This work explores correlations between genetic polymorphisms in apolipoprotein E (ApoE) and atrial fibrillation (AF). We detected polymorphisms in the APOE gene in 64 patients with AF and 49 non-AF volunteers at the Department of Cardiology of Lianyungang Second People's Hospital between July 2017 and July 2019. We found significant differences in age, body mass index, left atrial diameter, and left ventricular ejection fraction between the two groups. Six APOE genotypes were observed: ɛ2/ɛ2; ɛ2/ɛ3; ɛ2/ɛ4; ɛ3/ɛ3; ɛ3/ɛ4; and ɛ4/ɛ4. The ɛ3/ɛ3 genotype was significantly less frequent in the AF group than in the control group, while the ɛ3/ɛ4 and ɛ4/ɛ4 genotypes were significantly more frequent in the AF group than in the control group (p<0.05). ApoE3 penetrance was significantly lower in the AF group than in the control group (p<0.05), while ApoE4 penetrance was significantly higher in the AF group than in the control group (p<0.05). ApoE3 penetrance was significantly lower in the AF group than in the control group (p<0.05). Binary logistic regression analysis showed that age, body mass index, left atrial diameter, left ventricular ejection fraction, and ApoE4 were risk factors for AF. Finally, we found that ApoE polymorphisms impacted the occurrence of AF and that ApoE4 is an AF-sensitive phenotype.
Este trabalho estudou as correlações entre os polimorfismos genéticos da apolipoproteína E (ApoE) e fibrilhação auricular (FA). Entre julho de 2017 e julho de 2019 detetámos polimorfismos no gene da ApoE em 64 doentes com FA e em 49 voluntários sem FA (Serviço de Cardiologia do Lianyungang Second People's Hospital). Observaram-se diferenças significativas na idade, no índice de massa corporal, no diâmetro auricular esquerdo e na fração de ejeção ventricular esquerda entre os dois grupos. Seis genotipos da ApoE foram observados: ɛ2/ɛ2; ɛ2/ɛ3; ɛ2/ɛ4; ɛ3/ɛ3; ɛ3/ɛ4; e ɛ4/ɛ4. O genotipo ɛ3/ɛ3 foi significativamente menos frequente no grupo da FA do que no grupo controlo, enquanto os genotipos ɛ3/ɛ4 and ɛ4/ɛ4 foram significativamente mais frequentes no grupo da FA em relação ao grupo controlo (p<0,05). A penetração de ApoE3 foi significativamente inferior no grupo FA do que no grupo controlo (p<0,05). A penetração de ApoE4 foi significativamente superior no grupo FA em relação ao grupo controlo (p<0,05). A penetração da ApoE3 foi significativamente menor no grupo FA do que no grupo controlo (p<0,05). A análise da regressão logística binária revelou que a idade, o índice da massa corporal, o diâmetro auricular esquerdo, a fração de ejeção ventricular esquerda e a ApoE4 constituíram fatores de risco para FA. Finalmente, considerámos que os polimorfismos ApoE tiveram impacto na ocorrência da FA e que a ApoE4 é um fenotipo sensível à FA.
Apolipoprotein E (ApoE) is an important apolipoprotein in plasma that plays a key role in regulating lipoprotein metabolism. It is involved in lipid metabolism, oxidative stress, neuroimmune regulation, and inflammatory responses.1,2 There are three alleles of the human APOE gene, which can form six genotypes,3 thus forming a genetic polymorphism. Some of these genotypes may be susceptibility genotypes for hyperlipoproteinemia and arteriosclerosis.4,5 There are three ApoE genotypic categories: protective genotypes (ɛ2/ɛ2 and ɛ2/ɛ3), high-risk genotypes (ɛ3/ɛ4 and ɛ4/ɛ4), and others (ɛ2/ɛ4 and ɛ3/ɛ3).6–8
Atrial fibrillation (AF) is the most common type of arrhythmia. The mechanism of AF is complex, and previous studies have found that AF is closely related to dyslipidemia, excess weight or obesity, diabetes, metabolic syndrome, advanced age, smoking,9,10 hypertension, and various cardiovascular diseases.11 Analysis of a randomized controlled trial performed in the USA revealed that lower levels of low-density lipoprotein (LDL) and total cholesterol were associated with a higher incidence of AF.12 Other studies have shown that ApoE can promote the degradation of chylomicrons, LDL, and very low-density lipoprotein (VLDL) by binding to the low-density lipoprotein receptor (LDLR) and the liver ApoE receptor. We therefore hypothesized that ApoE may increase the risk of AF by degrading LDL.13,14 ApoE is involved in and has significant effects on all aspects of blood lipid metabolism, including the synthesis, secretion, transport, and metabolism of lipoproteins.15 Therefore, there is likely to be a correlation between ApoE and the occurrence of AF.
