Myocardial strain analysis enables more precise assessment of cardiac performance but is relatively load dependent. New tools have been developed with afterload adjustment. Our objective was to assess myocardial work (MW) in patients with repaired aortic coarctation (rACo).
MethodsProspective study of consecutive patients with rACo who underwent a routine transthoracic echocardiogram in 2018 and 2019 at our center. Patients with significant aortic valve disease, pacemaker, or other congenital heart diseases (except for mild bicuspid aortic valve disease) were excluded. Global longitudinal strain with two dimensional speckle tracking analysis and MW were obtained (GWI:Global Work Index; GCW: Global Constructive Work; GWW: Global Wasted Work; GWE: Global Work Efficiency). Blood pressure was measured in the patient's right arm.
ResultsWe included 42 patients in the analysis, mean age of 37±10 years, 38% males. In this group, 52% had hypertension and 64% had a concomitant bicuspid aortic valve. In comparison to previously published reference values, patients with rACo had significantly lower GWI (1807 vs. 1896 mmHg%) and GCW (2173 vs. 2232 mmHg%) (p<0.001), particularly in males. Systolic blood pressure is an independent predictor for GWI (β=0.432) and for GCW (β=0.534) and GLS an independent predictor of all MW parameters (β>0.594). Neither age nor gender were independent predictors.
ConclusionsIn patients with rACo, there are some signs of left ventricular dysfunction with a reduction in GCW and GWI and with preserved GWE, despite normal ejection fraction and strain.
O strain miocárdico permite uma avaliação mais precisa da função cardíaca, mas é relativamente dependente da carga. Existem novas ferramentas para ajuste da pós-carga. É nosso objetivo avaliar o trabalho miocárdico (TM) em doentes com coartação da aorta tratada (rCAo).
MétodosEstudo prospetivo de doentes consecutivos com rCAo submetidos a ecocardiograma transtorácico de rotina em 2018 e 2019 no nosso centro. Doentes com doença valvular aórtica significativa, pacemaker ou outras cardiopatias congénitas (com exceção de doença valvular aórtica bicúspide ligeira) foram excluídos. Analisou-se o strain global longitudinal por speckle-tracking e obtido o TM (Índice trabalho global - GWI, Trabalho construtivo global - GCW, Trabalho desperdiçado global - GWW - e Eficiência do trabalho global - GWE). A pressão arterial foi avaliada simultaneamente.
ResultadosIncluímos 42 doentes, com 37 ± 10 anos, 38% do sexo masculino. Destes, 52% eram hipertensos e 64% tinham válvula aórtica bicúspide. Em comparação com os valores de referência previamente publicados, os doentes com rCAo têm menor GWI (1807 vs. 1896 mmHg%) e GCW (2173 vs. 2232 mmHg%) (p<0,001), particularmente nos homens. A pressão arterial sistólica é um preditor independente para GWI (β=0,436) e para GCW (β=0,534) e o GLS é preditor de todos os parâmetros de TM (β>0,594). Nem a idade nem o género são preditores de TM.
ConclusõesEm doentes com rCAo, existem alguns sinais de disfunção ventricular esquerda, com redução do GCW e do GWI, com GWE preservada, apesar de ainda terem normal fração de ejeção e strain.
In recent years, myocardial strain has emerged as a very useful and reliable tool for function analysis, not only of the left ventricle (LV) but also of right ventricle and atrial function. It can detect subclinical myocardial disease, when LV ejection fraction is still in the normal range, and for that reason it is particularly useful for LV function assessment. However, some limitations still exist for strain because it is also load dependent.1–4 In fact, strain can be reduced in response to increased afterload, leading to misinterpretations of the true contractile function.2,4
Myocardial work (MW) can be assessed invasively from LV pressure – volume loops. Pressure-strain loops can be used for the same purpose. However, this analysis has been not implemented in clinical practice due to its invasive nature. In recent years, non-invasive techniques have been developed to obtain LV pressure-strain loops. This tool is presently included in new echocardiographic software, and it is easy to perform in clinical practice.5 It has the advantage of being less load dependent and it can be used as an additional tool in strain analysis when assessing LV function. It considers both deformation and afterload. The combination of LV strain data and non-invasively estimated pressure curves allows estimation of MW by the area within the pressure-strain loop. It has been previously shown that all these parameters have excellent correlation both for intra- and inter-observer variability.6
This non-invasive method has been used in research in several areas, such as acute coronary syndromes, hypertension, dilated cardiomyopathy, and response to cardiac resynchronization therapy or to new drugs.2,6–10 It was our objective to assess LV function in adult patients with repaired aortic coarctation (rACo), a condition associated with long-standing increased afterload.
