três meses após a alta, repetindo-se, em média, a cada seis meses durante um a dois anos. Existe uma elevada variabilidade no suporte e nas práticas implementadas para promover a prevenção secundária do EAM nos diferentes níveis hospitalares. Há a necessidade de: otimizar o percurso do doente, garantindo o acompanhamento pela Cardiologia no hospital de referência até à referênciação para o médico de família; implementar programas de cessação tabágica; programas de nutrição; programas de psicologia e medicina física e reabilitação. A implementação de um programa de reabilitação cardíaca é fundamental para o sucesso da gestão destes doentes.
Acute myocardial infarction (AMI) is a condition that affects 12000 Portuguese individuals annually,1,2 leading to high healthcare costs and disease-related indirect costs.2,3 Although primary prevention and treatment of AMI are prominent topics in Cardiology and Public Health, there is still a long road ahead in secondary prevention in AMI patients.4
According to the 2017 Report of the National Program for Cerebrovascular diseases, the numbers associated with mortality from AMI have been decreasing since 2014. However, the focus on improving quality of life and reducing morbidity among AMI patients has the potential to contribute positively to the prevention of new events and simultaneously leads to gains in quality of life and indirect costs of the disease.2,5
Commitment to secondary prevention of AMI, including regular follow-up with patient monitoring, counseling for changing lifestyles and adherence to pharmacological therapy and cardiac rehabilitation, is associated with a reduction in post-AMI mortality, in the occurrence of new episodes of infarction and hospitalization episodes and visits to the emergency service, as well as an increase in the quality of life perceived by the patient.5
An example of the deficiencies in the follow-up of post-myocardial infarction patients is reflected in data from the Exercise Physiology and Cardiac Rehabilitation Study Group of the Portuguese Society of Cardiology. Values shared by this group indicate that, in Portugal, only 9.3% of patients participate in cardiac rehabilitation programs, compared with a European average of >30%, a number cited as an objective for the inclusion of patients in these programs.6
The Cardiology Referral Network, recommended in a document from the Directorate-General of Health,7 foresees three levels of hospital capacity with cardiology services. Level 1 includes hospitals with outpatient and in-patient cardiology consultations, which should be equipped with non-invasive cardiology diagnostic techniques. Level 2 implies the existence of a permanently available hemodynamic laboratory and a cardiology intensive care ward. Level 3, corresponding to tertiary hospitals with more valences, implies the existence of the requirements of a Level 2 hospital and the existence of a cardiac surgery service. AMI patients who can be attended in less than 120 minutes after diagnosis should be referred to a Level 2 or 3 hospital.
Thus, it is clear the relevance of investigating the current situation in Portugal regarding secondary prevention of AMI in day-to-day clinical practice conditions, as well as the importance of raising awareness among health professionals, patients, policymakers, and civil society stakeholders about the improvements that can be made in this area based on evidence and expert consensus. This study aims to characterize the reality of the path of acute myocardial infarction patients in Portugal after hospital treatment. Subsequently, it aims to compare this with the reference guidelines for secondary prevention of AMI and develop recommendations for improvements.
MethodologyA non-systematic review process was conducted to understand what is recommended for the follow-up of patients with AMI, based on national and international guidelines, including secondary prevention of AMI. The acute phase of the disease was also evaluated. The research comprised two key components: targeted research on guidelines for cardiovascular disease prevention on the websites of the European and National Cardiology Societies (ESC, SPC) and research in PubMed using search terms related to AMI.
A Steering Committee, composed of cardiology experts in AMI (Appendix 1) with recognized participation in civil society in Portugal, was responsible for the data collection methodology for following the patient's post-acute course after AMI discharge. These experts met three times, these meetings included: validation of the project methodology, the preliminary validation of the patient pathway data and specific advice on the instruments for data collection, and the final guidelines for defining the ideal patient pathway model.
