Finding out which drugs are chosen to treat incident cases of hypertension may help in interpreting prevalent use of antihypertensive agents. We aimed to determine the proportion of patients who begin treatment with each antihypertensive drug class, which physicians initiate treatment and whether family physicians alter prescriptions initiated by others, and to compare the prescribing patterns of family physicians and other specialists.
MethodsIn this cohort-nested cross-sectional study between 2014 and 2015 within the Portuguese Sentinel Practice Network, family physicians notified incident cases of hypertension, reporting treatment, who issued the initial prescription and whether treatments initiated by other physicians were changed.
ResultsA total of 681 incident cases were notified. The initial prescription was issued by the patient's family physician in 86.9% of cases (95% CI: 84.2-89.3%). The most frequently used agents were angiotensin-converting enzyme inhibitors (51.3% of patients, 95% CI: 47.5-55.0%), thiazide and thiazide-like diuretics (32.2%, 95% CI: 28.8-35.8%), and angiotensin receptor blockers (21.4%, 95% CI: 18.5-24.7%). Compared to other specialists, family physicians used less beta-blockers (20.4 vs. 5.9%, p<0.001) and loop diuretics (8.2 vs. 0.8%, p=0.003). Prescriptions initiated by other specialists were changed by family physicians in 11.6% of cases (95% CI: 6.0-19.6%).
ConclusionAngiotensin-converting enzyme inhibitors were the most frequently prescribed antihypertensive class. Most diagnoses were made by the patient's own family physician. Prescriptions initiated by other specialists were usually continued by family physicians. Prescribing patterns were similar between family physicians and other specialists, except for lower use of beta-blockers and loop diuretics.
Conhecer os fármacos escolhidos para tratar os casos incidentes de hipertensão arterial ajuda a interpretar o uso prevalente de anti-hipertensores. Procurámos determinar a proporção de doentes que inicia tratamento com cada classe de anti-hipertensores, que médico inicia o tratamento, se os médicos de família alteram prescrições iniciadas por outros e comparar padrões de prescrição de médicos de família e outros especialistas.
MétodosEstudo transversal aninhado na coorte da Rede de Médicos Sentinela entre 2014 e 2015. Foram notificados casos incidentes de hipertensão arterial descrevendo o tratamento, quem fez a prescrição inicial e se os tratamentos iniciados por outros médicos foram alterados.
ResultadosNotificados 681 casos incidentes. A prescrição inicial foi feita pelo médico de família em 86,9% (IC95% 84,2-89,3%) dos casos. Os agentes mais utilizados foram inibidores da enzima de conversão da angiotensina (51,3%, IC95% 47,5-55,0%), diuréticos tiazídicos (32,2%, IC95% 28,8-35,8%) e antagonistas dos recetores da angiotensina (21,4%, IC95% 18,5-24,7%). Comparados com outros especialistas, os médicos de família utilizaram menos beta-bloqueantes (20,4 versus 5,9%, p<0,001) e diuréticos de ansa (8,2 versus 0,8%, p=0,003). As prescrições iniciadas por outros foram alteradas em 11,6% dos casos (IC95% 6,0-19,6%).
ConclusõesOs inibidores da enzima de conversão da angiotensina foram a classe mais prescrita. A maioria dos diagnósticos foi feita pelo médico de família do doente. Os médicos de família habitualmente mantiveram as prescrições iniciadas por outros especialistas. Os padrões de prescrição de médicos de família e outros especialistas foram semelhantes, exceto o menor uso de beta-bloqueantes e diuréticos de ansa.
