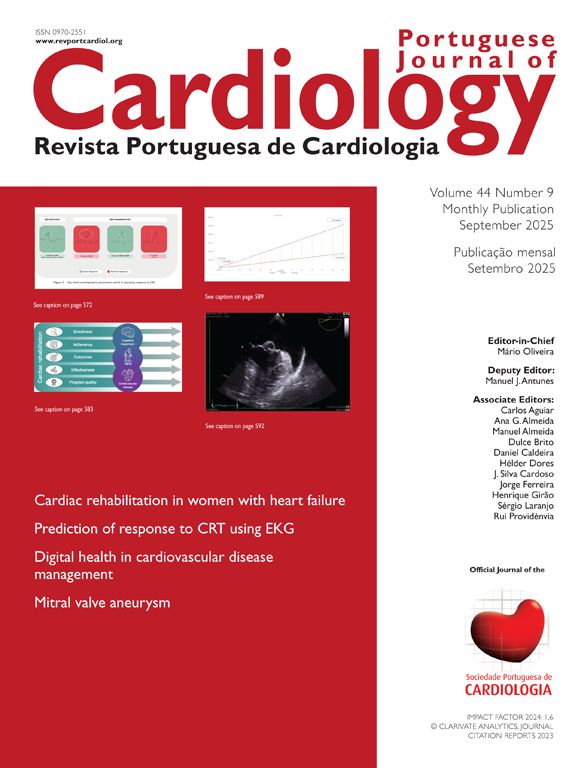
A 35-year-old man was sent to the Cardiology consult due to recurrent syncope after orthostatism preceded by prodromal symptoms. His syncopal response to orthostatism was so significant and so fast that he resorted to wheelchair ambulation. Additionally, the patient also reported episodes of syncope while lying down. Physical examination revealed the presence of an exuberant pectus excavatum. He was admitted to the Cardiology Department for evaluation. The initial cardiac study did not reveal significant findings: the 12-lead electrocardiogram presented an incomplete right bundle branch block, electrocardiographic monitoring showed rare supraventricular ectopy, and the transthoracic echocardiogram presented no relevant findings. A computed tomography scan was performed which showed severe pectus excavatum (Figure 1), with the lower sternum distancing 6 mm from the vertebral column, compressing the inferior vena cava (arrow). This resulted in a Haller index (a pectus index obtained from dividing the transverse diameter of the chest by the anterior–posterior diameter) of 46, far greater than the 3.25 cut-off to consider corrective surgery.1 A cardiac magnetic resonance imaging was then performed, revealing severe inferior vena cava compression in decubitus position (supplemental video).
The patient was referred for thoracic surgery and underwent a Nuss procedure, minimally invasive surgery to correct this thoracic deformity using intrathoracic bars.2 The patient did not experience any relevant complications from this, was syncope free during the follow-up and was able to walk once again. The chest radiograph and CT scan in follow-up revealed the excellent outcome of the surgery (Figure 2) with inferior vena cava decompression.
There are only a handful of published cases of pectus excavatum with inferior vena cava compression, with varying symptoms, such as syncopal episodes,3 lower extremity edema4 and pulsus paradoxus.5 To the best of our knowledge, we present the case with the most severe thoracic deformity causing disabling syncope in orthostatism, with a good functional outcome after surgical intervention.
Conflicts of interestThe authors have no conflicts of interest to declare.