International guidelines exclude athletes with implantable cardioverter-defibrillators (ICDs) from participating in sports, except those of low intensity (category IA, such as golf, billiards or bowling). However, these guidelines are based on expert consensus, and thus the safety and risks of participating in sports in this population are still largely unknown in the medical community.
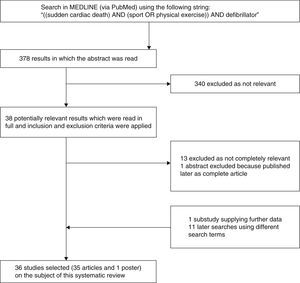
We performed a systematic review of the literature in PubMed using the following search string: “((sudden cardiac death) AND (sport OR physical exercise)) AND defibrillator”. After the application of pre-defined inclusion and exclusion criteria, 36 results were selected, which are explored in this paper.
Preliminary results on ICD use in this population appear to demonstrate the safety and efficacy of the device in this context. Further studies, with longer follow-up and with larger samples, may provide stronger evidence to support these findings. In the meantime, disqualifying almost all ICD patients from participating in sports, without taking into consideration their individual needs and characteristics, may be prejudicial to a considerable number of patients by preventing them from exercising their profession or engaging in recreational sport, for which their risk of sudden cardiac death may be low.
As recomendações internacionais excluem todos os atletas possuidores de um cardioversor desfibrilhador implantável (CDI) da prática de todos os desportos exceto os de baixa intensidade, inseridos na categoria IA (golfe, bilhar, bowling). No entanto, estas recomendações são baseadas em consensos de peritos e a segurança ou riscos resultantes da prática desportiva nesta população ainda são largamente desconhecidos da comunidade médica.
Foi realizada uma revisão sistemática da literatura existente na PubMed utilizando a seguinte expressão: «(sudden cardiac death) AND (sport OR physical exercise) AND defibrillator». Após a avaliação de critérios de inclusão e exclusão pré-definidos, foram selecionados 36 resultados que são explorados neste manuscrito.
Aesultados preliminares da utilização de CDI nesta população parecem atestar a sua segurança e eficácia. Estudos futuros, permitindo o seguimento de um maior número de desportistas por um período mais duradouro, poderão fornecer mais robustez e evidência mais forte a suportar estes achados. Entretanto, a abordagem ao desportista portador de CDI deve ser personalizada e adequada ao paciente, de acordo com a cardiopatia e tipo de desporto em questão. Uma abordagem generalista com desqualificação de quase todos os desportistas sem atender às suas especificidades pode prejudicar uma quantidade considerável de doentes aos quais será vedada a possibilidade de manter a sua profissão ou prática, para a qual poderiam eventualmente apresentar um risco baixo de morte súbita cardíaca.
arrhythmogenic right ventricular dysplasia
36th Bethesda Conference
dilated cardiomyopathy
European Society of Cardiology
implantable cardioverter-defibrillator
hypertrophic cardiomyopathy
sudden cardiac death
American College of Cardiology/American Heart Association
Sudden cardiac death (SCD) in athletes, its prevention by means of implantable cardioverter-defibrillators (ICDs), and whether athletes with ICDs should be disqualified from participating in competitive sport, are currently the subject of intense controversy.1
The recommendations of the 36th Bethesda Conference (BC#36)2 and the European Society of Cardiology (ESC)25 exclude athletes with ICDs from all but low-intensity sports (category IA of the BC#36 classification2) (Table 1). These recommendations are based on the perceived risks, including failure of the device to deliver appropriate therapies, injury resulting from loss of consciousness or control caused by an ICD shock or the arrhythmia itself, and damage to the device or leads.3 The guidelines were developed on the basis of expert consensus rather than on the results of studies, and there is as yet no solid evidence concerning the actual risks to ICD patients arising from participation in competitive sports.
Classification of sports (adapted from Maron et al.2).
Implantation of ICDs has grown exponentially in recent decades, often in individuals with normal myocardial function but with genetic mutations that could lead to fatal arrhythmias.4 The result is an increasing number of young individuals with ICDs, many of whom are athletes and, according to the guidelines, should be disqualified from participating in competitive sports.2,25 The problem is even more serious for professional athletes who are thereby prevented from exercising their profession and suffer the inevitable consequences.
Despite the existence of the guidelines, according to a 2006 survey, many clinicians do not follow them and opt to make their decisions based on the individual athlete, medical condition and sport concerned.5 In recent years, the subject has been explored by some centers; their findings may support evidence-based decision-making and lead to changes in the management of these patients.