Following the trend in developed countries, the prevalence of hypertension in Portugal is rising steadily.1 This has led to a near doubling in the use of antihypertensive drugs, in line with other OECD countries, and a corresponding increase in expenditure.2,3 A report by the Portuguese National Authority for Medicines and Health Products (INFARMED) found growing costs were mainly attributable to greater use of angiotensin receptor blockers (ARBs), despite increased use of generic medicines.2 Compared with other European countries, use of ARBs was higher in Portugal, with almost as many prescriptions for ARBs in 2011 as for angiotensin-converting enzyme (ACE) inhibitors. The same report found that primary care physicians were the prescribing source for 76% of cardiovascular medicines dispensed in outpatient pharmacies in Portugal, used more ARBs than hospitals (although less than physicians in private practice), and prescribed as many generics as hospitals and more than private practice physicians. In addition to their higher cost, ARBs are backed by weaker evidence than ACE inhibitors for reducing morbidity and mortality, although they are less likely to be discontinued due to adverse effects.4,5
Portuguese guidelines recommend thiazide or thiazide-like diuretics, ACE inhibitors, low-cost ARBs, long-acting calcium channel blockers (CCBs), or low-dose low-cost fixed-dose associations of diuretics with ACE inhibitors or ARBs as first-line therapy for patients at low to medium cardiovascular risk.6 For patients at high cardiovascular risk, low-cost fixed-dose associations of thiazide diuretics or CCBs with ACE inhibitors or ARBs are recommended. Beta-blockers are also considered appropriate as initial therapy for younger patients and those with coronary heart disease and certain arrhythmias. The European Society of Hypertension and European Society of Cardiology guidelines state that the main benefits of treating hypertension are due to lowering blood pressure, independently of which medicines are used.7 Therefore, thiazide and thiazide-like diuretics, beta-blockers, CCBs, ACE inhibitors and ARBs are all considered appropriate as first-line agents. The European guidelines recommend lifestyle changes alone for young individuals with isolated elevation of systolic blood pressure and as initial treatment for patients with grade I hypertension at low to moderate cardiovascular risk.
Most studies on antihypertensive medication prescribing focus on prevalent use.2,8–10 However, this does not enable conclusions to be drawn about how physicians choose to use each medicine: as a first-line agent, as an alternative when initial therapy results in side effects, or as an add-on treatment when the patient fails to achieve blood pressure goals.11 Focusing on incident use can determine which drugs are chosen as first-line treatment.
The prescription of ARBs and thiazide diuretics has been used as a quality indicator for primary care in Portugal since 2013.12 The implicit aim was to decrease ARB use. Although family physicians issue most prescriptions,2 it is not known how often they are responsible for initiating treatment or maintain prescriptions decided by other physicians. Specialists have been shown to influence primary care physicians by being earlier adopters of new drugs.13,14
Determining how antihypertensives are used to initiate treatment and who is responsible for their prescription can help guide efforts to improve quality of care in the Portuguese National Health Service (NHS). If family physicians have the responsibility for initiating treatment, then quality indicators targeting them may change how antihypertensives are used. If, however, most decisions are made by other physicians, targeting only family physicians will probably be ineffective.
With this study, we aimed to determine the proportion of patients with newly diagnosed hypertension who began treatment with each class of antihypertensive drug. Secondary objectives were to determine which physicians were responsible for diagnosing and initiating hypertension treatment and the proportion of cases in which family physicians altered prescriptions initiated by other prescribers, and to compare the prescribing patterns of family physicians with those of other specialists.
MethodsStudy design and settingThe Portuguese NHS is a publicly funded single-payer system, with each citizen being registered in a primary care practice and having an assigned family physician.15 Some of these family physicians participate as volunteers in the Portuguese Sentinel Practice Network,16 each of whom provides a cohort of their registered patients. This allows the network to maintain an open cohort of patients that is reasonably stable in each year and means the incidence of health problems can be calculated in this sample of the Portuguese population. The network was set up to conduct weekly surveillance of communicable and non-communicable diseases, and has also been used for observational epidemiological research to answer specific questions (satellite studies).
Between January 2014 and December 2015, the network expanded the information being reported on the incidence of hypertension for surveillance purposes, to conduct a continuous notification cross-sectional study among new cases of hypertension notified in the cohort.
