Sarcopenia, which is characterized by the loss of skeletal muscle mass and function, is prevalent among patients with heart failure (HF) and negatively impacts their quality of life (QoL). The purpose of this study was to test the hypothesis that reduced muscle strength, as measured by handgrip strength (HGS), is independently associated with poorer quality of life (QoL) in patients with heart failure (HF).
MethodsThis cross-sectional study involved 114 patients with stable HF. HGS was assessed through a digital dynamometer; sarcopenia was defined by using gender-specific thresholds. Additional assessments included demographics, comorbidities, HF severity, frailty and QoL (the Kansas City Cardiomyopathy Questionnaire was used as a tool). To determine factors independently associated with QoL, a multiple linear regression model was obtained; we also derived a stepwise multiple linear regression model based on the Akaike Information Criteria.
ResultsAverage HGS was 20.9±8.4 kg and 54.5% of patients were classified as having probable sarcopenia. HGS demonstrated a positive correlation with QoL (r=0.46, p<0.001) and negative correlation with the New York Heart Association classification and the Clinical Frailty Scale. Multivariate analysis revealed that a higher HGS, a younger age, a lower NYHA class and lower frailty scores were significantly associated with a better QoL. A 10 kg increase in HGS was associated with an 8.7-point rise in KCCQ-23 scores.
ConclusionHandgrip strength is an independent predictor of QoL in patients with chronic HF. A regular assessment of HGS in clinical practice may help monitor the risk of sarcopenia and improve patient management, potentially enhancing daily functioning and QoL.
A sarcopenia, definida como a perda de massa e função muscular, é frequente em doentes com insuficiência cardíaca (IC) e afeta negativamente a qualidade de vida (QdV). O objetivo deste trabalho foi testar a hipótese de que menor força muscular, avaliada pela força de preensão manual (FPM), está independentemente associada a pior qualidade de vida em doentes com IC.
MétodosEstudo transversal incluiu 114 doentes com IC estável. A FPM foi avaliada com dinamómetro digital e a sarcopenia definida de acordo com o género. Avaliações adicionais incluíram dados demográficos, comorbilidades, gravidade da IC, fragilidade e QdV (Kansas City Cardiomyopathy Questionnaire). Para identificar os fatores associados de forma independente à QdV, utilizámos um modelo de regressão linear múltipla e um modelo de regressão linear stepwise baseado no critério de Akaike.
ResultadosA FPM média foi de 20,9±8,4 kg, com 54,5% dos doentes com sarcopenia provável. A FPM apresentou correlação positiva com a QdV (r=0,46, p<0,001) e negativa com a escala NYHA e a Escala Clínica de Fragilidade. Na análise multivariada, maior FPM, idade mais jovem, menor classe NYHA e menores scores de fragilidade estavam significativamente associados a melhor QdV. Um aumento de 10 kg na FPM foi associado a um aumento de 8,7 pontos no KCCQ-23.
ConclusãoA FPM é um preditor independente da QdV em doentes com IC crónica. A avaliação regular da FPM pode ajudar a monitorizar o risco de sarcopenia e a melhorar a gestão dos doentes, contribuindo para uma melhor funcionalidade diária e qualidade de vida.
Sarcopenia is defined as the loss of skeletal muscle mass and function. Despite being part of the normal aging process, it can accelerate and become more pronounced in the presence of chronic diseases.1 Sarcopenia could be found in 20–45% of heart failure (HF) patients2–4 and has a significant impact on their functional capacity and quality of life.3 The diagnosis can be confirmed by the existence of low muscle strength (evaluated by handgrip strength [HGS] or the chair stand test), in association with a low muscle quantity or quality (by means of magnetic resonance imaging or computed tomography).5 An isolated decrease in muscle strength identifies probable patients with sarcopenia.5 Muscle strength is also considered a better marker for adverse outcomes other than muscle mass.3,5 HGS correlates well with overall strength, making it a reliable and easy to measure biomarker.5
Handgrip strength is a valuable prognostic marker in HF and reduced strength is associated with higher mortality and worse outcomes.6,7 QoL is also a key clinical parameter in HF, as lower scores, assessed through validated tools like the KCCQ-23, increase hospitalization and mortality.6,7 Declining QoL correlates with disease progression.8
ObjectivesIn this study, we tested the hypothesis that decreased muscle strength, as evaluated by means of HGS, is independently associated with worse QoL in patients with HF.
