Air pollution is one of the main environmental risk factors for health and is linked to cardiovascular diseases, which are the leading cause of mortality worldwide.
In this position paper, we discuss the main air pollutants and how they can promote the development of cardiovascular disease or cardiovascular events. We also summarise the main evidence supporting the association between air pollution and cardiovascular events, such as coronary events (acute coronary syndromes/myocardial infarction; chronic coronary syndromes), stroke, heart failure and mortality. Some recommendations are made based on these data and the European Society of Cardiology guidelines on cardiovascular disease prevention, acknowledging that it is important to increase awareness and literacy on this topic in Portugal.
A poluição do ar é um dos principais fatores de risco ambiental para a saúde e está associada à principal causa de morte em todo o mundo que são as doenças cardiovasculares. Neste position paper discutimos a forma como os principais poluentes atmosféricos podem promover o desenvolvimento de doenças ou eventos cardiovasculares. Também agregámos a melhor evidência que suporta a associação entre poluição do ar e eventos cardiovasculares, como eventos coronários (síndromes coronárias agudas/enfarte do miocárdio; síndromes coronárias crónicas), acidente vascular cerebral, insuficiência cardíaca e o risco de morte. Foram feitas recomendações de acordo com a evidência, os dados nacionais e as orientações da Sociedade Europeia de Cardiologia sobre prevenção de doenças cardiovasculares, reconhecendo que é importante aumentar a sensibilização e literacia sobre este tema em Portugal.
Cardiovascular diseases (CVDs) are the leading cause of mortality worldwide according to World Health Organization (WHO) data.1 In 2019, approximately 19 million people died due to cardiovascular (CV) causes, the majority due to myocardial infarction and stroke. CVDs account for approximately one third of all premature deaths, before the age of 70, due to noncommunicable diseases. Expectedly, ischemic heart disease and stroke were the no-communicable leading causes of disease burden in 2019.2
The risk for CV disease derives from genetics, lifestyle and environmental factors. CVDs share some modifiable risk factors that can be addressed individually such as smoking, sedentarism, unhealthy dietary habits, hypertension, dyslipidemia, diabetes, and obesity. One environmental risk factor that is unavoidable for most people is pollution.
Pollution exists in many forms such as air pollution, soil pollution, water pollution, noise pollution, among other types. Air pollution is the single biggest environmental health risk factor, including cardiovascular risk and its importance needs to be highlighted as the risk of death is at least similar to that of exposure to smoking.3–5
Air pollutionAir pollution is the contamination of the indoor or outdoor environment by any chemical, physical or biological agent that modifies the natural characteristics of the air.1 Usually the concept of air pollution refers to a combination of heterogeneous and complex fluids, gases, and particulate matter (PM).6
The main source of indoor air pollution varies geographically but comes essentially from cooking and heating using inefficient fuels and/or the use of traditional stoves, but also from the use of consumer products such as cleaning surface pesticides and solvents, among other sources.7,8 Outdoor air pollution derives from road traffic, emissions from industries, agricultural, trash or wildfire and released indoor pollution.
The components of air pollution thought to be involved in cardiovascular risk are nitrogen dioxide (NO2), carbon monoxide (CO), and sulfur dioxide (SO2), as well as PM, and others such as ozone (O3) or volatile organic compounds.9
Particulate matter (PM) is classified in three groups according to the particles size: Coarse particles (PM10, diameter <10 and ≥2.5 μm), fine particles (PM 2.5, diameter <2.5 μm), and ultrafine particles (<0.1 μm).