ParticipantsIn 2014 and 2015 the population under observation consisted of 35535 individuals, distributed between 82 family physicians participating in the Portuguese Sentinel Practice Network. Participating physicians were asked to notify all incident cases of hypertension. Hypertension was defined using the criteria adopted by the Portuguese Directorate-General of Health (DGS) (systolic blood pressure of 140 mmHg or higher or diastolic blood pressure of 90 mmHg or higher on several separate occasions).17
MeasurementsData were collected using paper or online forms. Notifications included information on patient age at diagnosis, gender, pharmacological treatment (entered in a free text field on the paper form, which was subsequently coded by the investigators as the international nonproprietary name; the online form had a list of antihypertensive drugs available on the Portuguese market by international nonproprietary name, of which up to three could be entered), other treatment measures (free text field), who had issued the initial prescription (the family physician participating in the sentinel practice network or a different physician, who was then specified in a separate free text field; these were subsequently divided in two categories: family physicians and other specialists), and, for prescriptions initiated by other physicians, whether the notifying physician had changed the treatment. The Sentinel Practice Network coordinating team followed up any submissions with incomplete or unintelligible information, contacting the notifying physician to gather missing data.
OutcomesThe main outcome in this study was the proportion of patients who began treatment with each class of antihypertensive drug. Classes were defined using the Anatomical Therapeutic Chemical classification for antihypertensives (C02), diuretics (C03), beta-blocking agents (C07), CCBs (C08), and agents acting on the renin-angiotensin system (C09).18
Secondary outcomes were the proportion of patients for whom initial diagnosis and prescription of therapy were by family physicians (those participating in the Sentinel Practice Network or other family medicine specialists) or by other specialists (hospital and private based); the proportion of patients for whom Sentinel Practice Network physicians altered prescriptions initiated by others; and the proportion of each class of antihypertensive drugs prescribed by family physicians as opposed to other specialists.
Drugs were compared regarding use as single treatment combinations in a given patient and total use (as part of any combinations of antihypertensive therapy – alone, in fixed-dose associations or combined with the administration of other drugs as separate pills).
Study sizeTo estimate the proportion of patients beginning treatment with each class of antihypertensive drug with 5% precision and 95% confidence, assuming as a worst-case scenario that 50% of patients would begin with a given class, a minimum sample size of 384 cases of hypertension was calculated. Given the notification rates in previous years of 206 new cases of hypertension per year, we estimated that two years of continuous notifications would be needed to achieve our target sample size.
Statistical analysisProportions of each antihypertensive class prescribed as initial therapy were estimated with the respective 95% confidence interval (CI). Patient distribution regarding gender among family physicians and other specialists was compared using Fisher's exact test and age distribution was compared using the t test. Prescription patterns of family physicians and other specialists were compared using multivariate logistic regression analysis adjusting for patient gender and age. A level of significance (α) of 0.01 was used as the threshold for statistical significance to account for multiple comparisons.
Ethical approvalThe study was approved by the Ethics Committee of the Portuguese National Health Institute Doutor Ricardo Jorge.
ResultsBetween 2014 and 2015, 72 family physicians participating in the Portuguese Sentinel Practice Network notified 681 new cases of hypertension. Ten participants did not provide any hypertension notifications, but notified other health conditions, hence their patient lists were included to estimate incidence. Hypertension incidence in the cohort was 9.6/1000 person-years. Mean age at diagnosis was 57.0 years (standard deviation 13.2), and 50.1% of patients were male.
Initial diagnosis and prescription were by the patient's family physician in 592 cases (86.9%, 95% CI: 84.2-89.3%), other family physicians in 21 cases (3.1%, 95% CI: 2.0-4.7%), other specialists in 49 cases (7.2%, 95% CI: 5.5-9.4%) and physicians with unknown specialty in 19 cases (2.8%, 95% CI: 1.8-4-3%). There were no statistical differences between family physicians (Sentinel Practice Network participants and other family physicians) and other specialists (excluding unknown specialty) regarding patient age (56.7 vs. 60.4 years, p=0.058) or gender (49.1 vs. 59.2% male, p=0.19).
Pharmacological treatment was initiated in 95.5% (95% CI: 93.6-96.8%) of cases, while lifestyle changes alone were introduced in 4.4% (95% CI: 3.1-6.2%) and no treatment was reported in one notification. Among patients who were prescribed drugs, lifestyle changes were also prescribed in 50.1% (95% CI: 46.3-54.0%).