MethodsPopulationThis is a single-center, prospective and observational study, including all consecutive adult patients (aged ≥18 years) with rACo followed at the outpatient congenital heart disease clinic at our hospital, and referred for a routine follow-up transthoracic echocardiogram in 2018 and 2019. Patients with LV systolic dysfunction (LV ejection fraction <51% and global longitudinal strain (GLS) >-17%), significant aortic valve disease (such as aortic valve prosthesis, more than mild aortic sclerosis – defined by a peak gradient >15 mmHg – or more than mild regurgitation), atrial fibrillation, pacemaker or other congenital heart diseases were excluded. Because having a bicuspid aortic valve is a very frequently associated with aortic coarctation, patients with bicuspid aortic valves were also included, but only if peak transvalvular gradient was <15 mmHg. Patients with suboptimal image quality for myocardial deformation analysis were also excluded. Clinical characteristics were collected by review of the electronic medical record. The study complies with the Declaration of Helsinki and all patients gave their informed consent.
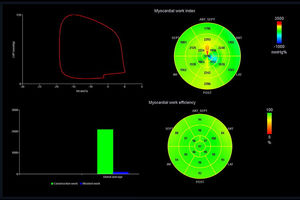
Echocardiographic studyA complete and comprehensive transthoracic study was performed using a Vivid E95™ or a Vivid 9™ ultrasound equipment (GE Healthcare) with a 3.5 MHz transducer. Patients were scanned in the left lateral decubitus position. All recordings and measurements were made according to the European Association of Cardiovascular Imaging guidelines.11–14 For strain analysis, images were acquired in apical four, two and three-chamber views, and the transducer settings of the B-mode image were adjusted to achieve a frame rate of at least 55 frames per second (fps) (preferably set at 60-80 fps) to assess GLS by speckle tracking echocardiography. The grayscale definition was adjusted whenever necessary to optimize two dimensional (2D) endocardial and myocardial definitions and images were stored in digital cine-loops with three sequential beats for offline analysis. Strain was analyzed using 2D speckle tracking in a semiautomated process and peak systolic longitudinal strain was synchronized with the QRS complex of the ECG. Blood pressure was simultaneously measured with the patient in a left lateral decubitus position, on the patient's right arm (brachial blood pressure) with an automatic sphygmomanometer. Peak systolic LV pressure was assumed to be equal to the peak arterial pressure. MW was estimated using a commercially available software package (EchoPAC™ workstation, version 203, GE) that derived non-invasive pressure-strain loops (Figure 1). MW was used to assess the work during shortening in systole and negative work during lengthening in isovolumetric relaxation (global constructive work (GCW)), the negative work during lengthening in systole and the work during shortening in isovolumetric relaxation (global wasted work (GWW)), global work efficiency (GWE)=GCW/(GCW+GWW) 100%] and global work index ((GWI) – total work within the area of the LV pressure-strain loop calculated from mitral valve (MV) closure to MV opening). Measurements were taken by a single operator. Results were compared to previously published reference values obtained in a large cohort of healthy volunteers.15,16
Statistical analysisContinuous variables are reported as mean or median and standard deviation or interquartile range, as appropriate. Categorical variables are reported as percentages. Differences between groups were tested with the chi-square test or Fisher's exact test, as appropriate for categorical variables. Student's t-test or Mann-Whitney test were used to compare continuous variables. Reference data presented as median and interquartile range or 95% confidence interval were transformed into mean and standard deviation whenever normality was confirmed with the methods proposed by Luo and Shi.17,18 Independent predictors of MW parameters were assessed by univariate and multivariable linear regression analysis. All variables with a p<0.10 in univariate analysis were included in the multivariable model. IBM SPSS Statistics software, version 26 (IBM SPSS Inc, Chicago, IL) and Primer of Biostatistics™ were used for statistical analysis. All statistical tests were two-tailed with a critical value of 0.05 for statistical significance.