To support the characterization of the national picture of patient pathway management, 12 structured interviews were performed between March and July 2022 with cardiology health professionals, including cardiologists from seven hospitals that represent levels 2 and 3 of the Cardiology Referral Network (full list included in Appendix 2), including hospitals with established cardiac rehabilitation programs. The selection of these professionals considered the geographic representation and the range of services provided by the institutions where they work. Research included hospitals at distinct levels in the referral network and health centers in their respective areas of influence. The criteria for selection were defined by the authors and considered hospitals’ willingness to participate. The interviews followed a standard script (Appendix 4) which included general and specific questions on the follow-up of patients with AMI in the healthcare institution where the professional worked (hospitals or health centers, including primary healthcare units – PHCUs – and family health units – FHUs). Domains assessed included the healthcare professional's perspective on the diagnosis, referral and follow-up of these patients at a national level, communication and interconnection of systems between hospitals and primary care at referral, and on points for improvement in the care of patients with AMI in terms of infrastructure, human resources, and health awareness. An online session was scheduled per interviewee, and the questions presented in the script were performed by the interviewer. Each interview took approximately 1 h. The answers were collected by the interviewer in an excel grid with the questions for analysis. The responses collected in these interviews were mapped and are presented aggregately due to non-disclosure purposes. The information collected allowed the elaboration of representative flowcharts of the pathway of patients after AMI treatment in multiple healthcare institutions, as well as to the construction of the representation of the ideal pathway, according to the opinions of health professionals. The latter representation was then submitted for validation by the Steering Committee at its second meeting, and the comparison between this and existing recommendations issued by medical societies is presented in the “Discussion” section of this paper.
ResultsCharacterization of the response nationallyRegarding the communication and liaison between hospitals in the referral network, for referral of patients to the various levels of the network, a clear distinction was observed between urban hospitals and inland hospitals. Urban hospitals have a relatively small referral area for level 2 services (for cardiac surgery services, this area is larger, given the small number of level 3 centers) where knowledge of the network among referring hospital professionals was good and human resources were available for patient communication and transport. At inland hospitals, to which patients from larger areas were referred, there were barriers to effective patient movement. There was a reported lack of liaison between hospitals in the network, motivated in part by the lack of knowledge of the network structure itself by the professionals responsible for referral to higher level hospitals. This scenario, combined with the shortage of physicians (who are by law required to be present in-patient transport), resulted in reported delays in access to revascularization by percutaneous coronary intervention in a hemodynamic laboratory for AMI patients.
With regard to the communication of patients’ clinical information between health professionals, only in level 3 hospitals in the referral network was there a greater interconnection among systems and consequent greater ease in information flows, as the same clinical information platform (SClinico) is used by cardiologists and general practitioners. At the remaining sites, the method used to refer patients to health centers was by letter written and printed by the cardiologist, containing the relevant discharge information, which should then be delivered by the patient to the physician or to the administrative services of the health center.
In the area of cardiac rehabilitation, a noticeable cleavage was perceived between level 2 hospitals in the inland and rural part of the country in contrast to hospitals in denser urban areas. The latter, predominantly level 3, generally had established and structured cardiac rehabilitation programs, which included the integration of in-house and community facilities, according to the ESC recommendations for structuring into program phases8,9 as reported by practitioners. The smaller geographical dispersion of patients followed in these hospitals also helped the pursuit of these programs, which facilitated logistics in the interaction between hospital, gym, and home. On the other hand, in the set of inland hospitals and covering a wider coverage area, a structured cardiac rehabilitation plan was not available; there was mention of pilot projects to be implemented, and occasional and ad hoc attempts to provide specialized counseling (by physiotherapists, for example) to the patient, still during hospitalization. In one of the hospitals in a lower-density urban area, the existence of a structured program with in-hospital and out-of-hospital phases was mentioned; however, it was discontinued due to the impact of the COVID-19 pandemic and when it was operational it had experienced low adherence due to the difficulty of travel for patients to the facilities where it was conducted.
Regarding the availability of specialists from different areas complementary to Cardiology and General Practice (especially Psychologists, Nutritionists, Physical Medicine and Rehabilitation Physicians and Smoking Cessation specialists), the national panorama was more heterogeneous. Still, hospitals with highly structured cardiac rehabilitation programs infrequently offered these valences on an individualized basis. On the other hand, services traditionally provided by GPs (smoking cessation and nutritional counseling) were more often relegated to the professionals who would necessarily be in contact with the patient (cardiologists and GPs) in the center and south regions, both in-hospital and in primary health care. The availability of psychology consultations, when available, was mainly at the level of primary care centers, with differences in the location of the consultation and time slots available.
Finally, regarding the frequency of post-discharge hospital follow-up and the professionals involved, in most hospitals, a follow-up was reported with the first visit at three months post-discharge, repeating, on average, every six months for a period between one and two years in non-atypical patients. However, these values were indicated as being highly volatile. Indeed, different values were collected with different professionals in the same hospital. In all hospitals, the possibility of referral to specialized consultations was found in case of comorbidities present after discharge from the hospital consultation (mainly heart failure and cardiac devices consultation). Only one hospital reported telephone contact with the patient between hospital discharge and the first consultation, with the purpose of assessing the relevance of anticipating the consultation in less clinically stable patients. Detailed results are presented in Appendix 5, with the feedback collected from the cardiologists and GPs in the interviews performed during the study.