Additionally, inflammatory mediators, including high-sensitivity C-reactive protein (hs-CRP), interleukin (IL)-6, IL-8, tumor necrosis factor-alpha (TNF-α), and transforming growth factor beta (TGF-β), are closely related to the occurrence and development of all AF types.16–18 Myocardial biopsies in healthy individuals and AF patients have demonstrated that the irreversibility of AF is associated with myocardial remodeling due to persistent inflammatory infiltration in cardiomyocytes.19 While ApoE has anti-inflammatory and antioxidative effects, ApoEɛ4 has a strong proinflammatory effect20 and activates nuclear factor-kappa B (NF-κB), which is involved in atrial remodeling.21
These data support the hypothesis that ApoE is associated with AF. This study was designed to examine the relationship between ApoE genetic polymorphisms and AF and to explore the relationship between ApoE genotype, phenotype, and AF.
MethodsPatient populationThis was a retrospective case-controlled single-center study of subjects who were followed in the Cardiology Department of the Second People's Hospital of Lianyungang City. Between July 2017 and July 2019, 64 inpatients with AF (paroxysmal, persistent, long-term persistent, and permanent) and 49 volunteers without AF (control group) were randomly selected from the hospital's cardiology department. There were 38 male and 26 female patients (mean age 74.38±8.37 years) in the AF group and 29 male and 20 female volunteers (mean age 65.24±12.14 years) in the control group.
The inclusion criteria for the AF group were: AF diagnosed according to definitive electrocardiography (ECG) or Holter ECG monitoring data (absence of sinus P wave, presence of fast and irregular f wave, frequency 350-600 bpm, normal QRS complex shape and duration, and irregular R interval); definite clinical symptoms; and medical history. The inclusion criterion for the control group was non-AF volunteers whose heart rate showed sinus rhythm. Additionally, both groups were required to submit complete medical records and blood samples. The study was approved by the Medical Ethics Committee of the Second People's Hospital of Lianyungang City (grant no. L1618), and all subjects provided written informed consent.
The exclusion criteria were: left ventricular dysfunction; rheumatic heart disease; dilated cardiomyopathy; pulmonary heart disease; hypertrophic cardiomyopathy; viral myocarditis; cardiac surgery; secondary hypertension; hyperthyroidism; electrolyte disorder; malignant tumor; liver and kidney insufficiency; severe infection; tuberculosis; metabolic syndrome; and any of a variety of major diseases that could lead to altered penetrance of inflammatory mediators and/or lipid metabolic disorders.
ApoE polymorphism testPeripheral blood (4 ml) was extracted from fasting patients in the early morning into EDTA anticoagulant tubes and stored in a refrigerator at 4°C. All patient samples were sent to the Unified Nanjing Jinyu Medical Laboratory Center (Nanjing, China) for ApoE gene polymorphism detection. Test results were reported within one week. Three phenotypes and six genotypes of ApoE were detected in this cohort: ApoE2 (ɛ2/ɛ2, ɛ2/ɛ3), ApoE3 (ɛ3/ɛ3) and ApoE4 (ɛ2/ɛ4, ɛ3/ɛ4, ɛ4/ɛ4).
Statistical analysisAll data were analyzed using IBM SPSS v. 21.0 (IBM Corp., Armonk, NY, USA). Measurement data are denoted as mean ± standard deviation, and comparisons were made between two independent samples using an adapted t test. Count data were compared by the chi-square test. Body mass index (BMI) did not conform to a normal distribution, and the comparison method was based on nonparametric tests. Where AF was considered a dependent variable, single factors related to the occurrence of AF were selected by comparisons between the AF and control groups. Covariables were included in binary logistic regression, and then multivariate analysis of AF-related factors was performed.
