The effectiveness of cardiac rehabilitation (CR) in improving exercise capacity and quality of life (QoL) in heart failure (HF) is well established. However, it remains underutilized in women. We aimed to compare the adherence and effectiveness of a CR program in women and men with HF.
MethodsThis was a prospective single-center study of consecutive 93 HF patients referred to a CR program between September 2019 and July 2021. We defined adherence as the percentage of sessions patients attended. Effectiveness outcomes were changes in peak oxygen uptake (VO2 peak) and QoL measurements before (baseline) and after the CR program (12wk). VO2 peak was assessed by a maximal effort cardiopulmonary exercise testing on a treadmill. QoL was assessed using the Minnesota Living with Heart Failure Questionnaire (MLHFQ).
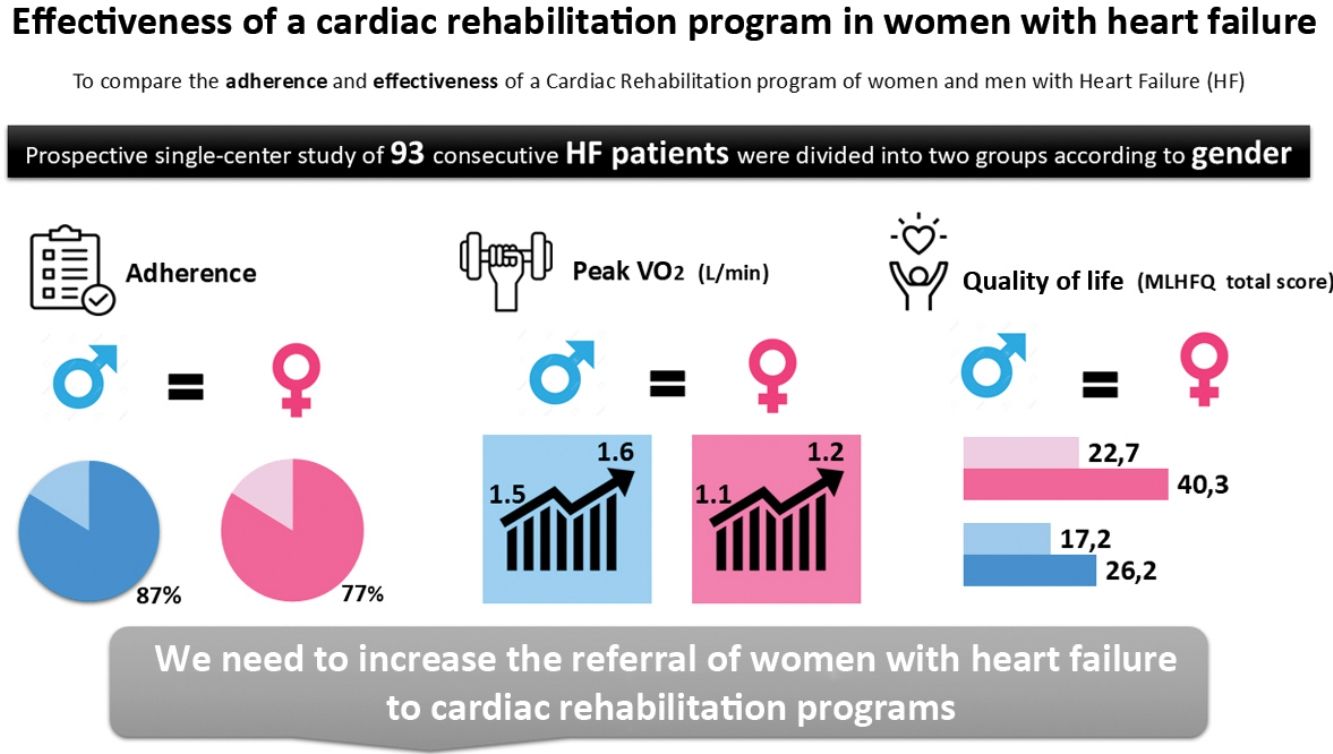
ResultsAmong 93 patients, 32.3% were female. Regarding adherence, 84% of patients completed the CR program, and no significant differences were found between groups (p=0.232). The increase in VO2 peak did not differ between genders (p=0.938). A significant reduction in the total, physical and emotional MLHFQ scores in both genders was observed (all p<0.05). There were no significant differences in QoL effectiveness analysis between the groups (all p=NS).
ConclusionWomen with HF adhered to the CR program similarly to men and had a similar increase in VO2 peak, a robust and validated prognostic marker for HF in this setting. Women benefited as much as men in all dimensions of QoL. Together, these data emphasize the need to increase the referral of women with HF to CR programs.