MethodsStudy populationThe authors conducted a unicentric cross-sectional study that included all patients diagnosed with heart failure HF. These patients were evaluated consecutively at an outpatient HF clinic in a tertiary hospital between January 2020 and March 2022.
Patients were included if they had a HF diagnosis according to 2021 European Society for Cardiology Guidelines for the diagnosis and treatment of acute and chronic HF.2 Also, clinical stability in the previous three months was mandatory, defined by the following: the absence of (i) exacerbations observed in the emergency department or hospitalization in the previous 3 months; (ii) therapeutic changes and (iii) worsening of symptoms (defined by ≥1 point increase in NYHA class), according to New York Heart Association (NYHA) Functional Classification. The exclusion criteria included the following conditions: (i) group D chronic obstructive pulmonary disease; (ii) a history of pulmonary thromboembolism within the past 6 months; (iii) advanced dementia, end-stage renal disease, cirrhosis classified as CHILD-PUGH B or C, active cancer, HIV infection, or substance abuse; (iv) cardiothoracic surgery, acute myocardial infarction, or stroke occurring within the last three months; (v) surgery performed within the previous 30 days; (vi) diseases that could affect hand strength, such as stroke, trauma, or carpal tunnel syndrome; and (vii) inability to walk.
All participants provided written informed consent upon enrollment. The hospital ethics committee approved the protocol.
Muscle strength assessmentMuscle strength was assessed using HGS measurement. A calibrated Camry Digital Hand EH-101® dynamometer was utilized. Participants sat quietly with their arms outstretched parallel to the trunk, the shoulder adducted in neutral rotation with the elbow flexed to 90°. They were instructed to apply maximum strength with their dominant hand using the dynamometer. The peak force achieved during a five second trial was evaluated. For each patient, the mean of three consecutive HGS evaluations (in kilograms) was calculated. Sarcopenia was defined by using the cut-off points proposed by European consensus on the definition and diagnosis of sarcopenia, adjusted for gender (<27 kg for men and <16 kg for women).5 In addition to muscle strength, we also collected the following variables at the same appointment: demographic data (gender and age), comorbidities to allow for calculation of Charlson Comorbidity Index (CCI), body mass index (BMI), HF characterization (ejection fraction and etiology), frailty, HF symptoms and QoL.
Heart failure symptoms assessmentThe severity of HF symptoms was evaluated using the NYHA Functional Classification which organizes patients into one of four categories based on their limitations during physical activity.
Frailty assessmentFrailty assessment was obtained using a Portuguese validated version of the Clinical Frailty Scale (CFS).9 The CFS is a validated scale that includes clinical/functional and cognitive items, designed to assess the degree of vulnerability of an individual based on clinical judgment. This evaluation takes into account factors such as cognition, mobility, functionality, comorbidities, and the individual's medical history and physical examination. This procedure must be carried out by a healthcare professional. The CFS score places patients into one of nine categories: 1 – very fit, 2 – well, 3 – managing well, 4 – vulnerable, 5 – mildly frail, 6 – moderately frail, 7 – severely frail, 8 – highly frail and 9 – terminally ill. Patients scoring ≥5 are considered frail.