ResultsWe included a total of 42 patients, with a mean age of 37±10 years (24 to 66 years), 38% males. Mean age for intervention was 12±10 years (0-45 years), mostly with surgery, and only four patients (9.5%) were treated percutaneously, with aortic stent implantation. Percutaneous re-intervention was necessary in six patients (14.3%) with a median time of 18 years between interventions, due to residual significant aortic gradient at the site of coarctation. In our population, 52.4% had hypertension, and were on specific medication and 64.3% had bicuspid aortic valve with mild disease. Table 1 shows baseline and main echocardiographic characteristics of the patients with rACo. In 18% of the patients, the ascending thoracic aorta showed mild dilation.
Baseline characteristics of patients with repaired aortic coarctation.
| Variables | Totaln=42 | Malesn=16 | Femalesn=26 | p-value |
|---|---|---|---|---|
| Age (years) | 37±10 | 39±10 | 36±10 | 0.431 |
| BSA (kg/m2) | 1.7±0.2 | 1.8±0.2 | 1.6±0.2 | <0.001 |
| SBP (mmHg) | 119±14 | 118±11 | 120±15 | 0.597 |
| DBP (mmHg) | 67±8 | 70±9 | 65 ± 7 | 0.046 |
| Hypertension (%) | 52 | 75 | 39 | 0.021 |
| Medication (%) | ||||
| RAAS blockers | 45 | 75 | 27 | 0.002 |
| Betablockers | 31 | 38 | 27 | 0.471 |
| Calcium Chanel Blockers | 12 | 9 | 8 | 0.275 |
| Echocardiographic data | ||||
| Bicuspid aortic valve (%) | 64 | 62 | 66 | 0.850 |
| LVEDD/BSA (mm/m2) | 28.5±3.7 | 27.3±38 | 29.5±3.5 | 0.060 |
| IVS (mm) | 9.1±1.9 | 10.4±1.6 | 8.3±1.6 | <0.001 |
| PWT (mm) | 8.4±2.0 | 9.4±1.7 | 7.7±1.8 | 0.005 |
| LV mass index (g/m2) | 91±25 | 100±18 | 81±27 | 0.071 |
| Left ventricular hypertrophy (%) | 32.0 | 50.0 | 15.4 | 0.074 |
| LAVi (mL/m2) | 26.1±7.0 | 24.1±7.1 | 27.3±6.8 | 0.157 |
| E (cm/s) | 100±17 | 91±15 | 105±17 | 0.014 |
| E/A | 1.3 (1.2-1.6) | 1.2 (1.0-1.5) | 1.4 (1.3-1.7) | 0.073 |
| E/e’ | 9.5±3.2 | 8.7 ± 3.0 | 10.0±3.4 | 0.203 |
| TAPSE (mm) | 23±4 | 23±3 | 22±4 | 0.450 |
| Tricuspid s’ (cm/s) | 13±2 | 13±2 | 13±2 | 0.502 |
| Aortic valve peak velocity (m/s) | 1.59±0.41 | 1.50±0.44 | 1.64±0.40 | 0.287 |
| Aortic valve peak gradient (mmHg) | 9.0 (6.8-13.3) | 7.5 (5.3-13.7) | 10.0 (8.5-13.2) | 0.065 |
| Descending aorta peak gradient (mmHg) | 18.5 (11.0-25.5) | 13.5 (11.0-19.0) | 21.5 (11.0-35.0) | 0.242 |
| GLS (%) | -19.5±2.5 | -18.9±4.1 | -19.9±2.5 | 0.335 |
| GWI (mmHg%) | 1807±406 | 1740 ± 418 | 1847±401 | 0.413 |
| GCW (mmHg%) | 2173±413 | 2043±396 | 2252±411 | 0.113 |
| GWW (mmHg%) | 78.5 (55.0-190.0) | 62 (37-175) | 91 (70-191) | 0.083 |
| GWE (mmHg%) | 95.5 (91.0-97.0) | 96 (90-98) | 95 (91-96) | 0.254 |
BSA: body surface area; DBP: diastolic blood pressure; GCW: global constructive work; GLS: global longitudinal strain; GWE: global work efficiency; GWI: global work index; GWW: global wasted work; IVS: interventricular septum thickness; LAVi: left atrial volume indexed; LVEDD: left ventricular end-diastolic diameter; PWT: posterior wall thickness; RAAS: renin angiotensin aldosterone system; SBP: systolic blood pressure; TAPSE: tricuspid annular plane excursion.