The main source of PM is road traffic; the emitted particles can reach the respiratory airways. The likelihood of reaching the distal airways increases the smaller the PM is. Airborne PM can result from direct emissions into the atmosphere or can be the result of a reaction with other substances in the atmosphere. Combustion processes are the main source of primary particle emission into the atmosphere, while road traffic is the primary cause of emissions in urban areas.10
Sulfur dioxide (SO2) is generally produced from the burning of fossil fuels such as coal and oil and the smelting of mineral ores, including aluminum, copper, zinc, lead, and iron, which contain sulfur. Industrial facilities and maritime transport are the main sources of SO2 emissions. Road traffic (mainly from diesel vehicles) is the main source of NO2.11,12
Ozone is formed through a photochemical reaction involving sunlight and gaseous precursors such as NO2 or volatile organic compounds, which can explain why ozone pollution typically occurs on warm and sunny days.12,13
In Portugal, road traffic and industries are the main source of pollutants, but seasonally the forest wildfires are other relevant sources of air pollution. The main pollutants resulting from biomass burning are CO, NO2, SO2 and PM. According to the WHO, exposure to smoke from forest fires, particularly to suspended PM, has been associated with respiratory and cardiovascular diseases, and even with increased mortality.14
Regarding indoor environment, second-hand smoke is the major source of air pollution, globally. In Europe, outdoor PM 2.5 inside penetration via air exchange is also a major factor responsible for indoor pollution.15
Pathophysiology of the cardiovascular effects of air pollutionThere are three possible mechanisms that explain the cardiovascular effects of air pollution which are not mutually exclusive: 1) Lung inflammation with systemic inflammatory and oxidative mediators; 2) Translocation of particles with vascular deposition; 3) Autonomic nervous system dysregulation.