A eficácia da reabilitação cardíaca (RC) na melhoria da capacidade de exercício e qualidade de vida (QoL) na insuficiência cardíaca (IC) está bem estabelecida. No entanto, continua subutilizada em mulheres. Foi o nosso objetivo comparar a adesão e a eficácia de um programa de RC entre mulheres e homens com IC.
MétodosRealizámos um estudo unicêntrico prospetivo com 93 doentes consecutivos com IC referenciados ao programa de RC no nosso hospital entre setembro de 2019 e julho de 2021. Definimos a adesão pela percentagem de sessões que os doentes frequentaram. A eficácia foi avaliada pelas diferenças no pico de consumo de oxigénio (VO2pico) e na pontuação da QoL antes e após o programa de RC. O VO2pico foi estimado durante uma prova cardiorrespiratória máxima. A QoL foi avaliada utilizando o Minnesota Living with Heart Failure Questionnaire® (MLHFQ).
ResultadosDos 93 doentes, 32,3% eram mulheres. Em relação à adesão, 84% dos doentes completaram o programa de RC e não foram encontradas diferenças significativas entre os grupos (p=0,232). O aumento no VO2pico não diferiu entre os sexos (p=0,938). Foi observada uma redução significativa na pontuação total, física e emocional do MLHFQ em ambos os sexos (todos p<0,05). Não foram encontradas diferenças significativas na análise de eficácia da QoL entre os grupos (todos p=NS).
ConclusãoAs mulheres com IC apresentaram uma adesão semelhante ao programa de RC e o mesmo aumento no VO2pico, um marcador prognóstico robusto e validado na IC. As mulheres beneficiaram tanto quanto os homens em todas as dimensões da QoL. Estes dados reforçam a necessidade de aumentar a referenciação das mulheres com IC para programas de RC.
Heart failure (HF) continues to be a significant global health concern associated with reduced survival; it is one of the leading causes of morbidity and mortality in both genders.1 It affects millions of people worldwide and prevalence is rising due to aging populations and improvements in survival rates for other cardiac conditions.2 Despite evidence from randomized clinical trials demonstrating the equal efficacy of pharmacological therapy in both men and women, a concerning issue of undertreatment among women persists.3
Cardiac rehabilitation (CR) is strongly recommended as a Class I Level A intervention for managing HF, as it has been shown to improve functional capacity and quality of life (QoL), as well as to reduce the risk of hospitalization and mortality.4–6 CR programs offer a multidisciplinary approach to secondary prevention, which includes patient assessment, cardiovascular risk management, exercise training, dietary advice, physical activity counseling, psychosocial support and vocational assistance.7,8 Despite its benefits, CR remains widely underused,9 especially among women.6,10 Several studies have shown that women are referred less frequently to CR programs, partially due to a misperception of its reduced effectiveness by healthcare professionals compared to men.6 In addition, it has been reported that females are less likely than males to attend CR sessions and complete the CR program.6,11,12 It is important to note that despite the low participation rates of females in CR, research has demonstrated that CR can lead to similar or even greater mortality benefits in females when compared with males in post-acute myocardial infarction patients.13–15 However, studies comparing the impact of CR between men and women with HF patients are lacking. These studies could provide valuable insights into potential differences in treatment responses, further emphasizing the need for gender-specific strategies in CR.
ObjectivesThe aim of our study was, therefore, to compare the impact of a CR program on functional capacity, exercise session adherence, and QoL in men and women with HF.
MethodsStudy design and study populationWe conducted a prospective single-center study of 93 consecutive patients with HF referred to a CR program from September 2019 to July 2021. Our study population comprised patients diagnosed with HF based on the diagnostic criteria outlined by the European guidelines4 and who were eligible to participate in the CR program based on CR recommendations.4,5,8,16 The patients included in our study were divided into two groups according to gender. The study was conducted at a tertiary university public hospital. The study was approved by the ethics committee and was conducted in accordance with the Declaration of Helsinki.
Intervention: Cardiac rehabilitation programThe CR program included a total of 24 exercise training sessions over 12-week (two sessions per wk). Each session comprised 5–10 minutes of warm-up with calisthenics and stretching exercises, followed by 25 minutes of resistance exercises using elastic bands (two sets of 12–15 repetitions for each exercise), followed by 30 minutes of moderate to vigorous aerobic training at 60%–80% of peak oxygen uptake (VO2 peak) or guided by Borg's scale (11–14). Finally, a 5-minute cool-down period with stretching exercises was conducted. In addition to the supervised sessions, patients were encouraged to boost their daily physical activity levels on the other days. Throughout the supervised exercise sessions, the patient's heart rate and electrocardiogram were monitored using a real-time heart rate monitor (Polar M200 model; Polar Electro Ltd). The intensity of the resistance training was progressively increased based on the patient's perceived exertion, as measured using the Borg scale.12 Additionally, the CR program included weekly group sessions, scheduled on the same days as the exercise sessions, to address dietary goals for improving modifiable cardiovascular risk factor control, encourage lifestyle behavior changes, and offer psychological and/or psychiatric consultations as clinically necessary.