Compared to the reference population, our study group was younger and had lower body surface area (BSA), lower diastolic blood pressure (DBP) but higher systolic blood pressure (SBP) (Table 2). Regarding echocardiographic data, LV mass index, E wave velocity, and E/e’ ratio weere significantly higher and left atrial volume index (LAVi) was similar, as well as GLS. Patients with rACo showed reduced GWI and GCW, but similar GWW and GWE.
Comparison with reference values.
| RACon=42 | Reference values*n=226 | p-value | |
|---|---|---|---|
| Age (years) | 37±10 | 45±13 | <0.001 |
| Males (%) | 38 | 38 | NS |
| Body Surface Area | 1.7±0.2 | 1.8±0.2 | <0.001 |
| Systolic blood pressure (mmHg) | 119±14 | 116±12 | <0.001 |
| Diastolic blood pressure (mmHg) | 67±8 | 73±8 | <0.001 |
| LV mass index (g/m2) | 91±25 | 71±17 | 0.006 |
| LAVi (mL/m2) | 26.1±7.0 | 25.9±6.0 | NS |
| E wave (cm/s) | 100±17 | 76±16 | <0.001 |
| E/A | 1.3 (1.2-1.6) | 1.3 (1.0-1.6) | NS |
| E/e’ | 9.5±3.2 | 6.4±1.7# | 0.002 |
| GLS (%) | -19.5±2.5 | -21.0±3.3 | NS |
| GWI (mmHg%) | 1807±406 | 1896±308 | <0.001 |
| GCW (mmHg%) | 2173±413 | 2232±331 | <0.001 |
| GWW (mmHg%) | 78.5 (55.0-190.0) | 78.5 (53.0-122.0) | NS |
| GWE (mmHg%) | 95.5 (91.0-97.0) | 96.0 (94.0-97.0) | NS |
GCW: global constructive work; GWE: global work efficiency; GWI: global work index; GWW: global wasted work; LAVi: left atrial volume index; rACo: repaired aortic coarctation.
As in previous studies MW has been reported to differ according to gender, and because in our study group more than 60% were females, a separate analysis was performed for each gender. Males with rACo had a significantly higher BSA, DBP and more hypertension (more often treated with renin angiotensin aldosterone system blockers), compared with women (Table 1). Regarding echocardiographic parameters, males had lower indexed LV diastolic dimensions and higher wall thickness, with a trend toward higher LV mass index and hypertrophy. Except for E wave velocity, that is higher in females, all the other LV diastolic parameters, GLS and MW were not significantly different, but a trend was apparent for higher GWW in females.
In a direct comparison with the reference group, males with rACo were younger, with lower DBP compared to the reference group (Table 3). BSA and SBP are similar. The echocardiographic differences identified are a higher E/e’ ratio and a trend to higher E wave velocity (p=0.059). There is a reduction in GWI, GCW and GWW with similar GWE. In females, age, BSA and DBP are significantly lower and SBP, E wave velocity and E/e’ ratio substantially higher in comparison to reference population. In MW analysis, they have similar GCW and increased GWW, with a slightly (non-significantly) lower GWE, and lower GWI.