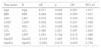
ResultsGeneral comparison between the atrial fibrillation and control groupsThere were no significant differences between the two groups in gender, height, weight, smoking status, hypertension, type 2 diabetes, or coronary heart disease. Significant differences were observed in age, BMI, left atrial diameter (LAD), and left ventricular ejection fraction (LVEF) (Table 1).
General comparisons between the atrial fibrillation and control groups.
| Group | AF group (n=64) | Control group (n=49) | t (chi-square) | p |
|---|---|---|---|---|
| Gender, male:female | 38:26 | 29:20 | 0.0004 | 0.983 |
| Age, years | 74.38±8.37 | 65.24±12.14 | 4.733 | <0.000 |
| Height, cm | 164.04±9.05 | 165.22±8.28 | 0.721 | 0.472 |
| Weight, kg | 70.61±11.19 | 67.09±12.51 | 1.551 | 0.123 |
| BMI | 26.13±3.57 | 24.33±3.52 | 507.6 (F value) | 0.000 |
| Smoking, n (%) | 28 (43.75%) | 20 (40.82%) | 0.098 | 0.754 |
| Type 2 diabetes, n (%) | 8 (12.50%) | 7 (14.19%) | 0.116 | 0.733 |
| Hypertension, n (%) | 34 (53.12%) | 29 (59.18%) | 0.413 | 0.520 |
| CHD, n (%) | 12 (18.75%) | 17 (34.69%) | 3.698 | 0.545 |
| LAD, mm | 42.91±10.90 | 35.67±4.54 | 4.365 | 0.001 |
| LVEF, mm | 53.59±9.59 | 58.29±9.33 | 2.612 | 0.010 |
AF: atrial fibrillation; BMI: body mass index; CHD: coronary heart disease; LAD: left atrial diameter; LVEF: left ventricular ejection fraction.
The ApoE alleles in the AF and control groups were quantified and their frequencies calculated. The theoretical frequencies of each genotype were then calculated according to the law of genetic equilibrium. Finally, the actual and theoretical frequencies of each genotype in the two groups were tested using the chi-square test. The control group test produced a p-value of 0.514, indicating that the law of Hardy-Weinberg equilibrium was applicable to the ApoE genotypes of the two groups, and that the collected data were credible and representative of the population (Table 2).
Hardy-Weinberg equilibrium test.
| Group | Genotype | p (Fisher) | |||||
|---|---|---|---|---|---|---|---|
| ɛ2/ɛ2 | ɛ2/ɛ3 | ɛ2/ɛ4 | ɛ3/ɛ3 | ɛ3/ɛ4 | ɛ4/ɛ4 | ||
| AF group (n=64) | 0.089 | ||||||
| Actual frequency | 1 | 8 | 2 31 | 16 | 6 | ||
| Theoretical frequency | 0.218 | 9.198 | 1.692 | 37.319 | 11.260 | 3.397 | |
| Control group (n=49) | 0.514 | ||||||
| Actual frequency | 0 | 7 | 1 35 | 6 | 0 | ||
| Theoretical frequency | 0.161 | 7.042 | 0.740 | 28.615 | 8.634 | 0.79 | |
AF: atrial fibrillation.
In this study, the proportions of the six ApoE genotypes (ɛ2/ɛ2, ɛ2/ɛ3, ɛ2/ɛ4, ɛ3/ɛ3, ɛ3/ɛ4, and ɛ4/ɛ4) were 0.9%, 13.2%, 2.7%, 58.4%, 19.5%, and 5.3%, respectively. Protective, high risk, and other genotypes accounted for 14.1%, 24.8%, and 61.1% of the samples, respectively. The frequency of the ɛ3/ɛ3 genotype was significantly lower in the AF group than in the control group, while the ɛ3/ɛ4 and ɛ4/ɛ4 genotypes were significantly more frequent in the AF group than in the control group (Table 3).