Regarding the inflammatory/oxidative hypothesis, it is known that common air pollutants, such as NO2, O3 and PM are pro-oxidant. Exposure to these inhaled pollutants can lead to oxidative stress, through different cellular mechanisms, such as the uncoupling of nitric oxide synthetase, mitochondrial dysfunction and formation of reactive oxygen species.16 Prolonged exposure to this pollutants can lead to a chronic low-level inflammation in the lungs17 and the process can extend systemically.18 Systemic inflammatory mediators can influence the atherosclerotic process, which, in the worst-case scenario, can lead to rupture of plaques and subsequent acute coronary or cerebrovascular syndromes.19–22
Some small pollutant particles can cross the alveolar-capillary membrane and circulate in the blood influencing the cardiovascular system directly.23 PM exposure is linked to abnormal activation of the hemostatic system, leading to a pro-coagulant and antifibrinolytic state.19,24,25 Exposure to air pollutants also induces some endothelial injuries, leading to an increase of endothelial cell apoptosis, a decreased circulating level of endothelial progenitor cells and tight junction protein degradation.6,26,27 After PM inhalation, we observe a rise in interleukin-6, which leads to increased fibrinogen, factor VIII and tissue factor release.19,21 A disrupted endothelial cell barrier, an increase in coagulation factors, a reduction in fibrinolytic capacity and platelet activation, all represent plausible pathophysiological mechanisms to promote thrombus formation.28,29 Recent studies also show that inhaled nanoparticles can go into systemic circulation and accumulate in common sites of atherosclerosis; a direct toxic interaction is plausible.30
Inhaled pollutants activate alveolar receptors that may also influence autonomic nervous system, impairing autonomic balance and favoring sympathetic over parasympathetic tone. Autonomic balance impairment may contribute to increased cardiovascular risk through the induction of pro-hypertensive vasoconstriction and the predisposition to arrhythmias.31,32
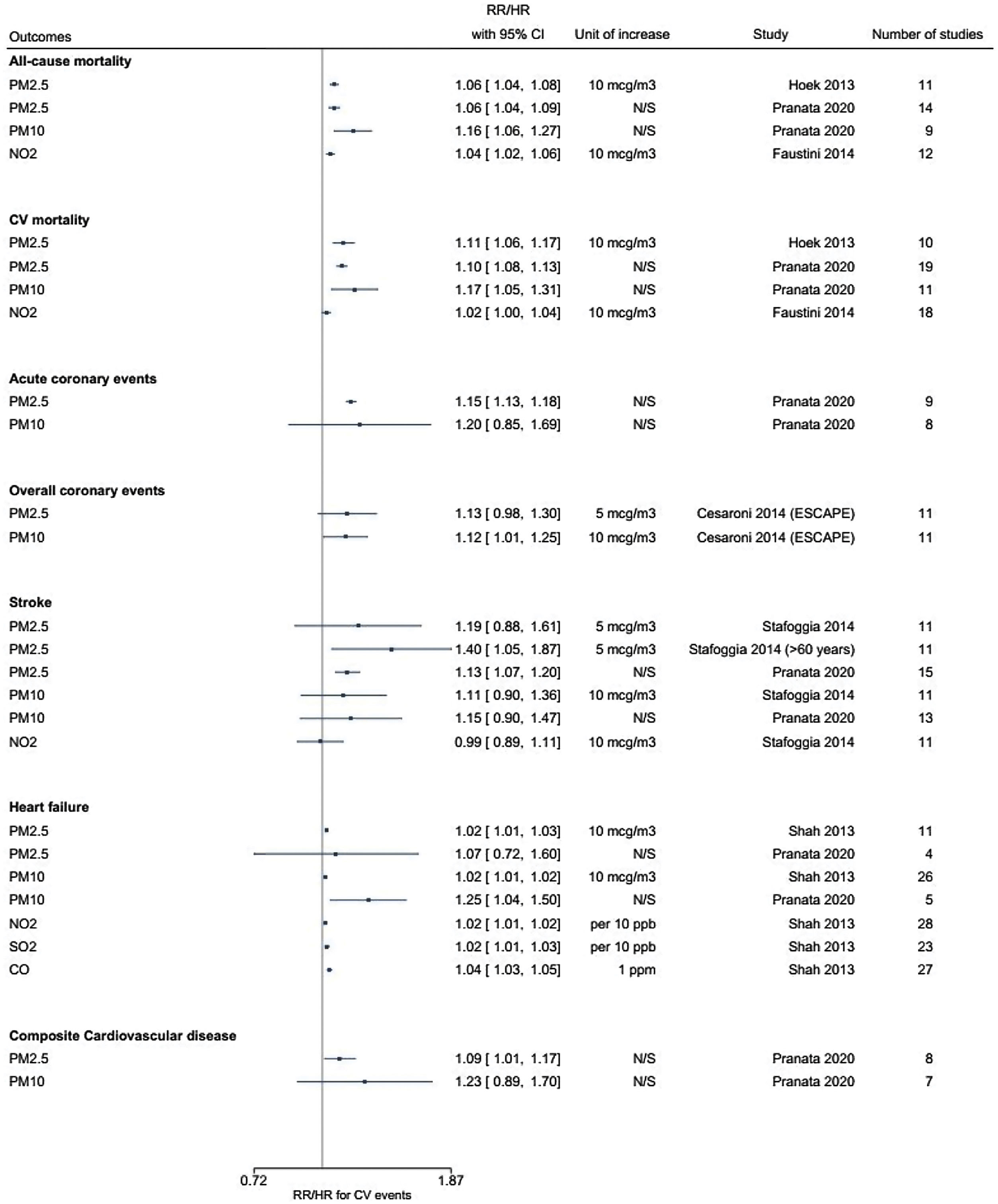
Review of the evidence for the association between air pollution and cardiovascular eventsIn order to review the association between air pollution and cardiovascular events, a search was performed in MEDLINE to retrieve the main reviews and consensus documents to identify aggregated evidence in systematic reviews using the keywords “air pollution”, “coronary disease”, “myocardial infarction”, “stroke”, “heart failure”. The authors selected publications based on when they were updated and their representativeness.