Comparison with reference values according to gender.
| Males | Females | |||||
|---|---|---|---|---|---|---|
| RACon=16 | Reference values*n=85 | p-value | rACon=26 | Reference values*n=141 | p-value | |
| Age (years) | 39±10 | 45±13 | <0.001 | 36±10 | 44±13 | <0.001 |
| BSA (kg/m2) | 1.8±0.2 | 1.8±0.2 | NS | 1.6±0.2 | 1.7±0.1 | <0.001 |
| SBP (mmHg) | 118±11 | 116±12 | NS | 120±15 | 113±12 | <0.001 |
| DBP (mmHg) | 70±9 | 73±8 | 0.002 | 65±7 | 72±9 | <0.001 |
| LAVi (mL/m2) | 24.1±7.1 | 26.1±6.2 | NS | 27.3±6.8 | 25.7±6.1 | NS |
| E wave (cm/s) | 91±15 | 72±16 | 0.059 | 105±17 | 79±16 | 0.001 |
| E/A | 1.2 (1.0-1.5) | 1.3 (1.0-1.6) | NS | 1.4 (1.3-1.7) | 1.3 (1.0-1.6) | NS |
| E/e’ | 8.7±3.0 | 5.9±1.4# | 0.012 | 10.0±3.3 | 6.7±1.6# | <0.001 |
| GLS (%) | -18.9±4.1 | -20.5±1.9 | 0.285 | -19.9±2.5 | -21.3±3.9 | 0.450 |
| GWI (mmHg%) | 1740±418 | 1849±295 | 0.004 | 1847±401 | 1924±313 | 0.011 |
| GCW (mmHg%) | 2043±396 | 2228±295 | <0.001 | 2252±411 | 2234±352 | NS |
| GWW (mmHg%) | 62 (37-175) | 94 (62-131) | <0.001 | 91 (70-191) | 74 (50-111) | <0.001 |
| GWE (mmHg%) | 96 (90-98) | 95 (94-97) | NS | 95 (91-96) | 96 (94-97) | NS |
BSA: body surface area; DBP: diastolic blood pressure; GCW: global constructive work; GWE: global work efficiency; GWI: global work index; GWW: global wasted work; LAVi: left atrial volume index; rACo: repaired aortic coarctation; SBP: systolic blood pressure.
In our group of patients, SBP and LV GLS were the only independent predictors of GCW, as well as GWI, even after adjustment for age and renin angiotensin aldosterone system blockers use (Table 4). The only independent predictor of both GWW and GWE was LV GLS. Neither age nor gender had any significant influence on any of the MW parameters in our sample of patients.
Correlations in multivariate analysis of myocardial work indices and main variables.