The aim of the present study is to systematically review the state of the art in this area.
MethodsThe review was based on information in articles indexed in MEDLINE (via PubMed) using the following search string: “((sudden cardiac death) AND (sport OR physical exercise)) AND defibrillator”. Filters were defined to restrict searches to articles in English, Portuguese or Spanish, with available abstracts, published between 1985 and 2014.
Articles were selected on the basis of their abstract, which was used to assess their relevance and whether they were likely to meet the inclusion and exclusion criteria defined below. The full text of each relevant article was read to determine whether it was to be included. The inclusion criteria were: (1) research on individuals with ICDs who participate in sports, whether (a) only athletes with ICDs, (b) athletes and non-athletes with ICDs, or (c) athletes with and without ICDs; (2) registries characterizing epidemiological aspects of SCD in athletes; (3) consensus documents and international guidelines on the subject. Letters to the Editor, case reports, and review articles that did not provide new observational data were excluded.
Additional searches were performed with alternative search strings in different search engines, including Sci-Hub and B-on, and the reference lists of the selected articles were consulted to identify other potentially relevant material, which was analyzed using the same inclusion and exclusion criteria.
ResultsThe search string produced a total of 378 results, of which 340 were excluded after a reading of the abstract indicated they were not relevant to the current review. The remaining 38 manuscripts, together with others identified from other sources, were analyzed using the same inclusion and exclusion criteria and a total of 36 were selected for the review: 35 articles3–30,32–36 and a poster presented at a congress.31 The selection process is shown in Figure 1.
Definition and epidemiology of sudden cardiac deathSCD, mainly caused by malignant ventricular arrhythmias,6 is one of the leading causes (>50%) of cardiovascular death worldwide. It is defined as unexpected natural death from a cardiac cause within a short time period, generally ≤1 hour from the onset of symptoms, in a person without any prior condition that would appear fatal.7 Although rare in the young, participation in competitive sports increases the risk of SCD7; the annual incidence of SCD in athletes aged <35 years is reported as 1:100000–300000,8 although recent studies have suggested that this is an underestimate and that 1:50000 is more realistic.9 It is more common in males.10
Causes of sudden cardiac deathThe fatal event is usually caused by rhythm disturbances, particularly tachyarrhythmias such as ventricular fibrillation. The arrhythmia may have various causes (ischemia, primary arrhythmia, rapid atrioventricular conduction), but the common denominator is electrical instability7 (Table 2).
Causes of sudden death in 387 young athletes (adapted from Maron et al.11).
| Cause | No. of athletes | % |
|---|---|---|
| HCM | 102 | 26.4 |
| Commotio cordis | 77 | 19.9 |
| Coronary artery anomalies | 53 | 13.7 |
| LVH of indeterminate causation | 29 | 7.5 |
| Myocarditis | 20 | 5.2 |
| Ruptured aortic aneurysm | 12 | 3.1 |
| ARVD | 11 | 2.8 |
| Myocardial bridging | 11 | 2.8 |
| Aortic valve stenosis | 10 | 2.6 |
| Atherosclerotic coronary artery disease | 10 | 2.6 |
| Dilated cardiomyopathy | 9 | 2.3 |
| Myxomatous mitral valve degeneration | 9 | 2.3 |
| Asthma (or other pulmonary condition) | 8 | 2.1 |
| Heat stroke | 6 | 1.6 |
| Drug abuse | 4 | 1.0 |
| Other cardiovascular cause | 4 | 1.0 |
| Long QT syndrome | 3 | 0.8 |
| Cardiac sarcoidosis | 3 | 0.8 |
| Trauma involving structural cardiac injury | 3 | 0.8 |
| Ruptured cerebral artery | 3 | 0.8 |
ARVD: arrhythmogenic right ventricular dysplasia; HCM: hypertrophic cardiomyopathy; LVH: left ventricular hypertrophy.
