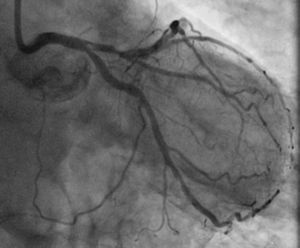
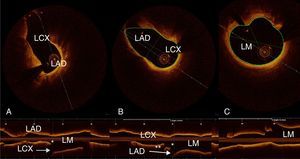
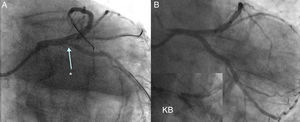
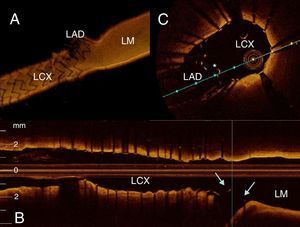
An 83-year-old man with hypertension, bilateral carotid disease, porcelain aorta and moderate renal failure was admitted with non-ST-elevation myocardial infarction. Coronary angiography revealed three-vessel disease with distal left main (LM) bifurcation involving the ostia of both the left anterior descending (LAD) and the left circumflex (LCx) coronary arteries (Medina 0,1,1; SYNTAX score 23) (Figure 1). The patient was considered unsuitable for surgery. Optical coherence tomography (OCT)-guided percutaneous coronary intervention (PCI) was undertaken. Pullbacks from the LAD and LCx (Figure 2) were obtained using frequency-domain OCT (ILUMIEN OPTIS PCI Optimization System, St. Jude Medical, St. Paul, MN). The OCT findings confirmed proximal LAD and LCx stenosis with ostial involvement, without significant disease in the LM. Moreover, the carina showed the “eyebrow” sign, indicating a risk of plaque shifting. Non-simultaneous V-stenting of both LAD and LCx was the chosen technique. After stenting the LAD (3.0/38 mm drug-eluting stent), plaque shifting to the LCx was evident on coronary angiography (Figure 3A). A 3.5/16 mm drug-eluting stent was implanted in the LCx, with final kissing balloon (Figure 3B). Pullback with real-time 3D reconstruction from the LCx revealed the V-stenting with correctly apposed struts and protruding only slightly into the LM (Figure 4).
Pullbacks from (A) left anterior descending (LAD) and (B) left circumflex (LCx) arteries with 3D reconstruction; (C) distal left main (LM) before LAD and LCx ostia showing no significant stenosis (area 12 mm2). Carina with “eyebrow” shape, leading to plaque shift (see also Figure 3). *: carina; **: marginal branch.
OCT-guided PCI in the LM is under-reported as compared to intravascular ultrasound (IVUS) and there are ongoing discussions as to whether OCT can replace IVUS in this setting. This case illustrates how OCT with its high resolution combined with real-time 3D reconstruction can be used to influence the approach to be chosen and to evaluate the final result.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.