Quality of life assessmentQuality of life was assessed by applying the validated Portuguese version of the KCCQ-23.10 This questionnaire covers seven clinically relevant domains: physical limitations (question 1), symptoms (frequency [questions 3, 5, 7 and 9], severity [questions 4, 6 and 8] and change over time [question 2]), self-efficacy and knowledge (questions 11 and 12), social interference (question 16) and QoL (questions 13–15).11 Responses are scored by assigning an ordinal value to each one, where 1 represents the lowest level of functioning level. The values are then summed within each domain. Missing values are replaced with the average of the answered items within the same domain. Scale scores are transformed into a 0–100 range, by subtracting the lowest possible scale score, dividing that by the range of the scale and then multiplying by 100.11 The scores obtained indicate a specific health status. Scores between 0 and 24 reflect a very poor to a poor QoL; 25 and 49 a poor to a fair QoL; 50 and 74 a fair to a good QoL and 75 and 100 a good to an excellent QoL.12
Statistical analysisDescriptive statistics were used to describe the study population at baseline. Discrete variables are reported as frequencies and percentages, whereas continuous variables are presented as mean and standard deviation or median and interquartile range according to their distribution. The normality of distributions was assessed using the Kolmogorov–Smirnov test.
Univariate analysis was performed using simple linear regression and a Pearson's correlation test to evaluate the correlation between HGS and other variables of interest. To identify the factors independently associated with QoL, we utilized a multiple linear regression model that included variables with a p-value <0.2 from the univariate analysis (Model 2). In addition, we developed a stepwise multiple linear regression model based on the Akaike Information Criteria (Model 3). Statistical analysis was performed using R for Windows. Statistical significance was set at p-value <0.05.
ResultsDuring the inclusion period, a total of 178 patients with HF were identified, but only 114 met the study inclusion criteria. Figure 1 summarizes the sample selection and reasons for exclusion.
The study population characteristics are presented in Table 1. A total of 25 (46.3%) males were included, with a mean age of 74.8±10.2 years. The population was complex and characterized by multiple comorbidities – median Charlson Comorbidity Index of 5 (4–6) points. The mean BMI was 29.2±5.5 kg/m2. Applying the CFS, 49% presented a CFS ≤3. The median ejection fraction (EF) was 50 (40.5–57.5)%, with only one fourth of the patients presenting HFrEF. Regarding symptom severity, most patients were in NYHA class II (59.3%). Hypertensive and valvular etiologies accounted for 22.2% and 18.5% of cases, respectively. Only 11.1% of patients had ischemic etiology.
Demographic and descriptive data.
| Total (n=55) | |
|---|---|
| Male (n (%)) | 25 (46.3) |
| Age (years, mean±SD) | 74.8±10.2 |
| CCI (points, median (IR)) | 5 (4–6) |
| BMI (kg/m2, median (IR)) | 29.2±55 |
| Heart failure characterization | |
| EF (%, median (IR)) | 50 (40.5–57.5) |
| HFpEF (frequency (%)) | 26 (48.1) |
| HFmrEF (frequency (%)) | 13 (24.1) |
| HFrEF (frequency (%)) | 14 (25.9) |
| Symptoms | |
| NYHA I (frequency (%)) | 11 (20.4) |
| NYHA II (frequency (%)) | 32 (59.3) |
| NYHA III (frequency (%)) | 11 (20.4) |
| HF etiology | |
| Valvular (frequency (%)) | 10 (18.5) |
| Ischemic (frequency (%)) | 6 (11.1) |
| Hypertensive (frequency (%)) | 12 (22.2) |
| Arrhythmia (frequency (%)) | 6 (11.1) |
| Infiltrative (frequency (%)) | 2 (3.7) |
| Toxic (frequency (%)) | 3 (5.6) |
| Others/in evaluation (frequency (%)) | 15 (27.8) |
| Treatment | |
| ACEI/ARA | 33 (61.1) |
| Spironolactone | 28 (51.9) |
| SGLT2i | 15 (27.8) |
| Sacubitril/valsartan | 9 (16.7) |
| Beta-blockers | 49 (90.7) |
| KCCQ-23 (points, mean±SD) | 67.2±24.2 |
| >75 points (frequency (%)) | 24 (44.4) |
| 50–74 points (frequency (%)) | 18 (33.3) |
| 25–49 points (frequency (%)) | 10 (18.5) |
| <25 points (frequency (%)) | 2 (3.7) |
| HGS (kg, mean±SD) | 20.9±8.4 |
ACEI: angiotensin converting enzyme inhibitors; ARA: aldosterone receptor antagonist; BMI: body mass index; CCI: Charlson Comorbidity Index; EF: ejection fraction; HFmrEF: heart failure with mildly reduced ejection fraction; HFpEF: heart failure with preserved ejection fraction; HFrEF: heart failure with reduced ejection fraction; HGS: handgrip strength; IR: interquartile range; KCCQ-23: Kansa City Cardiomyopathy questionnaire; SD: standard deviation; SGLT2i: Sglt2 inhibitors.