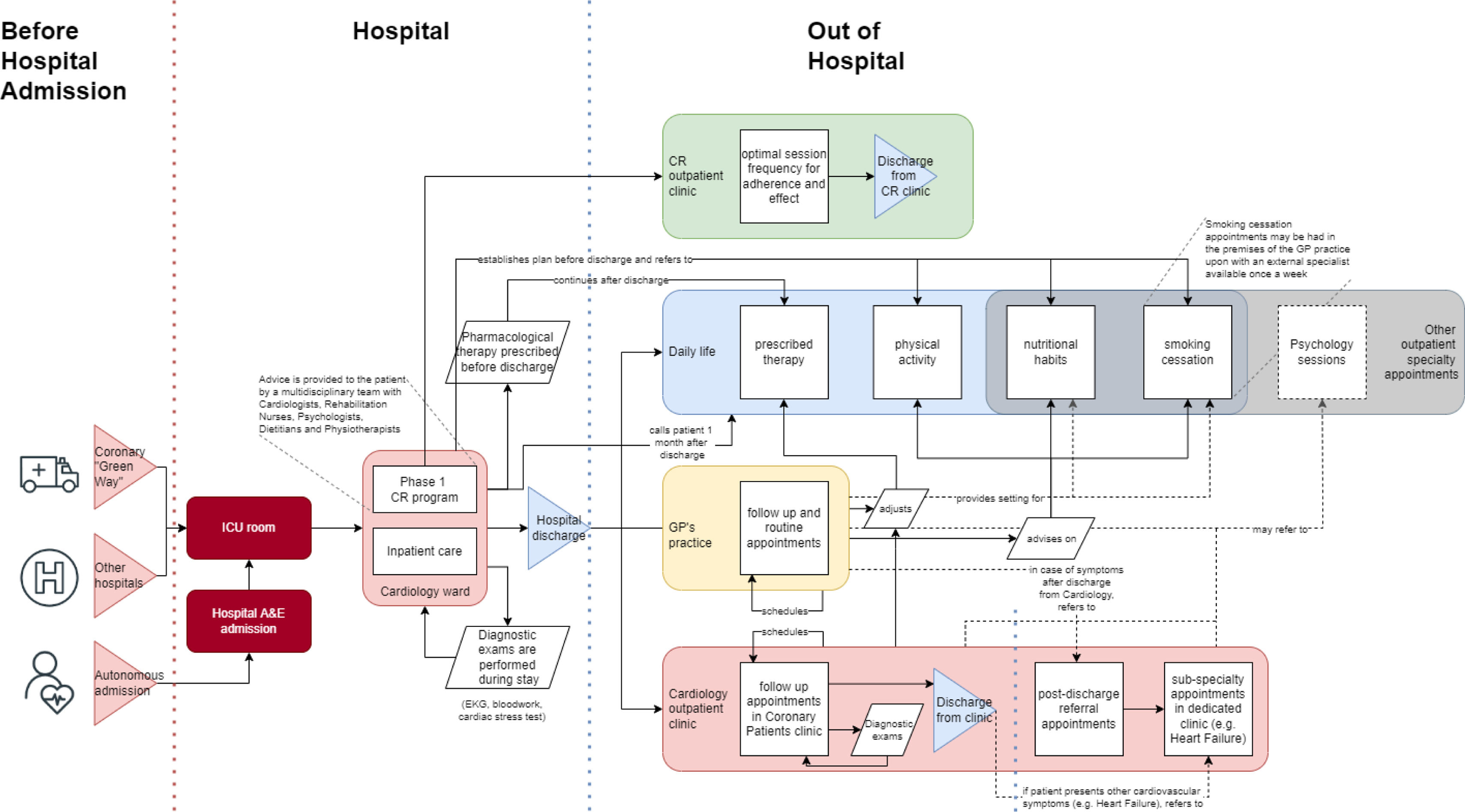
Patient pathwayAfter analysis of the interviews with health professionals and based on the research conducted, experts conceived, by consensus, an ideal model of the post-AMI patient's pathway, as presented in the flowchart in Figure 1. This pathway takes in account needs consensually stated by experts, including:
- •
The existence of a Cardiac Rehabilitation (CR) program in all hospitals with a Cardiology department with an in-hospital (Phase 1) and an out-hospital (Phase 2) phases, including exercise risk evaluation and intervention, education program, nutrition evaluation and intervention, risk factors evaluation and management (including smoking cessation, obesity and diabetes consults), medication optimization and adherence promotion and psychology evaluation and intervention components. After Phase 2, the patients should be referred to a community CR program (Phase 3) and to a General Practitioner (GP) with a referral letter. Patients should maintain regular appointments with a cardiologist according to the clinical situation.