A single drug was used in 68.3% (95% CI: 64.6-71.8%) of patients who were prescribed medication, two drugs in 30.3% (95% CI: 26.9-34.0%) and three drugs in 1.4% (95% CI: 0.7-2.7%). No significant differences were found between family physicians and other specialists in the use of a single drug compared with two or more (69.5 vs. 53.1% of patients, p=0.025).
Fixed-dose associations were used in 27.9% (95% CI: 24.5-31.4%) of patients who were prescribed pharmacological treatment. No differences were seen in the use of fixed-dose associations between family physicians and other specialists (27.6 vs. 32.7% of patients, p=0.45).
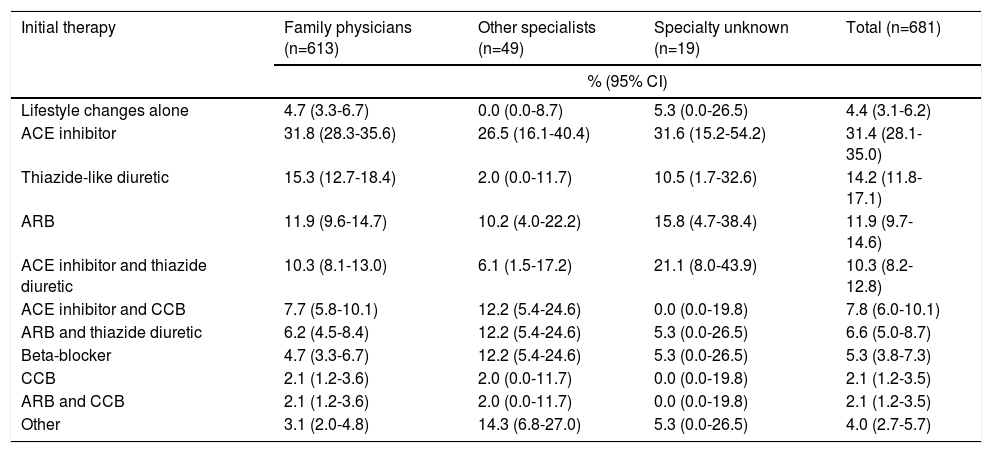
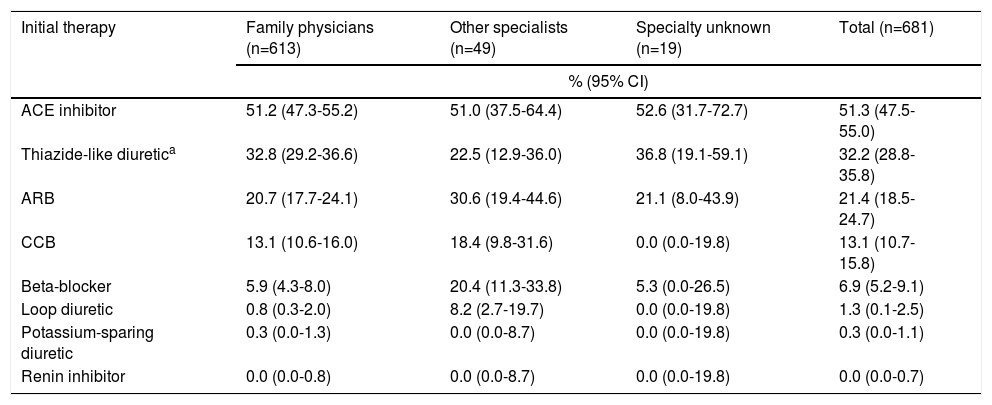
The proportions of each class of antihypertensive agents prescribed as initial therapy are shown in Table 1 (treatment combinations) and Table 2 (total use of each pharmacological class). ACE inhibitors were the drugs most often prescribed, both as single treatment (31.4% of patients) and in total (51.3%). Lisinopril was the most used ACE (32.4% of the class), followed by perindopril (26.1%) and ramipril (21.2%). There were no differences between family physicians and other specialists in the use of ACE inhibitors as single treatment (p=0.38) (Table 1) or in total (p=0.81) (Table 2).