According to the KCCQ-23, QoL was rated as good to excellent in 44.4% of the patients, fair to good in 33.3% of the patients, poor to fair in 18.5% of the patients and very poor to poor in 3.7% of the patients.
Sarcopenia was present in 54.5% of patients, with no significant differences between genders (men: 60%; women: 50%, p=0.458).
The mean HGS was 20.9±8.4 kg. When comparing the HGS between the four categories of KCCQ-23, good to excellent QoL was associated with higher HGS (23.6±9 kg) than fair to good (20.2 (16.4–24.1) kg), poor to fair (14.5 (12.3–14.5) kg) and very poor to poor (11.6 (9.5–11.6) kg) (p=0.02).
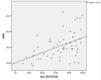
Figure 2 depicts a scatterplot that shows the correlation between HGS and QoL. Overall, these variables correlated positively, with a v Pearson's r value of 0.46 (p<0.001). Besides QoL, HGS negatively correlated with other variables, namely NYHA class (r=−0.33; p=0.016) and CFS (r=−0.50; p<0.001) (Supplementary material).
In the univariate analysis (Table 2), age (β=−0.18, p=0.012), HGS (β=1.3, p<0.001), NYHA scale (β=−28, p<0.001) and CFS (β=−13.0, p<0.001) were found to be significantly associated with QoL. On multivariable analysis (Table 2, Model 3), the effects of age, HGS, NYHA scale and CFS remained significant. For each increase in one NYHA class, QoL decreased 20 points on the KCCQ-23, whereas for each 10 kg increase in HGS, QoL increased 8.7 points on the KCCQ-23. Additionally, for every 10-year increase in patient age, there was an improvement of 6.9 points in the KCCQ-23 score. Conversely, an increase in the category of the CFS was associated with a decline of 6.0 points in quality of life as measured by the KCCQ-23.
Univariate and multivariate analyses considering KCCQ-23 as dependent variable.
| Univariate analyses | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| β | (95% CI) | p | β | (95% CI) | p | β | (95% CI) | P | |
| Female | −13.0 | (−25; 0.42) | 0.058 | 1.4 | (−8.1; 11) | 0.773 | – | – | – |
| Age | −0.81 | (−1.4; −0.19) | 0.012 | 0.73 | (−0.01; 1.5) | 0.059 | 0.69 | (0.14; 1.2) | 0.014 |
| HGS | 1.3 | (0.62; 2.0) | <0.001 | 0.89 | (0.17; 1.6) | 0.020 | 0.87 | (0.24; 1.5) | 0.007 |
| NYHA | −28.0 | (−35; −21) | <0.001 | −19 | (−29; −9.4) | <0001 | −20.0 | (−29; −11) | <0.001 |
| CFS | −13.0 | (−17; −9.3) | <0.001 | −6.6 | (−12; −1.6) | 0.013 | −6.0 | (−11.0; −1.2) | 0.016 |
| CCI | −2.9 | (−7.2; 1.5) | 0.193 | −1.1 | (−4.4; 2.1) | 0.497 | – | – | – |
| BMI | −0.95 | (−2.2; 0.26) | 0.122 | −0.21 | (−1.1; 0.69) | 0.645 | – | – | – |
Model 2 – multivariate analyses considering p<0.2 at univariate analyses as inclusion criteria; Model 3 – step wise model.
BMI: body mass index; CCI: Charlson Comorbidity Index; CFS: Clinical Frailty Scale; CI: confidence interval; HGS: handgrip strength; KCCQ-23: Kansa City Cardiomyopathy questionnaire.
In this research, the association between HGS, as a marker of muscle strength, and HF symptoms, frailty and QoL was studied in a population of patients with chronic HF.