AssessmentsDemographics and clinical dataDemographic data (age), anthropometric (body mass index), comorbidities, HF-related characteristics (HF phenotype, etiology, New York Heart Association (NYHA) functional class, left ventricular ejection fraction (LVEF), B-type natriuretic peptide (BNP) plasma levels], pharmacological and non-pharmacological treatments were captured from patients’ files and/or during the CR consult.
The analysis of the effectiveness of the outcomes of interest was conducted by comparing the baseline values (measured before the CR program) with the final values (measured after completing the 12-week CR program).
Functional capacityFunctional capacity was evaluated using VO2 peak (ml/min/kg) and the ventilatory efficiency [minute ventilation to carbon dioxide production (VE/VCO2) slope] assessed during the cardiopulmonary exercise test (CPX). All patients underwent a CPX on a treadmill (Medisoft, Model 870C) with continuous electrocardiographic monitoring throughout the entire protocol. Exercise testing protocol, the modified Naughton or Bruce, was chosen according to the patient's physical activity level and orthopedic/musculoskeletal condition. VO2 peak is currently recognized as the gold standard for objectively evaluating the functional capacity of HF patients.17 However, since the VE/VCO2 slope has prognostic value for submaximal exercise levels and several studies have recently demonstrated that it appears the most powerful predictor of prognosis in HF patients, this parameter was also used to estimate the impact and effectiveness of the CR program.17 Respiratory gas exchange measurements were obtained at each breath cycle and recorded every 30 seconds using the stationary metabolic cart system (Geratherm® Respiratory Ergostik, BLUE CHERRY®). Heart rate and blood pressure were regularly recorded throughout the test. VO2 peak was determined as the highest achieved VO2 during exercise. Patients were strongly encouraged to achieve a respiratory exchange ratio (RER) above 1.0518,19 and a Borg rating of perceived exertion score >17 on the 6–20 scale.20
Exercise sessions adherenceAdherence to the exercise sessions was assessed as the total percentage of exercise sessions attended by participants. Adherence to the CR program was defined as completing at least 80% of the prescribed exercise sessions, as described in the literature.21,22
Quality of lifeQuality of life was assessed using the Minnesota Living with Heart Failure Questionnaire® (MLHFQ). The MLHFQ was specifically developed and validated to evaluate the impact of HF systematically and comprehensively on patient's QoL.23,24 This questionnaire consists of 21 questions that cover the physical dimension (eight questions, scored from 0 to 40), emotional dimension (five questions, scored from 0 to 25), and socioeconomic factors that can potentially negatively affect the QoL of HF patients. The total MLHFQ score ranges from 0 to 105, with higher scores indicating a poorer QoL. Therefore, the total score as well as the scores for the physical and emotional dimensions were evaluated for each group.
Statistical analysisStatistical analysis was performed using IBM Statistical Package for the Social Sciences (SPSS) software, version 26.0. Continuous variables with a normal distribution were reported as means and standard deviations (SD), while continuous variables without a normal distribution were reported as medians and interquartile ranges (IQR). Categorical variables were presented as absolute numbers and percentages (%). The male and female genders were compared for each variable using the Student's t-test or Wilcoxon rank-sum test for continuous variables. The chi-square test or Fisher's exact tests were used for categorical variables to evaluate any differences between the two genders. Paired t-tests were employed to compare the mean values between baseline and final for each variable. Analysis of covariance was also employed to adjust for baseline CPX and MLHFQ measurements. p<0.05 was considered statistically significant.