The six systematic reviews included were published between 2013 and 2020 and focused on long- and short-term effects of air pollutants on cardiovascular diseases (CVD).12,16,33–36 Their main characteristics are shown in Table 1. All reviews evaluated long-term exposure, except for Shah et al. that assessed the effect of short-term exposure to ambient air pollution on CVD.36 One review (Hoek et al.) focused on the effect of PM, four reviews assessed PM and nitrogen oxides,12,33–35 and Shah et al. studied the effect of PM, NO2 and other air pollutants (SO2, CO, O3) in cardiovascular outcomes.
Main characteristics of selected systematic reviews assessing the impact of air pollutants in cardiovascular events.
| Study | Publication year | Location | Exposure temporality | No. Studies included | Study design | Air pollution exposure variables | Subjects (n) | Population | Main findings |
|---|---|---|---|---|---|---|---|---|---|
| Pranata et al. | 2020 | China, Taiwan, South Korea, Japan, US, Canada, Europe, UK, Sweden, Italy, Netherlands, Denmark, Greece, Switzerland | Long-term exposure | 49 | Cohort studies | PM2.5; P10; NO2 | 28 215 394 | Adults, both sexes | Air pollutants (PM 2.5, PM10, NO2) are associated with an increased incidence of CVD, all-cause mortality, and CVD mortality |
| Hoek et al. | 2013 | US, Canada, China, Japan, Germany, Sweden, Italy, Netherlands, Switzerland, France, Scotland, Denmark, New Zealand | Long-term exposure | 39 (30 related to cardiovascular disease) | Cohort studies | PM2.5 | NR | Adults, both sexes | Long-term exposure to PM2.5 is associated with mortality from CVD |
| Faustini et al. | 2014 | US, Canada, Sweden, Germany, Italy, Norway, France, Netherlands, China, Japan, New Zealand | Long-term exposure | 23 | Cohort and case-control studies | PM2.5; NO2 | NR | Adults, both sexes | The authors reported a 13% and 20% increase in cardiovascular mortality after a 10 μg/m3 increase in NO2 and PM2.5 concentrations, respectivelyThe authors observed a similar risk estimate for all-cause mortality in studies investigating the long-term effects of both NO2 and PM2.5 (4% versus 5% increase, respectively) using an exposure metric of 10 μmg/m3 |
| Shah et al. | 2013 | USA, Canada, Italy, Asia, Taiwan, Japan, Hong Kong, Australia, New Zealand, Brazil, South Korea, UK, Netherlands | Short-term exposure | 35 | Time-series, Case-crossover | CO; NO2; SO2; O3; PM2.5; PM10 | NR | Adults, both sexes | Air pollution has a close temporal association with heart failure hospitalization and heart failure mortality |
| Stafoggia et al. (ESCAPE Project) | 2014 | Europe (Finland, Sweden, Denmark, Germany, and Italy | Long-term exposure | 11 | Cohort studies | PM2.5; PM10; nitrogen oxides | 99 446 | Adults, both sexes | Authors reported a positive association between PM2.5 and cerebrovascular events even for exposure levels below the current European limits |
| Cesaroni et al. (ESCAPE Project) | 2015 | Europe (Finland, Sweden, Denmark, Germany, and Italy) | Long-term exposure | 11 | Cohort studies | PM2.5; PM10; nitrogen oxides | 100 166 | Adults, both sexes | Authors reported an increased incidence of coronary events in adults exposed to particulate matter (PM2.5 and PM10), even for exposure levels below the current European limits. |
NR: Not reported; PM: Particulate matter; US: United Sates; UK: United Kingdom.