| Variables | Univariate β-coefficient | p-value | Multivariate β-coefficient | p-value |
|---|---|---|---|---|
| GWI | ||||
| Age | 0.306 | 0.049 | 0.091 | 0.289 |
| Male gender | -0.130 | 0.413 | - | - |
| BSA | -0.081 | 0.612 | - | - |
| SBP | 0.460 | 0.002 | 0.432 | <0.001 |
| RAAS blocker | 0.359 | 0.020 | -0.036 | 0.687 |
| Betablocker | 0.003 | 0.985 | - | - |
| CCB | 0.122 | 0.411 | - | - |
| LVEDD/BSA | -0.013 | 0.933 | - | - |
| E wave | 0.238 | 0.128 | - | - |
| E/e’ | 0.180 | 0.255 | - | - |
| TAPSE | 0.007 | 0.964 | - | - |
| Tricuspid s’ | 0.020 | 0.908 | - | - |
| Aortic gradient | -0.074 | 0.642 | - | - |
| Bicuspid valve | -0.052 | 0.744 | - | - |
| LV GLS | -0.767 | <0.001 | -0.765 | <0.001 |
| GCW | ||||
| Age | 0.280 | 0.072 | 0.050 | 0.495 |
| Male gender | -0.248 | 0.113 | - | - |
| BSA | -0.082 | 0.605 | - | - |
| SBP | 0.547 | <0.001 | 0.534 | <0.001 |
| RAAS blocker | 0.367 | 0.017 | -0.033 | 0.665 |
| Betablocker | 0.103 | 0.515 | - | - |
| CCB | 0.094 | 0.554 | - | - |
| LVEDD/BSA | -0.029 | 0.858 | - | - |
| E wave | 0.291 | 0.061 | 0.121 | 0.077 |
| E/e’ | 0.231 | 0.141 | - | - |
| TAPSE | -0.124 | 0.432 | - | - |
| Tricuspid s’ | -0.107 | 0.540 | - | - |
| Aortic gradient | 0.089 | 0.574 | - | - |
| Bicuspid valve | -0.106 | 0.506 | - | - |
| LV GLS | -0.746 | <0.001 | -0.716 | <0.001 |
| GWW | ||||
| Age | 0.149 | 0.346 | - | - |
| Male gender | -0.029 | 0.853 | - | - |
| BSA | -0.080 | 0.614 | - | - |
| SBP | 0.121 | 0.443 | - | - |
| RAAS blocker | 0.017 | 0.917 | - | - |
| Betablocker | 0.073 | 0.648 | - | - |
| CCB | 0.177 | 0.263 | - | - |
| LVEDD/BSA | 0.160 | 0.311 | - | - |
| E wave | -0.089 | 0.574 | - | - |
| E/e’ | 0.238 | 0.128 | - | - |
| TAPSE | -0.173 | 0.275 | - | - |
| Tricuspid s’ | -0.017 | 0.921 | - | - |
| Aortic gradient | 0.096 | 0.546 | - | - |
| Bicuspid valve | 0.203 | 0.197 | - | - |
| LV GLS | 0.594 | <0.001 | 0.594 | <0.001 |
| GWE | ||||
| Age | -0.030 | 0.852 | - | - |
| Male gender | -0.029 | 0.857 | - | - |
| BSA | 0.017 | 0.913 | - | - |
| SBP | -0.064 | 0.689 | - | - |
| RAAS blocker | 0.066 | 0.677 | - | - |
| Betablocker | 0.026 | 0.869 | - | - |
| CCB | -0.054 | 0.736 | - | - |
| LVEDD/BSA | -0.081 | 0.611 | - | - |
| E wave | 0.220 | 0.162 | - | - |
| E/e’ | -0.173 | 0.273 | - | - |
| TAPSE | 0.077 | 0.629 | - | - |
| Tricuspid s’ | -0.126 | 0.472 | - | - |
| Aortic gradient | -0.071 | 0.655 | - | - |
| Bicuspid valve | -0.207 | 0.189 | - | - |
| LV GLS | -0.675 | <0.001 | -0.675 | <0.001 |
BSA: body surface area; CCB: calcium channel blocker; DBP: diastolic blood pressure; GCW: global constructive work; GLS: global longitudinal strain; GWE: global work efficiency. GWI: global work index; GWW: global wasted work; LVEDD: left ventricular end-diastolic diameter; RAAS: renin angiotensin aldosterone system; SBP: systolic blood pressure; TAPSE: Tricuspid Annular Plane Systolic Excursion.