Distribution of apolipoprotein E polymorphisms in the atrial fibrillation and control groups.
| Genotype | Protected | Other | High risk | Summation, n (%) | |||
|---|---|---|---|---|---|---|---|
| ɛ2/ɛ2 | ɛ2/ɛ3 | ɛ2/ɛ4 | ɛ3/ɛ3 | ɛ3/ɛ4 | ɛ4/ɛ4 | ||
| AF group | 1 | 8 | 2 | 31 | 16 | 6 | 64 (39.5%) |
| Control group | 0 | 7 | 1 | 35 | 6 | 0 | 49 (60.5%) |
| p (Fisher) | 0.037 | ||||||
| Summation, n (%) | 1 (0.9% | 15 (13.2%) | 3 (2.7%) | 66 (58.4%) | 22 (19.5%) | 6 (5.3%) | 113 (100%) |
AF: atrial fibrillation.
The penetrance of ApoE3 was significantly lower in the AF group than in the control group, while the penetrance of ApoE4 was significantly higher in the AF group than in the control group (Table 4).
Regression analysis of factors correlating with atrial fibrillationUnivariate logistic regression analysis was performed with AF as the dependent variable and BMI, LAD, LVEF, ApoE2, and ApoE4 as independent variables. The results showed that age, BMI, LAD, LVEF, and ApoE4 were risk factors of AF (Table 5).
Regression analysis of factors correlating with atrial fibrillation.
| Risk factor | B | SE | p | OR | 95% CI |
|---|---|---|---|---|---|
| Age | Age | 0.011 | 0.002 | 0.001 | 1.011 |
| BMI | BMI | 0.268 | 0.069 | 0.000 | 1.307 |
| LAD | LAD | 0.018 | 0.003 | 0.002 | 1.018 |
| LVEF | LVEF | 0.039 | 0.003 | 0.001 | 1.049 |
| HDL | HDL | 1.031 | 0.508 | 0.042 | 0.357 |
| LDL | LDL | 0.482 | 0.291 | 0.097 | 1.620 |
| CRP | CRP | 0.253 | 0.104 | 0.015 | 1.288 |
| ApoE2 | ApoE2 | -0.018 | 1.029 | 0.973 | 0.982 |
| ApoE4 | ApoE4 | -0.625 | 0.072 | 0.000 | 3.754 |
BMI: body mass index; CI: confidence interval; CRP: C-reaction protein; HDL: high-density lipoprotein; LAD: left atrial diameter; LDL: low-density lipoprotein; LVEF: left ventricular ejection fraction; OR: odds ratio; SE: standard error.
LDL levels were higher in the AF group than in the control group, while high-density lipoprotein levels were lower. There were no significant differences in total cholesterol or triglyceride levels between the two groups (Table 6).
Comparison of blood lipid levels between the atrial fibrillation and control groups.
| TC | TG | HDL | LDL | |
|---|---|---|---|---|
| AF group, mmol/l | 4.79±1.13 | 1.37±0.68 | 1.23±0.35 | 2.71±0.58 |
| Control group, mmol/l | 4.88±1.19 | 1.45±0.61 | 1.37±0.39 | 2.49±0.55 |
| t | 0.548 | 0.853 | 2.556 | 2.632 |
| p | 0.584 | 0.395 | 0.011 | 0.009 |
HDL: high-density lipoprotein; LDL: low-density lipoprotein; TC: total cholesterol; TG: triglycerides.
The white blood cell count and percentage of neutrophils were higher in the AF group than in the control group, but these differences were not significant. hs-CRP levels were higher in the AF group than in the control group, and the difference was statistically significant (Table 7).
Comparison of inflammatory markers between the atrial fibrillation and control groups.
| Inflammation index | WBC, ×109 | Neutrophils, % | hs-CRP, mg/l |
|---|---|---|---|
| AF group | 7.26±2.04 | 0.63±0.12 | 5.61±2.12 |
| Control group | 6.90±1.83 | 0.61±0.11 | 4.85±1.46 |
| t | 1.254 | 1.312 | 2.856 |
| P | 0.211 | 0.191 | 0.005 |
AF: atrial fibrillation; hs-CRP: high-sensitivity C-reactive protein; WBC: white blood cell count.