The most common cause of SCD in young athletes is hypertrophic cardiomyopathy (HCM),11 although in a study in the region of Veneto, Italy, the leading cause was arrhythmogenic right ventricular dysplasia (ARVD).12 This may be explained by regional differences between Europe and the USA and by the different screening methods used in Italy, where all competitive athletes aged under 35 undergo testing consisting of a thorough clinical and family history, physical examination and 12-lead ECG. Such screening is more likely to detect HCM (in which over 95% of cases present a pathological ECG) than ARVD, most cases of which are only diagnosed on autopsy and which contribute significantly to mortality in young athletes.14 In athletes aged over 35, the leading cause of SCD is atherosclerotic coronary disease.3
Definition of sports and of athletesAccording to the BC#36, a competitive athlete is defined as one who participates in a team or individual sport, competes regularly, and undergoes systematic training (usually intense) to achieve excellence.2 A sport is an organized, competitive, entertaining, and skillful activity requiring commitment, strategy, and fair play, in which a winner can be defined by objective means. It is governed by a set of rules or customs.15 This definition does not include recreational or leisure activities, since they are not competitive,15 and according to the BC#36 and ESC guidelines, sport is considered more demanding than other recreational activities, placing the individual at higher risk of a fatal arrhythmia. However, it should be borne in mind that some competitive sports may incur less risk than certain leisure activities; for example, competitive shooting is less likely to lead to SCD than amateur weightlifting.2 The BC#36 recommendations accordingly classify sports by the intensity of their static and dynamic components (low, moderate or high) (Table 1). On this basis, weightlifting has a large static component and running has a large dynamic component.16
Use of implantable cardioverter-defibrillators in athletesThe sooner defibrillation is performed, the more effectively ventricular fibrillation can be terminated. If the shock is delivered within 30 s, there is a 90% probability that it will be successful, but this falls by 7%–10% for every minute that passes, and if defibrillation is begun 10 min after the event the likelihood of resuscitation is only 10%.17,18
The location of an ICD means that it can interpret the cardiac rhythm and apply a shock almost immediately, which leads to success rates of 95%–99%. As a result, in the last 20 years ICDs have become the gold standard treatment for ventricular arrhythmias.4
The indications for ICD implantation in athletes in the ESC6,20 and American College of Cardiology/American Heart Association (ACC/AHA)6 guidelines are similar to those for the general population. The main complications are lead dislodgment or fracture, inappropriate shocks, and generator migration or pocket erosion.3
The number of individuals with ICDs for primary prevention has risen sharply in recent years, due to more widespread screening of families with a history of inherited arrhythmia syndromes, channelopathies and cardiomyopathies, as well as improved identification of silent mutation carriers. As a consequence, there are increasing numbers of apparently healthy and highly active individuals who, due to their increased risk of suffering an arrhythmic event (or to prevent recurrence), have an ICD to prevent SCD, which can be the first manifestation of disease.
Specific risks associated with implantable cardioverter-defibrillators in athletesThere are various considerations specific to athletes that can affect the safety and efficacy of ICDs in this population and thus influence the decision whether they can resume their sporting activity after implantation (Table 3).3 A major concern is that the ICD may not reliably defibrillate under athletic conditions, because of physiological alterations such as increased circulating catecholamine levels, leading to dehydration, acidosis, electrolyte disturbances and volume depletion, which in turn make the occurrence and perpetuation of arrhythmias more likely.22 There is little evidence on the efficacy of ICD shocks under the metabolic conditions of intense exercise.21
Factors affecting the use of implantable cardioverter-defibrillators in athletes (adapted from Lawless et al.3).
| Increased exercise-induced ventricular arrhythmias |
| Fear of ICD failure to defibrillate under athletic conditions |
| Worsening of ARVD and DCM |
| Increased inappropriate shocks due to sinus or supraventricular tachycardia or atrial fibrillation |
| Injury due to momentary loss of consciousness and/or control due to arrhythmia or ICD shock |
| Damage to ICD mechanism: |
| 1. Lead fracture |
| 2. Generator migration or pocket erosion |
| 3. Traumatic damage to or destruction of generator or reset |
| Lack of evidence of ICD effectiveness under conditions of intense exercise |
ARVD: arrhythmogenic right ventricular dysplasia; DCM: dilated cardiomyopathy; ICD: implantable cardioverter-defibrillator.
Furthermore, strenuous exercise worsens certain conditions such as ARVD and dilated cardiomyopathy.23,24
Another potential problem is that inappropriate shocks may be more frequent during exercise, due to sinus or supraventricular tachycardia or atrial fibrillation. Moreover, an athlete (and, in the case of motor sports, spectators) may be injured as a result of transient loss of consciousness and/or control due to arrhythmia or ICD shock. In addition, the ICD or leads may be damaged, particularly due to repeated energetic arm movements, as found in sports such as golf and boxing, or to direct impacts on the ICD itself or the subclavian region (“subclavian crush”), as may occur in any contact sport.3 Finally, those who argue that athletes with ICDs should be excluded from competition point out that inappropriate shocks can have a negative psychological effect on these individuals.