Fifty-five percent of patients (54.5%) were identified as having probable sarcopenia according to the HGS evaluation. The term probable sarcopenia is relatively recent, having been introduced in 2019 by the European Working Group on Sarcopenia in Older People 2 (EWGSOP2).13 Due to the lack of consensus on sarcopenia assessment methods and the novelty of this definition, determining the exact prevalence of pre-sarcopenia remains challenging. However, studies estimating the prevalence of sarcopenia in patients with HF report rates ranging from 34% to 66% and highlight the high burden of muscle dysfunction in this population.14
Handgrip strength independently predicted the quality of life in this population. Currently, the goals of HF patient management include improving symptoms and QoL, in addition to increasing survival.15 QoL was also identified as an independent predictor of mortality and hospitalization for HF.15
Several pathophysiological mechanisms have been proposed to explain the onset of sarcopenia in patients with HF including malnutrition, inflammation, hormonal changes, oxidative stress, autophagy, and apoptosis.16 A sub-analysis of the SICA-HF trial reported a sarcopenia prevalence of 19.5%.17 However, SICA-HF defined sarcopenia solely based on the evaluation of muscle mass using dual-energy X-ray absorptiometry, which may underestimate the true prevalence of sarcopenia. Additionally, although patients with muscle wasting showed significantly lower HGS, there were no significant differences in the ratio of muscle strength to muscle mass between those with and without muscle wasting.17 In the absence of confirmation of low muscle quantity or quality a diagnosis of sarcopenia cannot be accurately established. As a result, relying solely on HGS evaluation may lead to an overestimation of the presence of sarcopenia, even though muscular strength is considered a better predictor of adverse outcomes than mass.3,5 Nevertheless, this sample of patients with HF shows a worrying prevalence of reduced HGS, suggesting a likely presence of sarcopenia.
In this sample, 49% of patients were not considered frail as they presented CFS ≤ 3. A high percentage (70%) of frailty was described in the FRAIL-HF study among patients hospitalized for HF aged ≥70 years old.18 Although the mean age in this study was similar (74.8±10.2 years), patients <70 years old were not excluded. Also, patients followed in outpatient clinics may have had more stable disease, presenting HF in earlier stages and characterized by fewer physically limiting comorbidities. This may have been reflected in a lower prevalence of frailty. A close follow up of frail patients by the HF team, with regular symptom monitoring and medication adjustment is important to prevent worsening of frailty and HF decompensation.3
Handgrip strength is positively correlated with QoL and negatively with NYHA class and CFS. As expected, physical health and functioning contribute to QoL and are negatively impacted by sarcopenia.19 Independent predictors of QoL in patients with HF included HGS, NYHA scale, the CFS, and age. These results were robust since the findings from Model 2 were quite similar to those from Model 3. For every 10 kg increase in HGS, the KCCQ-23 QoL score improved by 8.7 points.
The NYHA class worsening is a well-known factor in decreasing QoL in chronic HF.16 Physical inactivity is common in frail patients due to the progression of HF. These patients often experience impaired exercise capacity and limitations in everyday activities, which contribute to muscle loss.3 Sarcopenia is age-related, and the estimated annual decline in muscle strength is 1.5% after 50 years old.1,3 Even after adjusting for NYHA class, age and frailty, HGS remains an independent predictor of QoL in patients with HF.
In this study, an older age was independently associated with a better QoL, a finding that appears counterintuitive as aging is typically associated with increased comorbidity burden, functional decline and higher HF severity. This association may reflect survival bias, as older patients attending specialized HF clinics may represent a subgroup with better disease management and physiological resilience. Moreover, psychosocial adaptation mechanisms could influence this relationship, with older patients potentially developing more effective coping strategies and adjusted expectations regarding their health status.20 Further longitudinal studies are warranted to explore these hypotheses and clarify the causal pathways underlying this association.