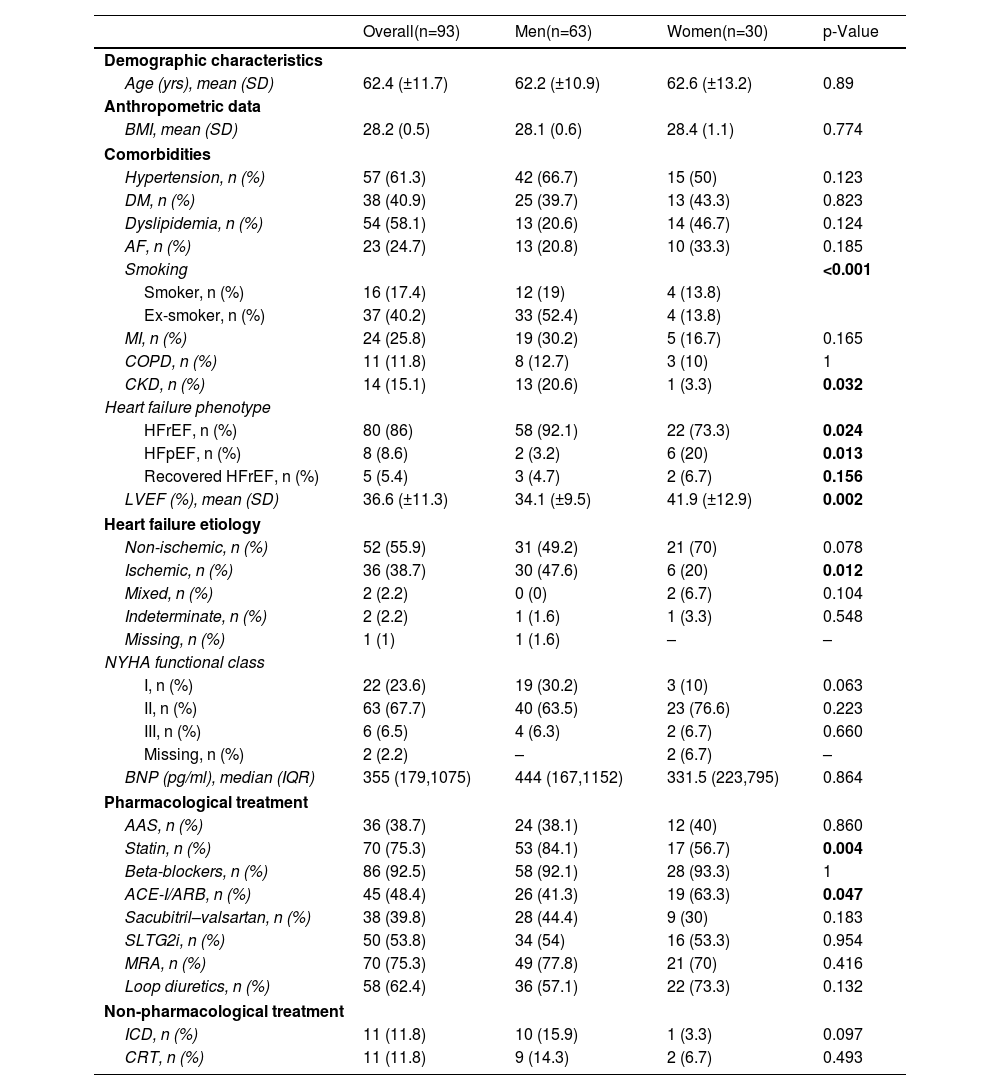
ResultsStudy populationAmong a total of 93 patients with HF referred to the CR program, the mean age was 62±12 years. Baseline demographic and clinical characteristics of the study population by gender are shown in Table 1. In general, men and women showed similar characteristics, including age, body mass index, comorbidities and treatment. Hypertension was the most frequent (61.3%) in the total sample, as well as both genders, while chronic kidney disease (CKD) was more prevalent in men (20.6% vs. 3.3%, p=0.032). Most patients were in NYHA functional class II (69.2%) and the average of LVEF in men was lower compared with women (34% vs. 42%, p=0.002). HF with reduced ejection fraction (HFrEF) was the most prevalent phenotype in men (92.1% vs. 73.3%, p=0.024), whereas HF with preserved ejection fraction (HFpEF) was the most observed in women (20% vs. 3.2%, p=0.013). In the male group, ischemic etiology was statistically more prevalent (48.4% vs. 20%, p=0.012).
Characterization of overall study population and by gender.