Proportion of patients prescribed each combination of antihypertensive treatment, by class and type of physician.
| Initial therapy | Family physicians (n=613) | Other specialists (n=49) | Specialty unknown (n=19) | Total (n=681) |
|---|---|---|---|---|
| % (95% CI) | ||||
| Lifestyle changes alone | 4.7 (3.3-6.7) | 0.0 (0.0-8.7) | 5.3 (0.0-26.5) | 4.4 (3.1-6.2) |
| ACE inhibitor | 31.8 (28.3-35.6) | 26.5 (16.1-40.4) | 31.6 (15.2-54.2) | 31.4 (28.1-35.0) |
| Thiazide-like diuretic | 15.3 (12.7-18.4) | 2.0 (0.0-11.7) | 10.5 (1.7-32.6) | 14.2 (11.8-17.1) |
| ARB | 11.9 (9.6-14.7) | 10.2 (4.0-22.2) | 15.8 (4.7-38.4) | 11.9 (9.7-14.6) |
| ACE inhibitor and thiazide diuretic | 10.3 (8.1-13.0) | 6.1 (1.5-17.2) | 21.1 (8.0-43.9) | 10.3 (8.2-12.8) |
| ACE inhibitor and CCB | 7.7 (5.8-10.1) | 12.2 (5.4-24.6) | 0.0 (0.0-19.8) | 7.8 (6.0-10.1) |
| ARB and thiazide diuretic | 6.2 (4.5-8.4) | 12.2 (5.4-24.6) | 5.3 (0.0-26.5) | 6.6 (5.0-8.7) |
| Beta-blocker | 4.7 (3.3-6.7) | 12.2 (5.4-24.6) | 5.3 (0.0-26.5) | 5.3 (3.8-7.3) |
| CCB | 2.1 (1.2-3.6) | 2.0 (0.0-11.7) | 0.0 (0.0-19.8) | 2.1 (1.2-3.5) |
| ARB and CCB | 2.1 (1.2-3.6) | 2.0 (0.0-11.7) | 0.0 (0.0-19.8) | 2.1 (1.2-3.5) |
| Other | 3.1 (2.0-4.8) | 14.3 (6.8-27.0) | 5.3 (0.0-26.5) | 4.0 (2.7-5.7) |
ACE: angiotensin-converting enzyme; ARB: angiotensin receptor blocker; CCB: calcium channel blocker; CI: confidence interval.
Proportion of patients who were prescribed each class of antihypertensive drugs, by type of physician.
| Initial therapy | Family physicians (n=613) | Other specialists (n=49) | Specialty unknown (n=19) | Total (n=681) |
|---|---|---|---|---|
| % (95% CI) | ||||
| ACE inhibitor | 51.2 (47.3-55.2) | 51.0 (37.5-64.4) | 52.6 (31.7-72.7) | 51.3 (47.5-55.0) |
| Thiazide-like diuretica | 32.8 (29.2-36.6) | 22.5 (12.9-36.0) | 36.8 (19.1-59.1) | 32.2 (28.8-35.8) |
| ARB | 20.7 (17.7-24.1) | 30.6 (19.4-44.6) | 21.1 (8.0-43.9) | 21.4 (18.5-24.7) |
| CCB | 13.1 (10.6-16.0) | 18.4 (9.8-31.6) | 0.0 (0.0-19.8) | 13.1 (10.7-15.8) |
| Beta-blocker | 5.9 (4.3-8.0) | 20.4 (11.3-33.8) | 5.3 (0.0-26.5) | 6.9 (5.2-9.1) |
| Loop diuretic | 0.8 (0.3-2.0) | 8.2 (2.7-19.7) | 0.0 (0.0-19.8) | 1.3 (0.1-2.5) |
| Potassium-sparing diuretic | 0.3 (0.0-1.3) | 0.0 (0.0-8.7) | 0.0 (0.0-19.8) | 0.3 (0.0-1.1) |
| Renin inhibitor | 0.0 (0.0-0.8) | 0.0 (0.0-8.7) | 0.0 (0.0-19.8) | 0.0 (0.0-0.7) |
ACE: angiotensin-converting enzyme; ARB: angiotensin receptor blocker; CCB: calcium channel blocker; CI: confidence interval.