Body mass index was not an independent predictor of QoL. BMI does not seem to be a good indicator of adiposity and has a better relationship with lean body mass in patients with HF, which is associated with better HGS.21 Oreopoulos et al. found that BMI, lean body mass and percent body fat were not associated with QoL.21 Lilamand et al. described a population of hospitalized geriatric patients with heart disease, finding that malnutrition, regardless of BMI, was an independent predictor of QoL.16
Also, a 2018 metanalysis showed that HGS is predictive of cardiac death, all causes of death and HF hospitalization in patients with cardiac disease including HF and ischemic heart disease.22 Sarcopenia impacts the functional capacity of patients with HF and is associated with an increased risk of adverse events (falls, fractures, a worse neurocognitive profile, and a low physical performance).3
Both resistance training and aerobic exercise are crucial for managing sarcopenia and improving physical performance.14 In patients with HF and sarcopenia, aerobic activity is associated with reduced hospitalizations and mortality, likely due to decreased inflammation and increase in muscle cross-sectional area.14 Nutritional interventions, especially adequate protein intake and essential nutrients, play a crucial role in mitigating the effects of sarcopenia.14 The implementation of strategies aiming to increase muscle strength and delay the onset of frailty may improve QoL for patients living with HF and reduce hospitalization and mortality. This is particularly important as HF is an increasing problem, particularly among older adults.23
Handgrip strength could be useful, not only as a clinical marker, but also as a patient awareness tool for promoting physical activity. Since sarcopenia can be mitigated through lifestyle interventions, routinely assessing and sharing HGS results with patients may encourage them to take part in physical exercise programs. Future studies should explore whether integrating HGS monitoring into HF management could enhance patient engagement and improve outcomes.
There are limitations to this study that must be acknowledged. First, a control group was not included in this study, which makes it more difficult to distinguish the effects of aging worsening HGS from muscle loss attributable to HF. Secondly, body composition, lean body mass or levels of leisure time/physical activity were not assessed; only the maximum HGS peak was evaluated. This neglects other variables of interest in the HGS evaluation, such as force development rate and strength loss rate between the peak and final strength. Thirdly, by using CCI to evaluate comorbidities, important factors that may further impact sarcopenia and QOL have potentially been overlooked, such as anemia or depression. Finally, some disease-modifying drugs, such as sacubitril-valsartan and SGLT2i,24–26 have been associated with improvements in QoL. However, due to the different therapeutic indications for each drug, considering the EF and the reduced number of patients taking these drugs, they were not considered in the analysis.
Due to the observational nature of the study, a causal relation between sarcopenia and worst QoL cannot be ascertained. Whether sarcopenia leads to a worse QoL in HF or whether disease progression leads to inactivity and a worse QoL remains to be determined. Longitudinal and interventional studies targeting muscle mass and strength are needed to clarify these associations. Such studies would allow us to determine whether an improvement in sarcopenia could lead to reduced symptoms and a better QoL in patients with HF. The small sample size also did not allow us to perform a separate analysis for patients with and without preserved EF. In fact, EF was not associated with QoL, as assessed by the KCCQ-23, in the univariate analysis.
This study was conducted in a tertiary hospital, where patients often have more advanced HF and a higher burden of comorbidities. Assessment in primary care settings could help to understand whether sarcopenia also affects QoL in the earlier HF stages. It could also show us whether early interventions, like exercise and nutrition programs, help prevent muscle decline and improve outcomes.
ConclusionIn conclusion, there is a high prevalence of HGS reduction in patients with chronic HF. HGS is positively correlated with QoL and negatively with symptoms in HF. The authors identified HGS as an independent predictor of QoL in patients with chronic HF, with every 10 kg decrease in HGS associated with an 8.7-point decrease in KCCQ-23.
Handgrip strength, which is easily measured in an outpatient clinic, can be a useful tool in assessing and monitoring sarcopenia risk in patients with HF, whose strength may be a limiting factor for daily activities and QoL.
Future intervention studies aiming to improve muscle strength could help clarify the causal relationship between sarcopenia and QoL while also providing insights into long-term patient outcomes.
Ethics statementThe study was conducted in accordance with ethical principles and approved by the Unidade Local de Saude Gaia e Espinho Ethics Committee. All participants provided written informed consent.
Conflicts of interestThe authors declare no conflicts of interest.