- •
Follow-up by a GP after CR (Phase 2) discharge, along with the cardiac rehabilitation program and in direct communication with the cardiologist of the cardiac rehabilitation program. This component will place emphasis on lifestyle advice and continued cardiovascular risk factor management. It also includes continuation of the CR Program in the community (Phase 3).
- •
Possibility of referral to dedicated consultations in Nutrition, Smoking Cessation and Psychology through the CR program (Phase 3) and through the GP.
- •
Possibility of referral by the GP to specialized cardiology consultations (heart failure, arrhythmology, etc.), or others (e.g. nephrology) manifesting comorbidities.
In this pathway, the patient is admitted after traveling autonomously to the emergency department (if in existence at the hospital in question), via the Coronary Fast Track, or referral from a lower-level hospital in the Cardiology Referral Network. All these ports of entry are possible and were identified in the mapping with the hospitals.
After acute treatment, mostly focused on primary angioplasty, the patient is kept for 24–48 h in the coronary intensive care unit and then taken to the cardiology ward, where the patient remains for three to six days, if stable. During hospitalization, the parameters and doses of pharmacological therapy are optimized, and the necessary complementary diagnostic and therapeutic tests are ordered and analyzed.
Phase 1 of the CR program is also initiated, with intervention for the patient's education for lifestyle modification and risk factors management by the medical and nurse team. Early mobilization is promoted by physiotherapist and nurse. Intervention by specialists in Psychology, Nutrition, Smoking Cessation, and Physical Therapy, according to the patient's needs, can be done during hospitalization or early after discharge and hospitalization areas for this support must be available. An informed hospital discharge should be provided by a trained nurse or a cardiologist. The first Cardiology outpatient appointment and the onset of CR program (Phase 2) are also scheduled.
After clinical discharge from hospital, the patient's recovery can be grouped into four primary areas: Cardiac Rehabilitation Program, Cardiology Consultation, General Medicine Consultation and Everyday Life. In the period between discharge and the first visit, approximately in the first month, there should be a follow-up telephone contact by the Cardiology department where the patient was followed, to assess the patient's recovery and, if deemed necessary, change the priority of the first outpatient cardiology visit. This telephone contact should be performed by a cardiology nurse, to record outcomes of the first month of day-to-day life for the patient. This should be done independently from the CR Sessions and aims to question the patient on the actual experienced outcomes. In this call, a reminder should be given regarding the upcoming first post-discharge appointment.
In the CR program, according to national10 and European recommendations11 the patient enters Phase 2, which includes a clinical and functional evaluation for exercise capacity and possible limitations to exercise. The program includes CV risk factor management, the promotion of adherence to optimized treatment and modified lifestyle, a structured exercise program of two to three weekly sessions supervised by an exercise expert for an ideal period of three months (that can be extended to six months) and nutritional and psychological evaluation and intervention with a structured education program, identification of unstable cardiac situations and referral to exams and assistant cardiologist or hospital, as necessary. After this period, the patient is referred to a community institution, with a referral letter, where they can exercise and remain under surveillance (Phase 3). After Phase 2, decision to maintain dedicated consultations in Nutrition, Smoking Cessation and Psychology will depend on the patient's needs and health professional advice.
The Cardiology consultation takes place three months after hospital discharge, after Phase 2 of the CR program and is maintained with the regularity considered adequate by the attending physician for a period of one to two years in asymptomatic patients. Over follow-up, therapeutic adjustment and patient education are conducted, and it must be possible to refer patients to any of the areas highlighted above (Psychology, Nutrition, Smoking Cessation, and Physical Therapy). For a symptomatic patient, the follow-up at coronary patient consultations should be maintained. If new comorbidities are diagnosed, such as heart failure, or the need for implantation of a device (e.g., implantable cardioverter-defibrillator), the patient should be referred to a specialized consultation.