Myocardial deformation assessment with strain using 2D speckle tracking echocardiography has brought about major advancs in LV quantification beyond the traditional ejection fraction. However, strain imaging is relatively load dependent, with an inverse relationship between strain and afterload, and it can affect diagnostic accuracy in myocardial function evaluation.1–6 After several years of research, Russell et al. developed a non-invasive tool to estimate LV pressure during a cardiac cycle and used LV pressure-strain loops to assess MW, showing a strong correlation with invasive measurements.5 Since then, MW has been associated with improvements in the identification of cardiac resynchronization therapy responders7,8 and coronary occlusion in patients with acute coronary syndrome.2 Myocardial work considers both load and deformation and it can offer incremental value in myocardial functional assessment, particularly in the presence of changes in afterload that could lead to misleading results by strain analysis. Increases in afterload can negatively impact on myocardial strain.2 Previous papers showed good repeatability and reproducibility of myocardial work indices obtained by echocardiography.5,6,15,16,19
Aortic coarctation is a condition characterized by chronic increased afterload. Even after repair, some patients have some residual gradient in the descending thoracic aorta, remaining hypertensive and for that reason LV changes can occur. Our patients had been previously exposed to chronic increased afterload, some of them for a long time due to correction at a mean age of 12 years, and some are still on chronic overload despite repair and this might cause some chronic damage in the LV. In fact, 52% were hypertensive patients (on medication), and in general, blood pressure control was adequate in most of the patients at the time of examination, albeit higher compared to the reference population, particularly SBP. However, despite a normal mean SBP, it ranged from 97 to 152 mmHg, and there was also a mild increase in the descending aortic peak gradient, ranging from 3 to 43 mmHg. For that reason, some patients still have a significant and persistent increase in afterload.
With high blood pressure and afterload, there is a reduction in stroke volume, compensated by a shift in the LV pump function to work at a higher energy level, allowing for GLS and ejection fraction to be preserved, and this can be reflected by higher GWI.20,21 However, chronically increased afterload eventually leads to increased LV stiffness and concentric remodeling and eventually LV failure.20,21 In previous studies conducted in hypertensive patients, grade 1 hypertension is associated with an increase in both constructive and wasted work, with preserved MW efficiency and increase in GWI.6 In grade 2-3 hypertension, the increase in constructive and wasted work is more significant, in a proportional way, enabling preservation of GWE and a further increase in GWI.6 Wasted MW increase can be related to the increase myocardium wall stress against high afterload.6 In fact, myocardial hypertrophy caused by chronic increased afterload is a compensation mechanism for increased wall stress and increases significantly GWI.6 When dysfunction appears, with LV dilation and elevation of end-systolic wall stress, wasted work is further increased, now with a reduction in constructive work, leading to a reduction in both GWE and GWI.6
Based on previous observations, we would expect our group of patients to show the same pattern of increased GCW, GWW and GWI with preserved GWE as in hypertensive patients. However, we found lower GCW and GWI, without the expected and proportional increase in GWW but still with preserved efficiency. Global work index and GCW are being recognized as indices of myocardial performance, as an expression of positive LV work, hence contractility. Based on this assumption, the sample studied, despite normal LV systolic function (as assessed by ejection fraction and GLS), already had changes compatible with impaired myocardial performance, but mechanical efficiency remained preserved, as assessed by GWE. Our sample also had an increased LV mass and E/e’ ratio suggesting compensating changes due to this chronically increased afterload. Our findings are consistent with a possible cardiomyopathic process, not reproducing what could have been expected from a chronic afterload increase model without overt dysfunction by classic evaluation. Previous studies have reported that structurally normal hearts, even in the presence of cardiovascular risk factors, retain their mechanical efficiency, better inferred by preserved GWE, as we found in our work.22 However, in our study, despite GWE preservation, GWI and GCW were abnormally low, and this can be an indicator of a transitional stage to overt systolic dysfunction.