| Overall(n=93) | Men(n=63) | Women(n=30) | p-Value | |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age (yrs), mean (SD) | 62.4 (±11.7) | 62.2 (±10.9) | 62.6 (±13.2) | 0.89 |
| Anthropometric data | ||||
| BMI, mean (SD) | 28.2 (0.5) | 28.1 (0.6) | 28.4 (1.1) | 0.774 |
| Comorbidities | ||||
| Hypertension, n (%) | 57 (61.3) | 42 (66.7) | 15 (50) | 0.123 |
| DM, n (%) | 38 (40.9) | 25 (39.7) | 13 (43.3) | 0.823 |
| Dyslipidemia, n (%) | 54 (58.1) | 13 (20.6) | 14 (46.7) | 0.124 |
| AF, n (%) | 23 (24.7) | 13 (20.8) | 10 (33.3) | 0.185 |
| Smoking | <0.001 | |||
| Smoker, n (%) | 16 (17.4) | 12 (19) | 4 (13.8) | |
| Ex-smoker, n (%) | 37 (40.2) | 33 (52.4) | 4 (13.8) | |
| MI, n (%) | 24 (25.8) | 19 (30.2) | 5 (16.7) | 0.165 |
| COPD, n (%) | 11 (11.8) | 8 (12.7) | 3 (10) | 1 |
| CKD, n (%) | 14 (15.1) | 13 (20.6) | 1 (3.3) | 0.032 |
| Heart failure phenotype | ||||
| HFrEF, n (%) | 80 (86) | 58 (92.1) | 22 (73.3) | 0.024 |
| HFpEF, n (%) | 8 (8.6) | 2 (3.2) | 6 (20) | 0.013 |
| Recovered HFrEF, n (%) | 5 (5.4) | 3 (4.7) | 2 (6.7) | 0.156 |
| LVEF (%), mean (SD) | 36.6 (±11.3) | 34.1 (±9.5) | 41.9 (±12.9) | 0.002 |
| Heart failure etiology | ||||
| Non-ischemic, n (%) | 52 (55.9) | 31 (49.2) | 21 (70) | 0.078 |
| Ischemic, n (%) | 36 (38.7) | 30 (47.6) | 6 (20) | 0.012 |
| Mixed, n (%) | 2 (2.2) | 0 (0) | 2 (6.7) | 0.104 |
| Indeterminate, n (%) | 2 (2.2) | 1 (1.6) | 1 (3.3) | 0.548 |
| Missing, n (%) | 1 (1) | 1 (1.6) | – | – |
| NYHA functional class | ||||
| I, n (%) | 22 (23.6) | 19 (30.2) | 3 (10) | 0.063 |
| II, n (%) | 63 (67.7) | 40 (63.5) | 23 (76.6) | 0.223 |
| III, n (%) | 6 (6.5) | 4 (6.3) | 2 (6.7) | 0.660 |
| Missing, n (%) | 2 (2.2) | – | 2 (6.7) | – |
| BNP (pg/ml), median (IQR) | 355 (179,1075) | 444 (167,1152) | 331.5 (223,795) | 0.864 |
| Pharmacological treatment | ||||
| AAS, n (%) | 36 (38.7) | 24 (38.1) | 12 (40) | 0.860 |
| Statin, n (%) | 70 (75.3) | 53 (84.1) | 17 (56.7) | 0.004 |
| Beta-blockers, n (%) | 86 (92.5) | 58 (92.1) | 28 (93.3) | 1 |
| ACE-I/ARB, n (%) | 45 (48.4) | 26 (41.3) | 19 (63.3) | 0.047 |
| Sacubitril–valsartan, n (%) | 38 (39.8) | 28 (44.4) | 9 (30) | 0.183 |
| SLTG2i, n (%) | 50 (53.8) | 34 (54) | 16 (53.3) | 0.954 |
| MRA, n (%) | 70 (75.3) | 49 (77.8) | 21 (70) | 0.416 |
| Loop diuretics, n (%) | 58 (62.4) | 36 (57.1) | 22 (73.3) | 0.132 |
| Non-pharmacological treatment | ||||
| ICD, n (%) | 11 (11.8) | 10 (15.9) | 1 (3.3) | 0.097 |
| CRT, n (%) | 11 (11.8) | 9 (14.3) | 2 (6.7) | 0.493 |
Abbreviations: AAS: acetylsalicylic acid; ACE-I: angiotensin-converting enzyme inhibitor; AF: atrial fibrillation; ARB: angiotensin receptor blockers; BMI: body mass index; BNP: B-type natriuretic peptide; CKD: chronic kidney disease; COPD: chronic obstructive pulmonary disease; CR: cardiac rehabilitation; CRT: cardiac resynchronization therapy; DM: diabetes mellitus; HFpEF: heart failure with preserved ejection fraction; HFrEF: heart failure with reduced ejection fraction; ICD: implantable cardioverter-defibrillator; IQR: interquartile range; LVEF: left ventricular ejection fraction; MI: myocardial infarction; MRA: mineralocorticoid receptor antagonist; NYHA: New York Heart Association; SD: standard deviation; SLTG2: sodium-glucose co-transporter 2.
In our study, the overall adherence to the CR program was 84%, with adherence rates of 87% in men and 77% in women. No statistically significant differences were observed between genders regarding adherence to the CR program (p=0.232). Of the 15 patients who did not adhere to the CR program, the majority were male (8, 53.3%) with a non-ischemic etiology (9, 60%).
