This case report discusses an unusual presentation of ST-segment elevation myocardial infarction (STEMI) with normal coronary arteries and severe mechanical complications successfully treated with surgery. An 82-year-old man presented STEMI with angiographically normal coronary arteries and no major echocardiographic alterations at discharge. At the first month follow-up, he complained of fatigue and dyspnea, and contrast echocardiography complemented by cardiac magnetic resonance imaging revealed a large left ventricular apical aneurysm with a thrombus communicating by two jets of a turbulent flow to an aneurysmatic formation of the right ventricular apex. The patient underwent a Dor procedure, which was successful.
Ventricular septal defects and ventricular aneurysms are rare but devastating complications of STEMI, with almost all patients presenting multivessel coronary artery disease. Interestingly in this case, the angiographic pattern was normal.
O presente caso clínico discute a apresentação incomum de um enfarte agudo do miocárdio com supradesnivelamento de ST (EAMCST) com complicações mecânicas graves e artérias coronárias normais tratado cirurgicamente com sucesso. Um homem de 82 anos sofreu um EAMCST com artérias coronárias angiograficamente normais e sem alterações ecocardiográficas de relevo aquando da alta. Na consulta do primeiro mês pós enfarte, por queixas de cansaço e dispneia, realizou um ecocardiograma complementado por uma ressonância magnética cardíaca que revelaram um grande aneurisma apical do ventrículo esquerdo, com trombo, comunicando através de dois jatos de fluxo turbulento com uma formação aneurismática do ápice do ventrículo direito. O paciente foi submetido a um procedimento de Dor com sucesso.
A rutura do septo interventricular e os aneurismas ventriculares permanecem eventos raros mas devastadores com a quase maioria dos pacientes apresentado doença coronária multivaso. Curiosamente neste caso, o padrão angiográfico era normal.
In the contemporary era of primary angioplasty, mechanical complications after ST-segment elevation myocardial infarction (STEMI) such as ventricular septal defect (VSD) and ventricular aneurysm are increasingly only found in anecdotal reports. Nevertheless, the outcome remains extremely poor without prompt surgical intervention.1–5 Total occlusion of the infarct-related artery with minimal collaterals is the common underlying angiographic pattern.1,2 Only 1–12% of all acute coronary events have normal coronary arteries or non-significant coronary disease on angiography. Prognosis in this population is usually favorable without mechanical complications. Absence of coronary artery disease in postinfarction mechanical complications is extremely rare and very few cases have been reported in the literature.4,5
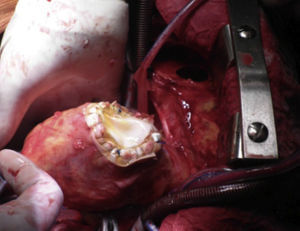
Case reportIn this report, we describe the case of an 82-year-old man, with a previous aortic valve replacement with a bioprosthesis four years previously. He was admitted for anterior STEMI with normal coronary arteries on angiography and apical ballooning. At this time the transthoracic echocardiogram (TTE) revealed a normally functioning aortic prosthesis and the apex was akinetic. He was followed at another institution where, at the first month follow-up visit, he complained of fatigue and dyspnea. TTE showed a VSD and an apical aneurysm of the left ventricle (LV) and the patient was transferred to our institution. In our department a complete TTE displayed a dilated LV, with normal global systolic function and hyperkinesia of the basal and mid segments. A large apical aneurysm was visualized with a LV to right ventricle (RV) turbulent flow suggestive of a shunt with a gradient of 90–97 mmHg (Figure 1). Contrast TTE with Sonovue® (Figure 2) and cardiac magnetic resonance imaging (Figure 3) were performed for further characterization, both showing a large LV apical aneurysm with a thrombus and a VSD with two jets of a turbulent flow to an apical RV pseudoaneurysm, also with a thrombus inside. The patient underwent corrective surgery with a Dor procedure (endoventricular circular patch plasty) combined with VSD closure and resection of the RV pseudoaneurysm (Figure 4). The procedure was successful and the postoperative course was uneventful.
Postinfarction VSD is usually associated with multivessel coronary artery disease with significant stenosis in all major vessels. In the case reported, although the angiographic pattern was completely normal, STEMI was complicated by a VSD, LV aneurysm and RV pseudoaneurysm. VSD usually occurs in the first two weeks after infarction, with a peak in the first 24 hours and between the third and fifth day post-infarction.1–3 It is associated with signs of pulmonary congestion, biventricular failure, and hypotension, which were not observed in our patient during that period. Clinical features associated with an increased risk of VSD include lack of development of a collateral network, advanced age, hypertension, anterior wall infarction and possibly fibrinolysis.5 Medical treatment is usually not effective and early surgical closure of the rupture is recommended.1 The pathophysiology, clinical characteristics, and prognosis of STEMI with angiographically normal coronary arteries are still under investigation. Smoking, cocaine abuse, hypercoagulable states, myocardial bridging, trauma, endothelial dysfunction and vasospasm, together with acute myocarditis, are among the most frequently reported causes, but none were present in this patient. Nevertheless, the apparently normal coronary arteriogram could be explained by disruption with thrombosis of a plaque at a site of outward remodeling of the artery followed by spontaneous lysis or distal embolization of the thrombus into the microcirculation after fragmentation. The compensatory enlargement or positive remodeling maintained the lumen caliber of the coronary artery affected by atherosclerosis, explaining the normal angiographic pattern.
STEMI with angiographically normal coronary arteries appears to be less severe, with fewer complications during the acute and late phases compared with infarction due to severe atherosclerotic disease.5 Although its incidence has decreased considerably since the advent of early mechanical reperfusion, STEMI complications are associated with a high rate of mortality and urgent need for early surgical repair. This case report discusses the unusual presentation of STEMI with normal coronary arteries and severe mechanical complications successfully treated with surgery.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.