Previously published papers on reference values for MW indices showed some divergent data regarding gender comparisons.15,19 Galli obtained significantly lower GWI and GCW in men, with similar GWW and GWE.19 Those results were explained by the authors by the fact that both GLS and E wave velocity, that were correlated with GWI and GCW, were significantly lower in men than in women. However, Manganaro obtained higher GWW, similar GCW, lower GWE and a trend to lower GWI in men.15 These GWW higher values were thought to be related to the effect of blood pressure, which was higher in male, but multivariate analysis did not confirm the effect of blood pressure on GWW. In fact, multivariable analysis has consistently shown in all studies, including ours, an absence of effect based on age or gender in MW parameters and a strong correlation of GWI and GCW with SBP and correlation of LV GLS with all MW parameters. But despite the absence of correlation between blood pressure and GWW, Chan showed that in hypertensive patients, there is an expected increase in GWW and for that reason, we would assume some possible influence of blood pressure.6 To further increase the discrepancy in results from different studies, in our sample we found that GWW was higher in females and the other MW parameters were identical. The main differences between genders were lower LV mass index, higher E wave velocity and a trend to higher E/E’ ratio in females. But these differences were also observed in Galli and Manganaro studies. Also, GLS (the only independent predictor of GWW) was identical between genders. However, if we compare mean SBP between genders in our sample and in the reference group, we found that the group with the highest SBP is the female group with rACo, suggesting again a possible relationship between blood pressure and this increase in GWW. This question remains unanswered and additional studies with larger samples are needed.
LimitationsOur sample of patients with rACo is relatively small, but many patients had to be excluded due to concomitant bicuspid aortic valve disease with significant aortic stenosis. In fact, we only included patients with bicuspid aortic valve disease if they did not have significant disease (stenosis or regurgitation). Patients with significant aortic stenosis were excluded, as their LV pressure will not be an accurate reflection of peripheral blood pressure.
In the non-invasive MW technique, the use of arterial systolic pressure measured with a cuff and sphygmomanometer in the brachial artery can be imprecise, because systolic pressure varies throughout the arterial tree. However, Russel demonstrated that this technique is sufficiently reliable to be used in clinical practice.5 Blood pressure was measured in the right and left arm to check for differences, as it is usually the practice in these patients, but only blood pressure from the right arm was considered for the present study because it is the closest to the heart. Moreover, blood pressure measurements were taken simultaneously with the echocardiographic acquisition, according to the standard technique in use.5,15,19 However, we do not have information regarding ambulatory blood pressure measurements and control in the studied population.
Heart rate may have a potential impact in MW, but this was not assessed in our study.23 However, our patients had a relatively homogeneous heart rate between 60-80 bpm, and for that reason, we do not expect a significant influence from heart rate in our results.
We used reference values from a previous study as a comparator. These results were obtained from a large sample, allowing specific subgroup analysis according to gender and age, that was not possible in our sample because it was much smaller and sub-group analysis in our sample would have lacked statistical power.
Myocardial work analysis is not available in all echocardiographic equipment and for that reason, it cannot be applied at all centers. It is expected that other vendors will have this technology available in a near future. However, some reproducibility problems between vendors may be described, as is the case for strain analysis.
ConclusionsThe introduction of non-invasive MW estimation by speckle tracking echocardiography, a method validated against invasive measurements, has brought a new promise in the clinical evaluation of myocardial performance in previous studies, particularly because it can unmask myocardial at risk of future failure in face of normal deformation indices and impaired MW parameters.
In patients with rACo, we found a lower GCW and GWI, suggesting some degree of LV dysfunction, despite normal ejection fraction and GLS, confirming the usefulness of myocardial work compared with standard techniques. Systolic blood pressure is an independent predictor of GWI and GCW and GLS the other independent predictor of all MW parameters. For that reason, strict control of blood pressure is essential in these patients.
We can postulate that MW analysis may offer additional information about cardiac performance at a very early stage of the disease. However, the prognostic role of this promising tool requires additional longitudinal research. MW impairment can forecast or anticipate overt dysfunction, particularly in the context of increased afterload, and research with serial assessments of patients at risk of developing systolic dysfunction is warranted.
Author's contributionAna Teresa Timoteo - concept and design, data collection, data interpretation, statistical analysis, drafting of the manuscript, critical revision, and approval of the article.
Luisa Moura Branco - data collection, critical revision, and approval of the article.
Ana Galrinho - data collection, critical revision, and approval of the article.
Pedro Rio - data collection, critical revision, and approval of the article.
Lidia Sousa - data interpretation, critical revision, and approval of the article.
Rui Cruz Ferreira - data interpretation, critical revision, and approval of the article.
Conflicts of interestThe authors have no conflicts of interest to declare.