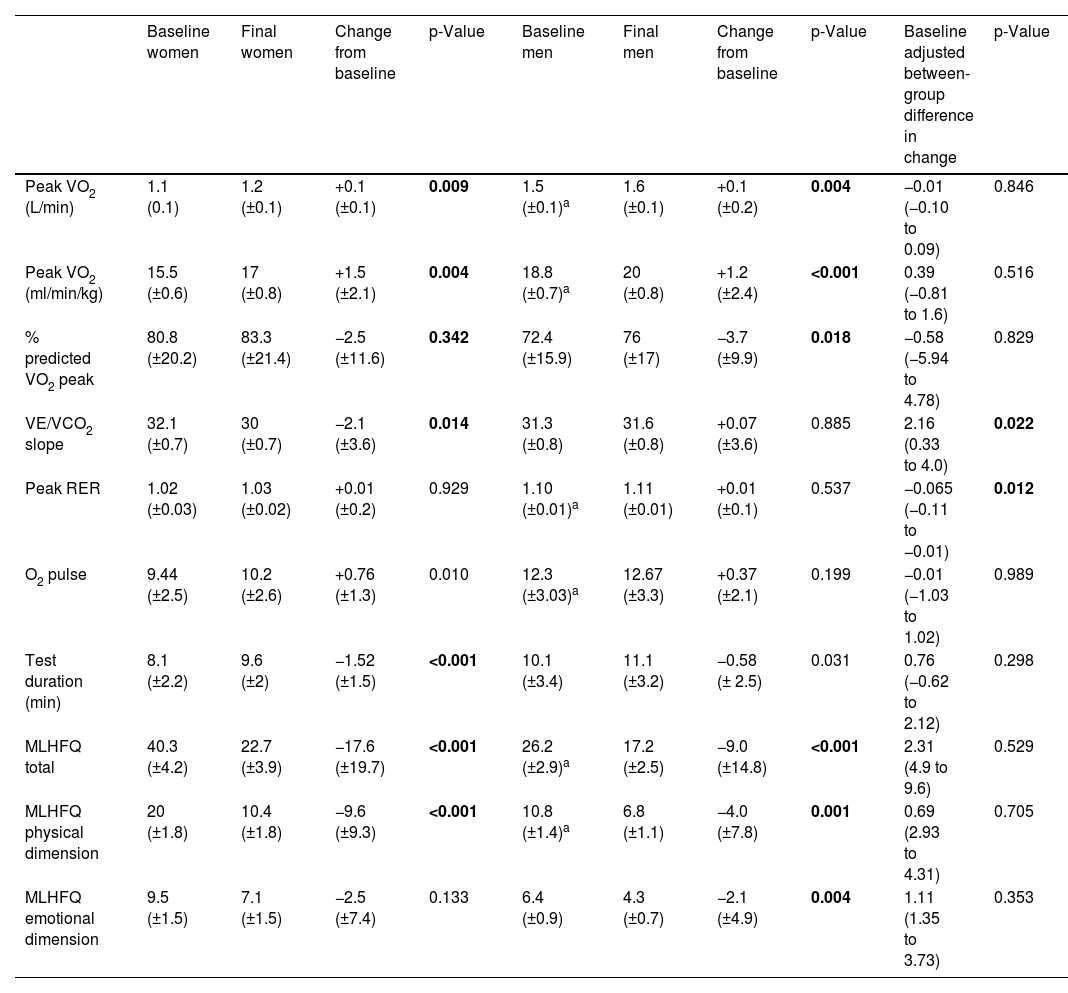
Functional capacityTable 2 presents the baseline and final functional capacity evaluations in the study population by gender. A significant increase in VO2 peak was observed in both genders after the CR program compared to baseline (men: +1.2±2.4 ml/min/kg; women: +1.5±2.1 ml/min/kg), with no between-group difference (0.39 ml/min/kg, 95% CI: −0.81 to 0.81, p=0.516). Furthermore, no significant difference was observed between men and women in the O2 pulse after adjusting for baseline values (p=0.989). Regarding ventilatory efficiency (VE/VCO2 slope), only women experienced significant improvements (−2.1±3.6, p=0.014), with a significant between-group difference (2.16, 95% CI: 0.33–4.00, p=0.022). Both genders saw a small increase in RER peak after CR program; however, there were no significant difference within each group (p=NS). There was a significant difference between-group (−0.065, 95% CI: −0.11 to 0.01, p=0.012) when adjusted to baseline values, with men showing a slightly greater increase in RER peak compared to women.
Baseline and final functional capacity and quality of life in the study population by gender.