Follow-up by a GP starts when the patient goes to their usual attending physician, who has access (via computer system and/or letter) to information about the AMI event and CR program results. It is also a moment to adjust the pharmacological therapy, if necessary, and it is a vital moment for continuing patient education on lifestyles and cardiovascular risk reduction, which will be present in the patient's daily life. There should also be referrals to psychology, nutrition, smoking cessation, or other medical appointments that might be needed. Follow-up by GPs is done on an open-ended basis, and after discharge from the external cardiology consultation; GPs should be able to refer the patient back to the same or to a specialized cardiac appointment for comorbidities (e.g., heart failure) if necessary.
It is expected that the various strands of action listed above will be reflected in the patient's daily life, combining the ability to persuade the patient to adopt habits (non-smoking, healthy nutrition, increased physical activity and therapeutic adherence) and therefore reducing cardiovascular risk factors, predictors of new event, higher morbidity and higher mortality.
Discussion and conclusionThe patient's pathway perceived through the discussion with several professionals involved in the treatment and follow-up of AMI varies substantially according to multiple factors such as the region or the level of the follow-up hospital in the Cardiology Referral Network.
The data collected allowed us to identify regional and level asymmetries in the referral network with an impact on the pathway of AMI patients. In fact, level 2 hospitals in regions with lower urban density or geographically more inland were generally reported to have a lower development of CR programs and offer other specialties and health areas, as well as greater logistical and communicational difficulty in network integration, which impacted their ability to follow-up patients longer. In contrast, professional hospitals in large urban centers reported the existence of a CR program and its link to the community more frequently, as well as a more agile operation of patient referral in the network. Referral of patients to their GP, depending on the geographical distribution of the assisted population in a hospital and the consequent integration of the clinical information system of the referring hospital with that of the health centers, proved to be a preponderant factor in the way communication among professionals occurs.
Agreement among the professionals interviewed regarding the relevant elements of an adequate follow-up of post-AMI patients, reflected in the flowchart of Figure 1, suggests a relatively broad consensus on the merit of these same factors in the secondary prevention of AMI. In fact, this patient management model reflects the recommendations of the ESC,8 thus focusing on the geographical and supply asymmetries in Portugal. The assessment of the follow-up of these patients, through validated indicators, may help to quantify and better direct the efforts to implement the model presented herein, bringing the Portuguese Health System closer to the health gains listed above and improving the health of AMI patients.
The differences that were highlighted in the exploration phase appear now as barriers to the full implementation of the ideal patient pathway agreed on by the specialists. On the issues of liaison and coordination between institutions, awareness raising initiatives, as well as easy access to a map of the reference institutions in the network, may complement the necessary efforts to guarantee the availability of healthcare professionals thus enabling the smooth movement of patients throughout the network. Information flow constraints, on the other hand, may be tackled through closer integration and harmonization of Electronic Health Records systems and technologies, easing the transmission of clinically relevant data among the professionals tasked with caring for each patient. Complementarily, challenges relating to shortages of staff, infrastructure or equipment require a different and more resource-constrained approach, thus prompting the need for a discussion on health financing and management of healthcare institutions. Investment in the provision of CR centers which are accessible and have enough capacity for the demand of post-AMI patients should go hand in hand with efforts to ensure the availability of dietitians, psychologists, smoking cessation specialists and further categories of healthcare professionals whose impact on the patients’ outcomes has been demonstrated.
This study presents strengths and limitations due to its methodology. A non-systematic literature review was conducted meaning that there may be additional scientific papers that could have impacted the results presented, namely the ideal post-AMI patient pathway. Nonetheless the authors’ research covered European and National cardiac prevention guidelines and included a comprehensive PubMed research, therefore the risk of not including relevant papers is considered low. Regarding the interviews performed, the sample of hospitals only includes seven public hospitals that covered levels 2 and 3 of the Cardiology Referral Network in Portugal.12 Representative from level 1 hospitals were invited to participate in the interviews but it was not possible to obtain confirmation of their involvement. Information regarding these hospitals was provided by the Steering Committee based on their expertise. Study included hospitals from different regions in Portugal (North, Center and South) which enabled us to gain a comprehensive national view. During the study we also contacted nurses from the hospitals included in the scope of the analysis, but it was not possible to gather their input. Nurses play a relevant role in the post-AMI patient pathway and their input was mitigated with the information collected in the other interviews performed. Regarding the post-AMI patient pathway, we have presented an ideal pathway based on the research we undertook. Nonetheless there is room for further development of this ideal pathway considering other scenarios that were not explored in this research. These include home-based rehabilitation for patients who are unable to attend rehabilitation clinics and the relation between the program and the return to work in the employed population.
Conflicts of interestThe authors have no conflicts of interest to declare.