Hoek et al. showed that with a 10 mcg/m3 increase in PM2.5, overall mortality increased by 6% and cardiovascular mortality by 11%.16 All-cause mortality was also raised with an increased exposure to elemental carbon and NO2.16
Cesaroni et al. focused on the association between long-term exposure to PM and NO2 and the incidence of acute coronary events in 11 cohorts participating in the European Study of Cohorts for Air Pollution Effects (ESCAPE project). The authors observed a positive association between long-term exposure to PM and the incidence of coronary events.33
Stafoggia et al. assessed the effect of long-term exposure to PM within the 11 cohorts included in the ESCAPE project. The authors found a positive association between long-term exposure to PM2.5 and stroke incidence especially among participants ≥60 years of age and among those who had never been smokers.34
Cesaroni et al. and Stafoggia et al. highlighted the harmful effects of PM even at low concentrations, since they observed a positive association between long-term exposure to PM and the incidence of coronary events and stroke, respectively, for exposure levels below the current European limits.33,34
Regarding other air pollutants, Shah et al. reported that increases in CO and SO2 were associated with heart failure (HF) hospitalization or death (3.52% per 1 part per million (95% confidence interval [CI] 2.52-4.54) and 2.36% per 10 parts per billion [95% CI 1.35-3.38], respectively).36 Increases in O3 concentration were not associated with HF hospitalization or death (0.5% per 10 parts per billion, 95% CI -0.10 to 1.02).36
Pranata et al. analyzed other CVD outcomes including ischemic heart disease (IHD), hypertension, and atrial fibrillation (AF), reporting a positive statistical association between long-term exposure to PM and NO2 and increased incidence of IHD, hypertension, and AF.35
Overall, all reviews reported that exposure to increased levels of air pollution was consistently associated with several important adverse cardiovascular health outcomes (Figure 1).
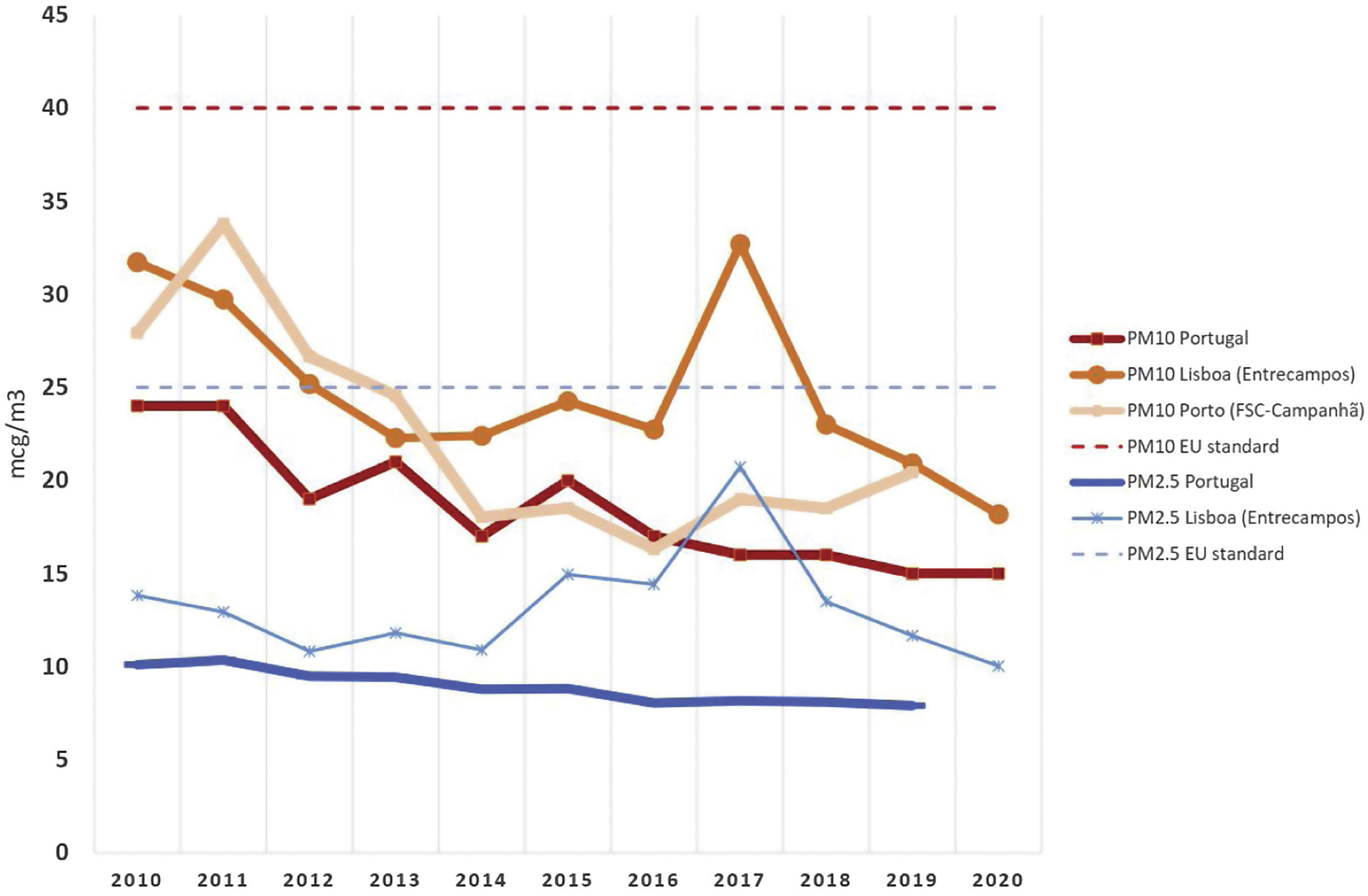
Air pollution indexes in PortugalThe indexes of air pollution in Portugal have been declining. The PM indexes are currently lower than the annual threshold recommended by the European Union Ambient Air Quality Directives (Figure 2). Even though, as seen in Figure 2, the quality of the air regarding both PM2.5 and PM10 in larger cities such as Lisbon and Porto is lower than average, it suggests that there are geographic discrepancies as regards air pollution. In line with these data, the 2020 Quality of Air Report states that in Portugal, it