Thiazide and thiazide-like diuretics were the second most used drugs, with hydrochlorothiazide leading the class (43.9%; always used as part of fixed associations as it is not available as a single agent in the Portuguese market), followed by indapamide (39.4%) and chlorthalidone (16.7%). No differences were found in the use of thiazide-like diuretics as single treatment (p=0.032) or in total use (p=0.16) between family physicians and other specialists.
ARBs were the third most used drugs as single treatment (Table 1) and in total (Table 2), with losartan being used most often (30.8% of class), followed by olmesartan (20.5%), valsartan (17.8%) and telmisartan (15.1%). There were no differences between family physicians and other specialists regarding single (p=0.88) or total use (p=0.081).
CCBs were rarely used as single treatment (2.1% of patients), but they were the fourth most used class in total (13.1%), with amlodipine being the most prescribed (51.1% of class). Again, no differences were seen between family physicians and other specialists (p=0.93 for single use and p=0.44 for total use).
Beta-blockers were used by family physicians less than other specialists, both as single treatment (4.7 vs. 12.2%, p=0.007) and in total (5.9 vs. 20.4% of patients, p<0.001). Bisoprolol was the most prescribed beta-blocker (44.7% of class).
Total use of loop diuretics was also lower in primary care physicians (0.8 vs. 8.2%, p=0.003). Loop diuretics were used as single treatment in only one case. Potassium-sparing diuretics were not reported as single initial treatment, and were used in combination with other antihypertensives in only two cases. Direct renin inhibitors were not used as part of the initial treatment for hypertension.
In the 89 cases in which treatment was not initiated by physicians participating in the Sentinel Practice Network, there was a change in pharmacological treatment in 10 patients (11.6%, 95% CI: 6.0-19.6%) and information was missing for three patients (3.4%).
DiscussionMain findingsThe clear majority of patients with newly diagnosed hypertension were prescribed pharmacological treatment. Two-thirds of patients were started on a single drug, with physicians preferring, in decreasing order, ACE inhibitors, thiazide-like diuretics and ARBs. Most patients who were prescribed more than one drug were started on fixed associations, of which ACE inhibitors with thiazide diuretics or with CCBs were preferred. Loop and potassium-sparing diuretics were rarely prescribed in first-line treatments, and there were no reports of the use of direct renin inhibitors.
Most diagnoses were made by the patient's family physician. Family physicians did not differ significantly from other specialists regarding the use of most classes of antihypertensives, but used less beta-blockers and loop diuretics. When other specialists initiated therapy, it was usually continued by family physicians.
Strengths and limitationsBy prospectively collecting data within the Sentinel Practice Network cohort, we were able to gather accurate data regarding drugs being prescribed for new cases of hypertension, avoiding recall bias and administrative inaccuracies. In most cases, the physician reporting the case was the one who had made the diagnosis and therapeutic decision a few moments before. For cases in which the diagnosis had been made by other physicians, information was gathered from patients when they visited their family physicians to request refill prescriptions or for other medical problems. If needed, additional information could be gathered from the patient's national record, which allows the family physician to view details of prescriptions issued elsewhere, including by hospital and private physicians (electronic prescription has been mandatory since August 2011 to be eligible for reimbursement by the Portuguese National Health Service).19 Having this information available to Sentinel physicians greatly reduced patient recall bias in our study.
Some patients may have been diagnosed with hypertension by other physicians and not visited their family physician during the study period, and were therefore not reported to the Sentinel Practice Network. Hence, the incidence of hypertension may be underestimated and the proportion of diagnoses made by family physicians may be overestimated in our study. However, hypertension incidence was similar to that reported previously in the Sentinel Practice Network,20 and by authors in other settings.21 This suggests that under-reporting was low.
The study did not collect data on disease severity, the presence of comorbidities or contraindications to specific drugs. These could influence the choice of initial treatment, particularly under Portuguese guidelines. However, gathering such information would have increased the amount of time physicians had to dedicate to each notification and the space needed on the paper notification forms. Both would make the study unacceptable to the Sentinel Practice Network. We cannot exclude the possibility that patients with more severe clinical conditions on initial presentation, such as acute cardiovascular events or heart failure, were more often seen and managed by specialists than by family physicians. This may explain the higher prescription of beta-blockers and loop diuretics.