In light of the above, current guidelines recommend that athletes with ICDs should be disqualified from all competitive sports except those with low static and dynamic components, such as golf, billiards or bowling (category IA of the BC#36 classification) (Table 1).
New studies and controversyTable 4 summarizes the main results of studies assessing the use of ICDs in athletes.
Main studies assessing the use of implantable cardioverter-defibrillators in athletes.
| Study | Population | Main findings and conclusions | Limitations |
|---|---|---|---|
| Lampert et al.5 | 614 physicians involved in assessing athletes | - Only 10% followed the guidelines strictly- More than two-thirds based restrictions on patients’ underlying heart disease- Many patients with ICDs continue to participate in vigorous and even competitive sports | - A survey, not a prospective study- Participants were self-selected- Responses may not reflect the opinions of all physician members of the Heart Rhythm Society- Recollection of events may have been selective- Factors potentially predisposing to shocks were not determined |
| Lampert et al.26 | 372 athletes with ICDs, 137 highly competitive | Many athletes with ICDs can engage in vigorous competitive sports without increased risk of arrhythmia or of damage to the ICD system | - Study participants were self-selected- Most subjects had excellent ejection fractions- Not all shocks were reported immediately, some only at six-monthly follow-up |
| Saarel et al.31 | 21 competitive athletes with ICDs | Sports-related complications (n=0, 0%), appropriate shocks (n=7, 33%) and inappropriate shocks (n=1, 5%) were rare- Patients chose to continue to participate because it appeared to be safe to do so | - Small sample |
ICD: implantable cardioverter-defibrillator.
A 2006 survey5 of physician members of the Heart Rhythm Society designed to assess the decisions being made regarding sports participation in patients with ICDs painted a very different picture from that to be expected from the guidelines: of the 614 physicians who responded, only 62 (10%) followed the BC#36 and ESC guidelines strictly by excluding patients from all sports except those in category IA, while most (n=464; 76%) only recommended avoidance of contact, 273 (45%) recommended avoidance of competitive sports, and 71% reported caring for patients who participated in sports, including vigorous, competitive sports. More than two-thirds based restrictions on patients’ underlying heart disease and not solely on the guidelines. It is worth noting that 40% of responders had over 10 years’ experience with ICD patients. Although a high proportion of patients participated in sports, and shocks were common, adverse events were rare. Most complications were due to device failure such as lead fracture or migration attributed to repetitive arm movements (n=28), most commonly weightlifting (n=16), tennis (n=2) and golf (n=5). Interestingly, the latter is classified as IA and thus not excluded by the guidelines. While there was agreement that heart failure and ischemic heart disease should limit sports participation, physicians disagree concerning long QT syndrome and Brugada syndrome.5
In view of the observation that despite the guidelines, ICD patients continue to take part in competitive sports, Lampert et al. established a multicenter international registry.26 Participants were recruited via mailings to physicians and by direct communication with patients via patient group Internet sites and mailing lists. Data were collected through telephone contact every six months and medical records were obtained from 41 sites in North America and 18 in Europe. Patients were queried about shocks received, sequelae, preshock activity and any change in sports participation, health or ICD status. Of the 372 participants, 328 were participating in organized sports and 44 were participating in high-risk sports. Median age was 33 years and 33% were female. The most frequent diagnoses were long QT syndrome (n=73), HCM (n=63), and ARVD (n=55); the most common sports were running (n=106), soccer (n=69) and basketball (n=56), while the most common high-risk sport was skiing.
During a median follow-up of 31 months, there were no tachyarrhythmic deaths, resuscitated cardiac arrests, or injuries related to arrhythmias or shocks during sports participation. There were 49 shocks in 37 participants (10% of the study population) during competition/practice, 39 shocks in 29 participants (8%) during other physical activity, and 33 shocks in 24 participants (6%) at rest. More individuals received shocks during either competition/practice or physical activity than during rest (16% vs. 6%; p<0.0001), but there was no significant difference between the proportion receiving a shock during competition/practice and those receiving a shock during other physical activity (10% vs. 8%; p=0.34). Similarly, the proportion receiving appropriate shocks during either competition/practice or other physical activity was greater than the proportion receiving appropriate shocks during rest (8% vs. 3%; p=0.006), but there was no difference between competition/practice and other physical activity (6% vs. 4%; p=0.18). Of a subgroup of 60 highly competitive athletes, all ≤21 years of age, 17 (28%) experienced a total of 25 shocks. In this subgroup there was no significant difference between the number of shocks in this subgroup during competition/practice (1%) and at rest (4%).