| Baseline women | Final women | Change from baseline | p-Value | Baseline men | Final men | Change from baseline | p-Value | Baseline adjusted between-group difference in change | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Peak VO2 (L/min) | 1.1 (0.1) | 1.2 (±0.1) | +0.1 (±0.1) | 0.009 | 1.5 (±0.1)a | 1.6 (±0.1) | +0.1 (±0.2) | 0.004 | −0.01 (−0.10 to 0.09) | 0.846 |
| Peak VO2 (ml/min/kg) | 15.5 (±0.6) | 17 (±0.8) | +1.5 (±2.1) | 0.004 | 18.8 (±0.7)a | 20 (±0.8) | +1.2 (±2.4) | <0.001 | 0.39 (−0.81 to 1.6) | 0.516 |
| % predicted VO2 peak | 80.8 (±20.2) | 83.3 (±21.4) | −2.5 (±11.6) | 0.342 | 72.4 (±15.9) | 76 (±17) | −3.7 (±9.9) | 0.018 | −0.58 (−5.94 to 4.78) | 0.829 |
| VE/VCO2 slope | 32.1 (±0.7) | 30 (±0.7) | −2.1 (±3.6) | 0.014 | 31.3 (±0.8) | 31.6 (±0.8) | +0.07 (±3.6) | 0.885 | 2.16 (0.33 to 4.0) | 0.022 |
| Peak RER | 1.02 (±0.03) | 1.03 (±0.02) | +0.01 (±0.2) | 0.929 | 1.10 (±0.01)a | 1.11 (±0.01) | +0.01 (±0.1) | 0.537 | −0.065 (−0.11 to −0.01) | 0.012 |
| O2 pulse | 9.44 (±2.5) | 10.2 (±2.6) | +0.76 (±1.3) | 0.010 | 12.3 (±3.03)a | 12.67 (±3.3) | +0.37 (±2.1) | 0.199 | −0.01 (−1.03 to 1.02) | 0.989 |
| Test duration (min) | 8.1 (±2.2) | 9.6 (±2) | −1.52 (±1.5) | <0.001 | 10.1 (±3.4) | 11.1 (±3.2) | −0.58 (± 2.5) | 0.031 | 0.76 (−0.62 to 2.12) | 0.298 |
| MLHFQ total | 40.3 (±4.2) | 22.7 (±3.9) | −17.6 (±19.7) | <0.001 | 26.2 (±2.9)a | 17.2 (±2.5) | −9.0 (±14.8) | <0.001 | 2.31 (4.9 to 9.6) | 0.529 |
| MLHFQ physical dimension | 20 (±1.8) | 10.4 (±1.8) | −9.6 (±9.3) | <0.001 | 10.8 (±1.4)a | 6.8 (±1.1) | −4.0 (±7.8) | 0.001 | 0.69 (2.93 to 4.31) | 0.705 |
| MLHFQ emotional dimension | 9.5 (±1.5) | 7.1 (±1.5) | −2.5 (±7.4) | 0.133 | 6.4 (±0.9) | 4.3 (±0.7) | −2.1 (±4.9) | 0.004 | 1.11 (1.35 to 3.73) | 0.353 |
Data are presented as mean±SD. Abbreviations: MLHFQ: Minnesota Living with Heart Failure Questionnaire; RER: respiratory exchange ratio; SD: standard deviation; VE/VCO2: minute ventilation/carbon dioxide output ratio; VO2: oxygen consumption.
A significant decrease was observed in both groups after the CR program in the total score of MLHFQ (−9±14.8, p<0.001 in males and −17.6±19.7, p<0.001 in females). The physical dimension score significantly improved in both groups (−4±7.8, p=0.001 in males and −9.6±9.3, p<0.001 in females). On the other hand, in the emotional dimension score a significant improvement was observed only in men (−2.1±4.9, p=0.004), but not in women (−2.5±7.4, p=0.133). Regarding the analysis of effectiveness in QoL, no significant differences were observed between genders in the MLHFQ total score (p=0.529), as well as in the scores for the physical dimension (p=705) and the emotional dimension (p=0.353).
DiscussionThe main findings of our study indicate that women with HF adhere to a 12-week CR program similarly to men and have similar improvements in both VO2 peak and QoL.
Peak VO2 is a prognostic factor with significant clinical implications, as it has been associated with a reduced risk of rehospitalization in HF patients.6 In our study, we found no significant gender-based differences in the effectiveness of the CR program regarding functional capacity improvement. Several studies on the effectiveness of CR in ischemic heart disease and HF, particularly in functional capacity improvement assessed by VO2 peak after CR, point to inferior results observed in women.25–28 These findings suggest that women experience a comparatively smaller increase in VO2 peak from each session. It has been hypothesized that women may require a specific CR program with a longer duration.26,29,30 The prescription of more a conservative exercise plans due to older age and the higher burden of comorbidities in women when referred to CR programs has been identified as one of the factors that limit functional capacity and QoL improvement in women.28 In our sample, the groups were relatively homogeneous, regarding age and comorbidities, which may partially explain the results obtained. Furthermore, although the exercise training program was the same for both genders, patients received an individualized exercise intensity prescription. Similarly, a study of patients with cardiovascular disease compared the improvement in VO2 peak between genders after a high-intensity program, with results showing that men and women experienced similar improvements in VO2 peak (8.8% vs 9.0%, p=0.273).31
Additionally, there were significant differences between groups in terms of the RER. Less muscle mass and strength,32 hormonal influences (as estrogen promotes greater fat oxidation over carbohydrate use),33 psychological factors in perceived exertion (women may end exercise testing earlier due to perceived discomfort or exhaustion at lower intensities than men)34 and a lower lactate threshold32 may contribute to lower average RER values in women's CPETs. However, we believe these results should not hinder the interpretation of the present data.