is estimated that yearly PM2.5 might be responsible for 4900 premature deaths and 53 000 years of life lost (YLL), using 2018 estimates. Premature deaths attributable to NO2 and O3 exceed altogether 1000 and the YLL also exceed 10 000 years.37 This means that this share of air pollutants contributes to a major disease burden in Portugal, and a significant share of this burden is likely to be cardiovascular.
Data of PM2.5 and PM10 in Portugal. The dashed lines represent the thresholds of European Union Ambient Air Quality Directives. Data from PM2.5 were retrieved from Brauer et al., World Bank data, and Brito et al.38–40 The PM10 data and data from Lisbon and Porto stations (average yearly data calculated from the available reported values) were retrieved from the Portuguese Environment Agency's website.41
Air pollution is a real threat to cardiovascular health and should not be underestimated by people, organizations and decision/policy makers involved in the prevention and treatment of CVDs. This topic was recently endorsed by the guidelines of European Society of Cardiology on CVD prevention, which recommend encouraging avoidance of long-term exposure to regions with high air pollution in patients with at least high cardiovascular risk (class of recommendation IIb and level of evidence C). This calls for the need for better monitoring and warning systems, to at least inform patients about the sites and periods of this high-risk exposure.
Cardiovascular disease opportunistic screening may be also considered in high air pollution regions (class of recommendation IIb and level of evidence C),42 particularly where high volume road traffic exists such as in Lisbon and Porto, as well as in regions with high indexes of air pollution due to industrial pollutants.43
Avoiding smoking and second-hand smoke (a neglected type of air pollution), reducing the use of motor vehicles whenever possible and exercising preferably at sites with lower air pollution, are the recommendations at individual-level related to air pollution. Other types of individual-level interventions still require further data before recommendations can be made.
The Portuguese Society of Cardiology advocates greater interdisciplinary involvement to improve knowledge of air quality exposure and cardiovascular diseases, including by strengthening environmental monitoring; it also advocates for a concerted effort to raise awareness and literacy on this issue in Portugal among all stakeholders, including healthcare providers and clinicians.
FundingNone.
Conflict of interestNone of the authors have conflict of interests regarding the topic of this article.