There were no reported ICD malfunctions in 97% of the participants at five years and in 90% at 10 years. Most (70%) of athletes who received shocks during sports chose to continue playing.
These findings suggest that many athletes can safely participate in various contact or high-intensity sports without risk of injury, device damage, or ineffective defibrillation. Shock rates in the study population were generally similar to those in ICD patients who do not play sports or are less active.27,28 The rate of lead failure or fracture was also similar to five-year rates seen in other populations (85%–98%).29
Disqualifying athletes with ICDs from sports can significantly affect their quality of life,30 particularly younger individuals, who describe feelings of exclusion and being considered ‘not normal’ as the main problem with having an ICD. The fact that most athletes in the study continued to play even after receiving shocks suggests that the benefits of sport outweigh the negative impact that shocks may have.
Following publication of the above studies, other researchers have set out to investigate further. Saarel et al.31 recently presented preliminary results of a registry of 21 young patients with ICDs who choose to play competitive or dangerous sports greater than IA in both static and dynamic components. Ten had congenital heart disease, six had inherited arrhythmia syndromes and five had cardiomyopathy. Mean follow-up was five years; the most common sports were basketball and baseball. There were no cardiac deaths and no increase in morbidity after four years. One participant received two appropriate shocks for supraventricular tachycardia during a basketball game and subsequently retired from competitive sports; no other participant suffered more frequent shocks, appropriate or inappropriate, during sports, and no increase in device malfunction was reported. All participants were under beta-blocker therapy to prevent inappropriate shocks due to sinus or ventricular tachycardia.
DiscussionRecent studies5,26,31 appear to show that participation in sports by ICD patients is not as harmful as previously thought.
The decision whether to disqualify athletes with ICDs should be taken on an individual basis. In recent years, there has been a growing trend in medicine towards patient-centered decision-making, in which patients’ motivations and preferences are taken more into account, increasing their empowerment and role in decisions.32 However, it is important to avoid the opposite extreme, in which the physician acts merely as a provider of information and the patient is given complete autonomy to take decisions, irrespective of the physician's opinion.33,34 The guidelines are still based largely on input from cardiologists as the main decision-makers, and the question of the degree of empowerment that athletes with ICDs do or should have with regard to disqualification or retirement from sports is still an open one. These patients require counseling, taking the time to provide them with careful and clear explanations of the known risks of participation in sports, and the benefits and risks of ICDs, as well as aspects for which there is insufficient evidence, and to answer any questions they may have, in order to give them a greater sense of control and to enable joint and informed decisions.
There is consensus among physicians that heart failure, HCM and ischemic heart disease should limit participation in sports, but this is not the case with long QT syndrome and Brugada syndrome.3 In HCM, different sports, such as football or boxing, can be associated with different levels of risk. In certain cases the decision is not likely to be difficult, such as in left ventricular dysfunction with exercise-induced arrhythmia, but in ICD patients without left ventricular dysfunction other factors need to be taken into consideration.35
Although ICD shocks can have a negative impact on quality of life, exclusion from playing sports can have a similar or even worse effect. Physical activity considerably reduces cardiovascular morbidity and mortality through a variety of mechanisms.37 It should be stressed that in many cases the athlete will be forced to abandon their professional or recreational sports activity, which can have severe personal repercussions.30
LimitationsThis review has certain limitations. Firstly, there are few studies assessing the use of ICDs in athletes. Secondly, follow-up times for athletes with ICDs are short and there are no data on long-term efficacy and safety in this population. Thirdly, the use of automated external defibrillators was not examined, since there is extensive evidence and consensus in the medical community on this subject. Finally, most of the results relate to devices with intravascular leads; data on subcutaneous ICDs are still scarce.
ConclusionsManagement of athletes with ICDs should be individualized to the patient, according to the heart disease and sport in question. Disqualifying almost all ICD patients from participating in sports, without taking into consideration their individual needs and characteristics, may be prejudicial to a considerable number of patients by preventing them from exercising their profession or engaging in recreational sport, for which their risk of sudden cardiac death may be low.
The BC#36 guidelines are now 10 years old and based solely on expert consensus and the evidence available at the time. Recent studies may lead to a revision of the guidelines; however, there is still little evidence and further studies will be needed to provide solid data and clear answers to the many questions in this area.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Liz Almeida R, Providência R, Gonçalves L. Utilização de cardioversores desfibrilhadores implantáveis em desportistas: revisão sistemática. Rev Port Cardiol. 2015;34:411–419.