On the other hand, the effectiveness of CR in ventilatory efficiency improvement differed between genders, as only the women's group showed a significant VE/VCO2 slope improvement after CR. This result might be attributed to the small sample size of our study. Further larger studies are warranted to comprehensively elucidate the impact of CR programs on ventilatory efficiency between genders.
Results from a meta-analysis on adherence to CR programs show that the average adherence rate is approximately 66.5±18.2% across studies.35 However, in our study, the overall adherence to the CR program was 84%. Implementing measures described in the literature that have been shown to increase women's adherence to CR, such as self-monitoring of physical activity, planning, and personalized counseling by healthcare professionals,35 may explain the higher adherence observed in our study. Some studies have shown lower adherence to CR in women for several reasons, principally due to family responsibilities, transportation problems and advanced age with more comorbidities.35 Our findings reveal that despite women comprising less than half of the participants enrolled in our CR program (30 women vs. 63 men), no significant differences were observed in adherence between genders. Strategies including automatic referral systems, liaison/nurse-patient contact, and early post-hospital referral are warranted to increase women's referral to CR programs. In addition, since women are more likely than men to perceive exercise as tiring or painful,34 future research should explore exercise prescription strategies that employ alternative approaches. Incorporating specific aerobic training programs, such as dance-based programs, could provide considerable benefits for adherence and cardiovascular outcomes in women.6,36 Dance-based aerobics are often seen as enjoyable, social, and engaging, which can greatly boost motivation and, in turn, enhance adherence to CR programs.6,36 In addition, a meta-analysis showed a significant difference in VO2 peak and QoL in HF patients, demonstrating that dance therapy was as efficient as conventional exercise training in VO2 peak and QoL.36 Thus, randomized studies are needed to evaluate the innovative CR programming strategies for women.
Regarding the impact of our CR program on the QoL, our findings demonstrate a significant increase in QoL improvement, evidenced by a significant reduction in total, physical, and emotional dimension MLHFQ scores in both groups. These results are consistent with findings reported by other authors.37,38
Research indicates that women tend to have a lower QoL than men due to several factors, including a higher number of comorbidities associated with aging, a greater prevalence of psychosocial risk factors (including stress, anxiety, and depression), as well as the need for more frequent and intense exercise sessions to achieve desired outcomes within the program.39 Consistent with the aforementioned, our study revealed that women had lower QoL (higher scores) than men in all dimensions assessed by the MLHFQ prior to the CR program. However, according to our analysis, the effectiveness of the CR program in QoL improvement shows similar results for both genders. Results from a meta-analysis also demonstrated that women achieve similar benefits to men in terms of QoL improvement after CR, namely in the physical dimension.40 These results hold significance, considering the potential vulnerability of women to poorer prognosis due to older age and pre-existing clinical conditions.6,41 Furthermore, some authors have shown that women experienced greater long-term QoL improvement after a CR program that incorporates aerobic and resistance training (as in our CR program) compared to a program consisting of aerobic training alone,42 which might explain our results.
The implementation of a personalized training plan in our CR program, tailored according to the progression of symptoms, addressing specific fears and concerns related to exercise, is widely acknowledged to enhance exercise confidence and self-efficacy. This, in turn, promotes adherence to our CR program and, subsequently, contributes to the improvement in QoL. These strategies emerged as particularly important for women, who often report more negative perceptions toward exercise, higher levels of demotivation,43–45 stress, anxiety, and depression compared to men.38 Likewise, the interaction with other participants, facilitating the sharing of experiences, also promotes specific emotional support, thereby reducing anxiety and apprehension in women.46 This aspect may also contribute to our results. Regarding the emotional domain, although the effectiveness was similar between the groups, some authors argue that when psychosocial components specifically designed for women's needs are added to traditional CR models, women may benefit more than men.40
Our study has some limitations and strengths that deserve to be discussed. It is a prospective study, which was conducted at a single hospital, so the generalization of these results should be viewed with caution. The study included only 93 patients, with a significant imbalance between men (63) and women (30). Therefore, a larger sample, particularly including more women, could yield more robust and representative results. Additionally, this limitation made it impossible to evaluate patients with different heart failure phenotypes (HFrEF and HFpEF), which may influence the response to the program. Finally, as we only included women referred by the attending physician to the CR unit, selection bias cannot be excluded.
ConclusionsIn our study population, women with HF experience3d similar improvements in both VO2 peak and QoL and equal adherence to the CR program compared to men. These findings highlight the importance of improving the referral of women with HF to CR programs.
Conflicts of interestThe authors have no conflicts of interest to declare.