Yet these differences between family physicians and other specialists must be taken as hypothesis-generating only. The comparison of prescribing patterns was a secondary outcome in our study and multiple comparisons were made. Despite having used a statistical threshold of 0.01 instead of 0.05 for significance to account for multiple testing, it is still possible that these differences represent false positive results. We did not define a formal adjustment method for multiple comparisons in the study's methods since we could not have known how many combinations of antihypertensive treatments would be present in our sample. There may also have been other differences, but our study was underpowered to find them.
Although not statistically significant, there were large absolute differences between family physicians and other specialists in the proportion of men diagnosed, mean age at diagnosis, and the proportion of patients treated with a single drug. Our study may have been underpowered to find these differences, as there were relatively few cases diagnosed by other specialists.
Another limitation is that physicians who volunteer to participate in the Sentinel Practice Network may be different from other family physicians, resulting in different prescribing patterns. However, other authors have found these differences to be small.22,23 Also, given that the observed prescribing patterns for Sentinel physicians and other specialists were similar, it is unlikely that they differ significantly from those of other family physicians.
Interpretation of resultsPrevious research on prevalent use of antihypertensives had reported greater use of multiple agents, of ARBs relative to ACE inhibitors, and of diuretics, CCBs and beta-blockers.8,24 Greater use of combination therapy than in our study is to be expected, since an analysis of prevalent use will include patients with longer disease duration. More use of diuretics, CCBs and beta-blockers may be explained by the use of these agents mainly as add-on therapy when blood pressure goals are not achieved. Our study showed that ACE inhibitors were used almost two and a half times more than ARBs for initial treatment. This is different from what was observed in previous studies on prevalent use and administrative data on drug dispensing, in which ACE inhibitors were used less often than ARBs.2,8,24 Since ACE inhibitors and ARBs are seldom used in combination in the same patient, comparing prevalent use can approximate the relative proportion of patients treated with each of them. Lower prevalent use of ACE inhibitors may indicate that, after initiating treatment, a significant proportion of patients substitute them for other classes like ARBs. It is also possible that prescription patterns have changed since the previous studies and physicians are now preferring ACE inhibitors over ARBs.
Participants in the Sentinel Practice Network usually did not alter prescriptions issued by other physicians. This may be because they agree with the prescription, as our results show no major differences in prescribing patterns between family physicians and other specialists. It is also possible that family physicians feel they do not have enough information to change prescriptions initiated by specialists, the patient will continue under the responsibility of the other physician, or the patient would be resistant to change.25
Implications for practice and researchPharmacological treatment employed a large variety of drugs of different classes, and both family physicians and specialists appear to be following Portuguese and European hypertension guidelines for treating new patients.6,7 Since use of ARBs is much lower in incident than in prevalent patients, future studies should focus on how drugs are used after the initial diagnosis, particularly if ARBs are introduced because of adverse reactions, as substitutes or as add-on treatment due to failure of blood pressure control with initial therapy or for other reasons. If Portugal is to reduce use of ARBs, guidelines should include further recommendations on how to manage patients who are not adequately controlled or who experience adverse reactions with the drugs initially prescribed.
Family physicians and specialists had similar prescribing patterns, but the former were the main initiators of antihypertensive treatment. Therefore, efforts to improve quality of care in treating hypertension should be mainly directed at family physicians.
ConclusionsThe most used drug classes in incident cases of hypertension were, in decreasing order, ACE inhibitors, thiazide diuretics and ARBs. Most patients were diagnosed by the patients’ family physician, but when they were not, in most cases family physicians opted to maintain treatments initiated by other physicians. Prescribing patterns were similar between family physicians and other specialists except for lower use of beta-blockers and loop diuretics.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors thank all physicians participating in the Portuguese Sentinel Practice Network for their contributions to data collection, and also thank Inês Batista for her administrative support in the management of the Network. We are grateful to Professor Bruno Heleno for his critical review of the manuscript.