Percutaneous mitral balloon valvuloplasty (PMBV) was initially described by Inoue in 1984 as a novel percutaneous technique for the management of mitral stenosis. Intracardiac echocardiography was initially used in the 1980s but was not universally accepted due to its high-frequency transducers and problems with steerability and manipulation. In the 1990s technical improvements led to more generalized use in various structural interventional procedures. We present the case of a successful PMBV guided exclusively by ICE.
A valvuloplastia mitral percutânea por balão foi inicialmente descrita por Inoue em 1984 como uma nova técnica percutânea para o tratamento da estenose mitral. A ecocardiografia intracardíaca foi inicialmente utilizada na década de 80 sem aceitação universal devido à alta frequência dos transdutores e à sua capacidade de manobra e manuseamento problemáticos. Na década de 90 melhorias técnicas conduziram à sua utilização mais generalizada em diversos procedimentos de intervenção estrutural. Os autores apresentam um caso de uma valvuloplastia mitral percutânea conduzida por ecocardiografia intracardíaca.
Percutaneous mitral balloon valvuloplasty (PMBV) was initially described by Inoue in 1984 as a novel percutaneous technique for the management of mitral stenosis.1 PMBV provides excellent immediate and mid-term results comparable to surgical mitral commissurotomy2 and is currently the standard of care for selected patients with moderate or severe mitral stenosis.3
Although PMBV can be performed by a retrograde non-transeptal technique with comparable clinical results, most North American centers use the transeptal Inoue technique due to ease of use and greater experience.4 Transeptal puncture is a critical and challenging step because of the distorted septal anatomy in most mitral stenosis patients. It commonly constitutes the longest part of the procedure and a failure or complication may terminate the case or place the patient at significant risk or subject to unnecessary long hospitalizations. Traditionally, transeptal puncture was performed using angiographic landmarks. The use of transesophageal echocardiography (TEE) has improved the safety and efficiency of the procedure and it is currently the preferred method in most North American institutions.
Intracardiac echocardiography was initially used in the 1980s but was not universally accepted due to its high-frequency transducers and problems with steerability and manipulation.5 In the 1990s technical improvements led to more generalized use in various structural interventional procedures. The first successful balloon valvuloplasty using ICE was described in 2002 by Salem.6
Case reportA 31-year-old woman with known rheumatic mitral valve disease was referred for PMVB. She had been diagnosed with rheumatic heart disease four years previously after a routine transthoracic echocardiogram (TTE) and she had been asymptomatic during her recent annual clinic visits.
Over the previous three months she had noticed progressive dyspnea on exertion limiting her daily activities. The ECG showed normal sinus rhythm with left atrial enlargement. Repeat TTE revealed progressive moderate mitral stenosis with a mean valve area of 1.2 cm2 and mild mitral regurgitation, preserved left ventricular ejection fraction (LVEF), moderate left atrial enlargement and normal pulmonary artery pressure. A treadmill stress echocardiogram with a standard Bruce protocol was ordered, during which she performed 6 METS, which was less than normal for her age. She experienced significant dyspnea towards the end of the test with no associated left ventricular wall motion abnormalities but with a mean transmitral gradient increased from 8 mmHg to 17 mmHg, consistent with severe obstruction.
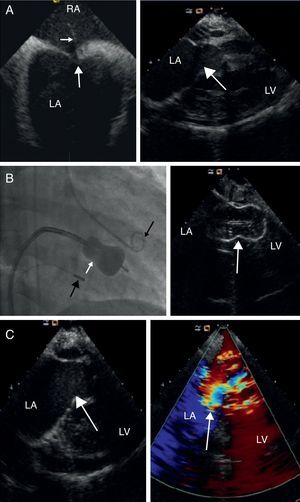
Elective PMBV was scheduled. Standard right heart catheterization was initially performed to invasively assess right heart pressures. Through a second right transfemoral venous access, the ICE catheter probe was advanced to the mid segment of the right atrium in order to visualize the atrial septum and guide the transeptal puncture. All septal borders were assessed before and during the tenting of the septum with the Mullin catheter (Figure 1A). After identification of the optimal interatrial septal position for puncture, the Brockenbrough needle and the sheath were advanced to the left atrium. With angiographic and ICE guidance the mitral valve balloon was advanced and inflated (Figure 1B). Immediate assessment of the post-procedural mitral valve morphology, transmitral valve gradient and mitral regurgitation were performed by fluoroscopy and ICE (Figure 1C).
(A) Left: ICE image showing tenting of the interatrial septum (large white arrow) with the Mullins catheter and Brockenbrough needle (small white arrow). LA: left atrium; RA: right atrium. Right: ICE 2-chamber view after insertion of the ICE probe into the right ventricle (RV). Visualization of the mitral valve (white arrow) prior to percutaneous mitral balloon valvuloplasty. Left atrial enlargement and left ventricular function and dimensions can be assessed. (B) Percutaneous mitral balloon valvuloplasty. Angiographic and ICE visualization of the inflated Inoue balloon (white arrow). ICE catheter probe (large black arrow) is located in the RV and the pig-tail catheter (small black arrow) in the left ventricle. (C) Post-PMBV ICE assessment. Left: two-dimension assessment. Right: Doppler evaluation of the mitral valve showing 1+ mitral regurgitation.
Transeptal puncture is an important skill for interventional cardiologists. The significant decrease in the incidence of mitral stenosis in the USA and the universal acceptance of echocardiography, cardiac computed tomography (CT) and cardiac MRI as alternative accurate and safe non-invasive imaging modalities have significantly decreased the number of transeptal punctures in most cardiac catheterization labs. Today fewer centers which are involved in structural heart interventions perform routine transeptal punctures and maintain their operators’ expertise.
ICE-guided structural heart disease procedures have gained increasing attention due to the ease of ICE use, the improved imaging resolution, use of Doppler and the feasibility of three-dimensional imaging applications.7 Compared to plain angiography, it achieves accurate assessment of the atrial septum and the adjacent anatomic structures, improving the safety of the puncture and the operator's level of comfort with a lower radiation exposure. Compared to TEE it eliminates the need for deeper procedural sedation, patient intubation and the involvement of an additional operator, with a probable decrease of the overall procedural cost.8
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.