ApoE, primarily expressed in the liver and brain, is an indispensable lipoprotein for physiological functions. Its most important function is to act as a ligand for the LDLR. Upon binding to the LDLR, ApoE enters liver cells, where it alters lipid metabolism and regulates lipid levels in the blood and brain.
Dyslipidemia is a recognized risk factor for atherosclerosis, and the incidence and severity of atherosclerosis are associated with the risk of AF.22 Previous studies concluded that high levels of LDL cholesterol are associated with a low risk of AF.23–25 However, other studies have shown no relationship between LDL and the occurrence of AF.22 In this study, univariate analysis showed that LDL was higher in the AF group than in the control group, and subsequent logistic regression analysis also showed that LDL was a risk factor for AF. Nevertheless, Alonso et al.26 concluded that total cholesterol is not related to the occurrence of AF, while other studies have suggested that it is associated with a low risk of AF.23–25 Our results showed no correlation between total cholesterol and AF. Generally speaking, although there is some controversy concerning the relationship between blood lipids and AF, it cannot be denied that ApoE may participate in the occurrence of AF by regulating blood lipids.
The slight effect of ApoE on blood lipid levels may not fully explain the effect of ApoE genetic polymorphisms on AF, because the development of AF is the result of many factors. This suggests that ApoE may have other biological functions and be involved in the occurrence of this disorder through other mechanisms.
Studies26,27 have reported that the occurrence and persistence of AF may be related to electrical and structural remodeling caused by electromechanical feedback associated with increased atrial diameter. In the current study, LAD in the AF group was greater than in the control group, and logistic regression analysis also showed that LAD was a risk factor for AF. Additional studies have found that ApoE has anti-inflammatory and antioxidant effects, and the order of these effects is ApoE2>ApoE3>ApoE4.28,29 The ApoEɛ4 allele lacks the anti-inflammatory properties of ApoEɛ2 and ApoEɛ3, but has a strong proinflammatory effect,27,30 which can lead to electrical and structural remodeling of the myocardium. This is supported by the higher hs-CRP levels in the AF group than in the control group in our study, as shown in Table 7. The mechanism may be as follows: ApoEɛ4 can activate NF-κB, resulting in the expression of monocyte chemoattractant protein-1 (MCP-1), TNF-α, IL-1β, IL-10, and other inflammatory mediators.16 MCP-1 can induce cardiomyocytes to express inflammatory cytokines including IL-1, IL-6, and TNF-α, causing negative cardiac inotropic effects, impairing cardiac function, and leading to myocardial structural remodeling.31,32 TNF-α may increase Ca2+ concentrations in cardiac myocytes,33 and downregulating L-type calcium channels leads to the shortening of action potential duration and the effective refractory period, and the formation of multiple reentry loops. At the same time, overloaded Ca2+ can activate calcium-activating proteins, leading to atrial contractile dysfunction through the degradation of cardiac troponin and other cardiac contractile proteins.34 This then results in atrial interstitial fibrosis, further leading to abnormal intra-atrial impulse conduction and atrial electrical remodeling. Taken together, these data support a correlation between AF and ApoE.
Many studies have shown that serum CRP is involved in the chemotaxis and activation of leukocytes and is an important marker of inflammatory responses.35 Chung et al.36 measured plasma CRP levels in 131 patients with atrial arrhythmias and 71 controls. They found for the first time that CRP was significantly increased in arrhythmias, confirming that inflammation may play an important role in the pathological mechanism of AF. At the same time, levels of plasma inflammatory markers are correlated with the burden of AF. CRP levels are significantly higher in patients with persistent AF than in patients with paroxysmal AF and normal controls. Our data also showed that plasma hs-CRP levels were significantly higher in the AF group than in the control group, indicating once again that CRP can be used as a marker of inflammation in AF and that inflammation plays an important role in the occurrence of AF.
Our results showed that there were no significant differences in gender, height, weight, smoking status, hypertension, type 2 diabetes, or coronary heart disease between the AF and control groups (p>0.05). However, we did observe significant differences in age, BMI, LAD, and LVEF. These findings suggest that older age, higher BMI, greater LAD, and lower LVEF increase the chance of AF. Advanced age is an independent risk factor for AF.23,37 Individuals with high BMI values may have high levels of body fat, which increases the prevalence of AF. Some studies have suggested that obesity is a risk factor for AF, and obese patients do in fact have a higher incidence and prevalence of AF, their disease is more serious, and it progresses faster.24 Obesity may increase the risk of AF through chronic inflammation caused by adipose factors. Taken together, our results suggested that ApoE may affect the occurrence of AF by regulating blood lipids and body mass. A greater LAD and low LVEF were mostly accompanied by myocardial electrical remodeling, structural remodeling, and fibrosis. These factors can easily lead to AF. In turn, the occurrence of AF will further increase LAD and decrease LVEF.
Six phenotypes, ɛ2/ɛ2, ɛ2/ɛ3, ɛ2/ɛ4, ɛ3/ɛ3, ɛ3/ɛ4 and ɛ4/ɛ4, were detected in 113 ApoE-genotyped subjects. The ɛ3/ɛ3 phenotype had the highest frequency, ɛ3/ɛ4 had the second highest frequency, and ɛ2/ɛ2 had the lowest frequency. ApoE genotypes can be divided into protective (ɛ2/ɛ2 and ɛ2/ɛ3), high-risk (ɛ3/ɛ4 and ɛ4/ɛ4), and others (ɛ2/ɛ4 and ɛ3/ɛ3). The risk of coronary heart disease, Alzheimer's disease, and stroke is average in patients with the ApoEɛ3 phenotype, lower for those with the ApoEɛ2 phenotype, and highest for those with the ApoEɛ4 phenotype. In this study, we found that the protective, high risk, and other genotypes accounted for 14.1%, 24.8%, and 61.1% of the sample, respectively. We also found that the distribution of the ApoE3 type accounted for 61.1% of the total, which is roughly consistent with previously published accounts.37 The high-risk ApoE4 genotypes accounted for 24.8% of the total. In this study, the ɛ3/ɛ3 genotype was significantly less frequent, while the ɛ3/ɛ4 and ɛ4/ɛ4 genotypes were significantly more frequent, in the AF group. The risk of AF in patients with ApoE4 (ɛ3/ɛ4, ɛ4/ɛ4) was the highest of all genotypic groups.
Finally, we found that penetrance of the ApoE4 phenotype was significantly higher in the AF group than in the control group. This may be related to the strong proinflammatory effect of the ɛ4 allele, which may be involved in the development of AF through the inflammatory pathway.14,16,38 Regression analysis of AF-related factors showed that the ApoE4 phenotype is an AF risk factor. ApoE4, as a risk phenotype, is likely to promote obesity, increased body fat content, and cardiovascular disease in patients with AF.39 Moreover, the role of ApoE4 in AF may be explained through the mechanisms of oxidative stress and inflammation.
LimitationsThe limitations of this study include its small sample size; lack of large-scale, multi-area sample testing; and the inability to monitor all blood samples throughout the entire process of preservation, transportation, and testing, which may have led to experimental errors.
ConclusionAlthough the mechanistic relationship between ApoE polymorphisms and AF is not completely understood, in the context of the previous literature, our results suggested that AF is affected to some extent by ApoE polymorphisms, particularly ApoE4, as ApoE4 was more closely correlated with AF. Additionally, among related factors, we also found that older patients and those with hypertension, greater LAD, and lower LVEF had higher incidences of atrial arrhythmias. To help prevent cardiovascular events, attention should be paid to interventions for atrial arrhythmias at the genetic and molecular level, to reduce the occurrence of atrial arrhythmias and their serious complications.
Future research directions include further exploration of the role of ApoE2 in AF, including the use of multi-regional population studies and improving long-term patient follow-up.
FundingThis project was funded by the High-level Health Personnel “Six One Project” Top Talent Scientific Research Project of Jiangsu Province (LGY2017065), the Science and Technology Bureau of Lianyungang City (SH1618).
Availability of data and materialsThe data that support the findings of this study are available from The Second People's Hospital of Lianyungang, Jiangsu, China.
Ethics approval and consent to participateThis study was approved by the institutional review board of the Second People's Hospital of Lianyungang Ethics Committee (no. L1618). All participants provided written informed consent.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank James P. Mahaffey, PhD, of Compuscript Ltd. for editing the English text of a draft of this manuscript.