The aim of the present paper was to report trends in coronary angioplasty for the treatment of ST-elevation myocardial infarction (STEMI) in Portugal.
MethodsProspective multicenter data from the Portuguese National Registry of Interventional Cardiology (RNCI) and official data from the Directorate-General for Health (DGS) were studied to analyze percutaneous coronary intervention (PCI) procedures for STEMI from 2002 to 2013.
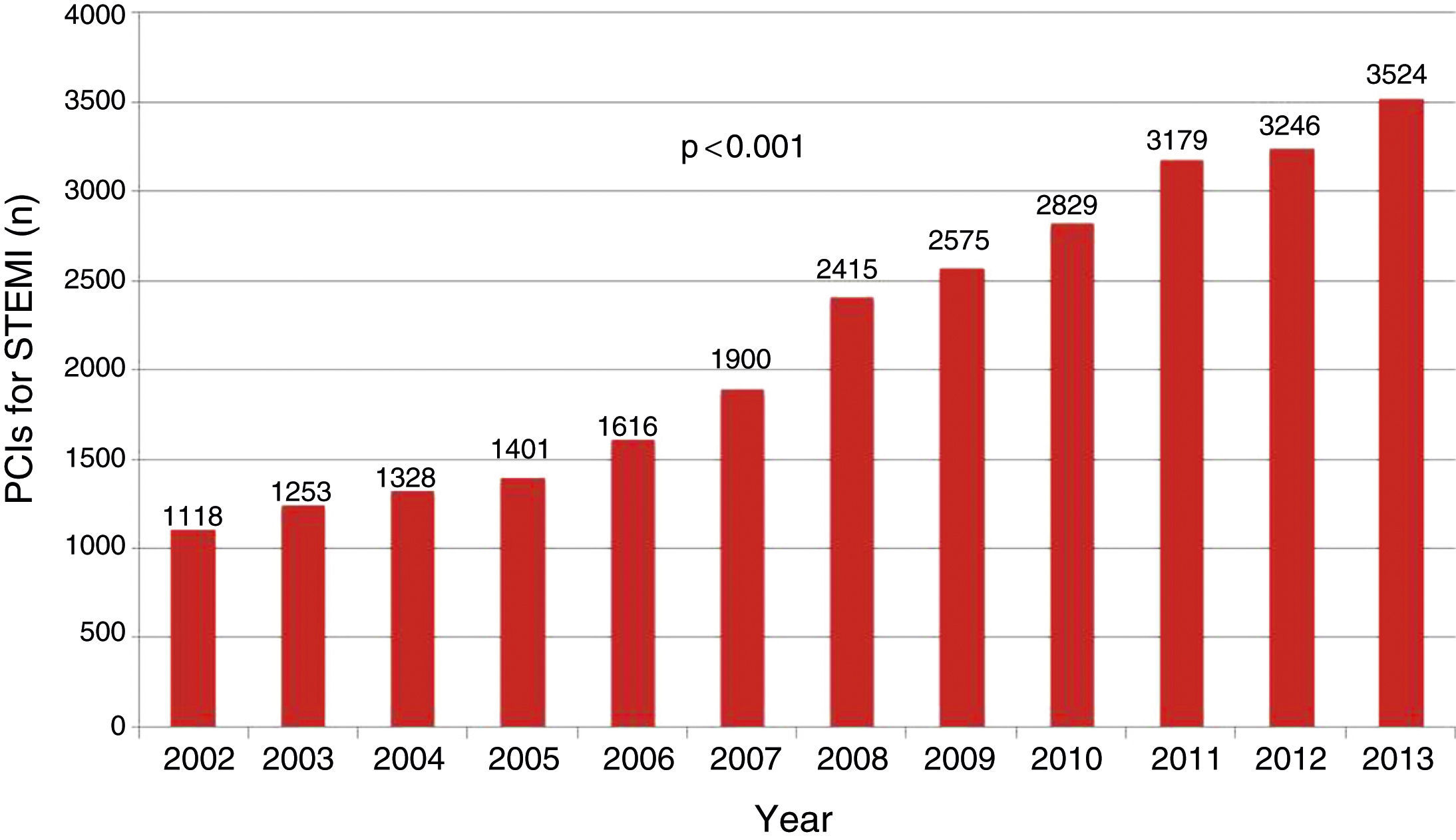
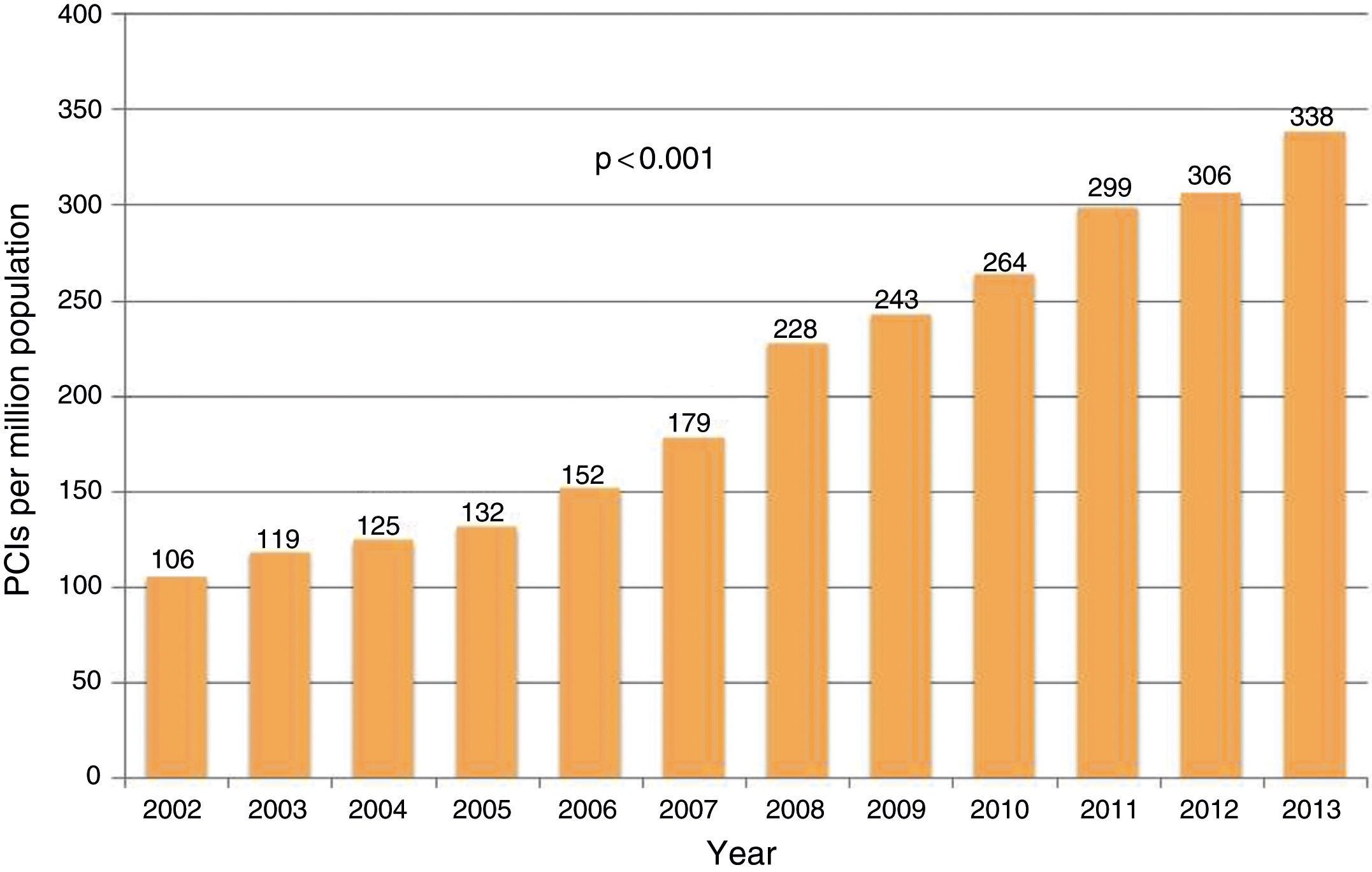
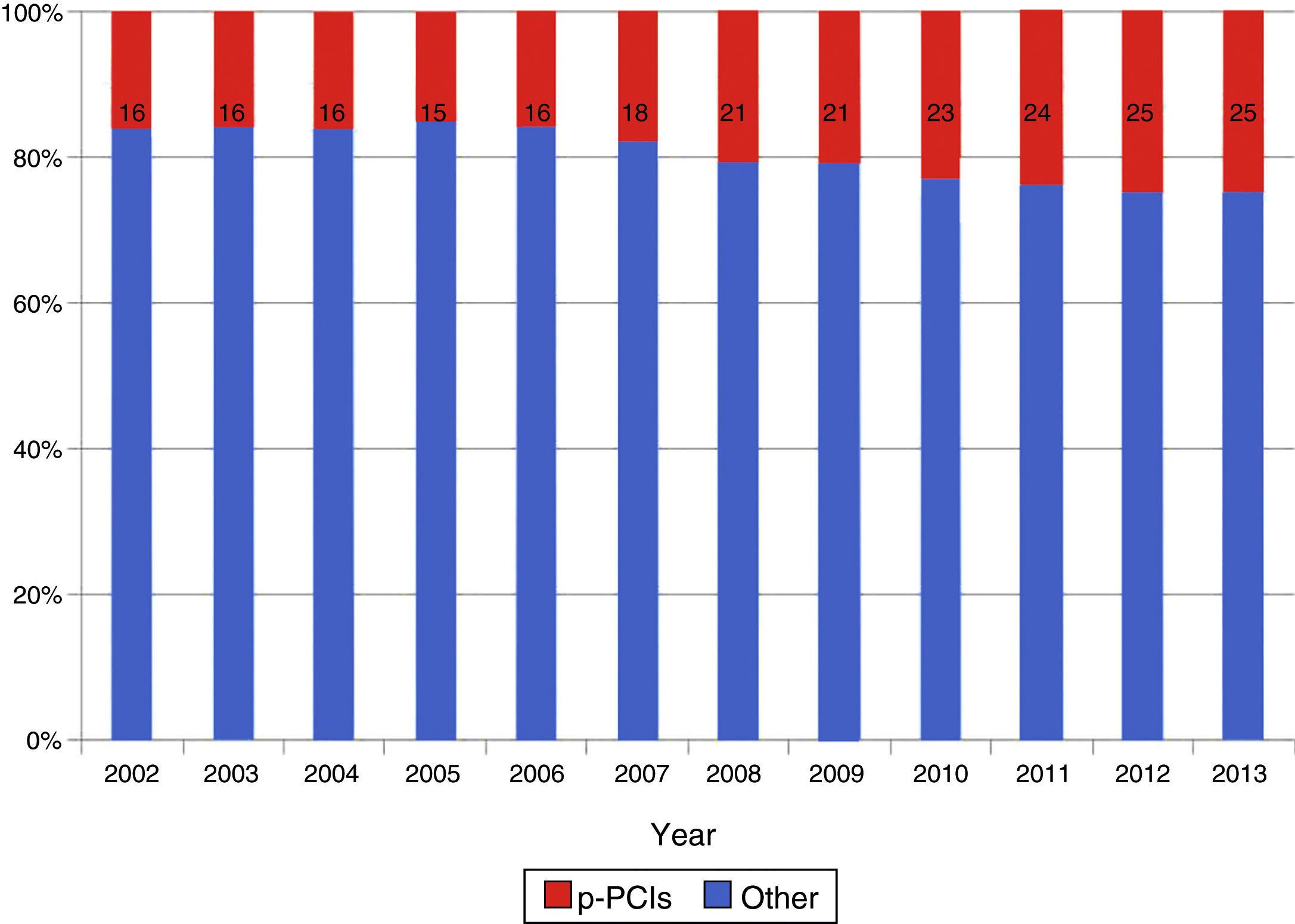
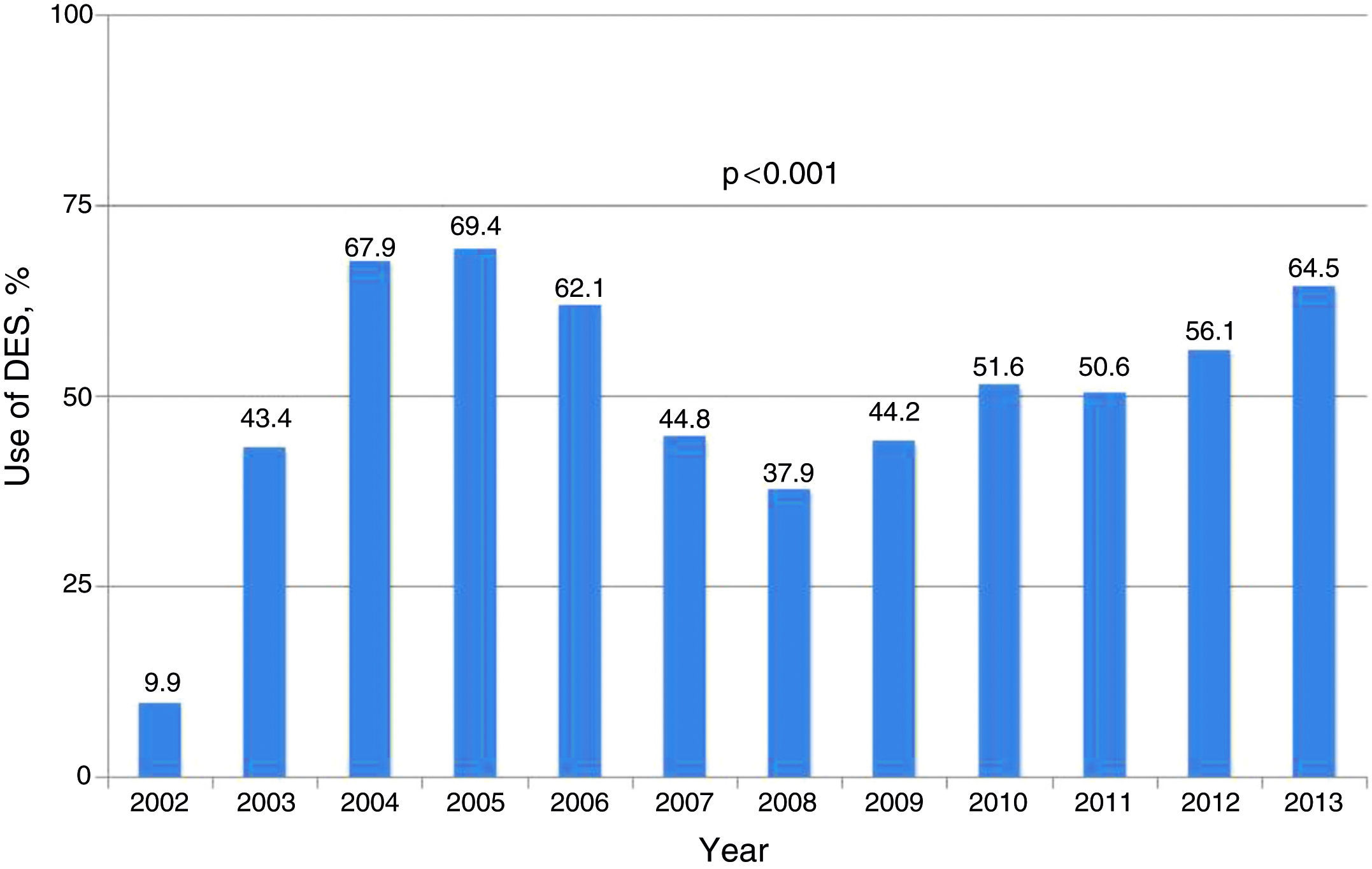
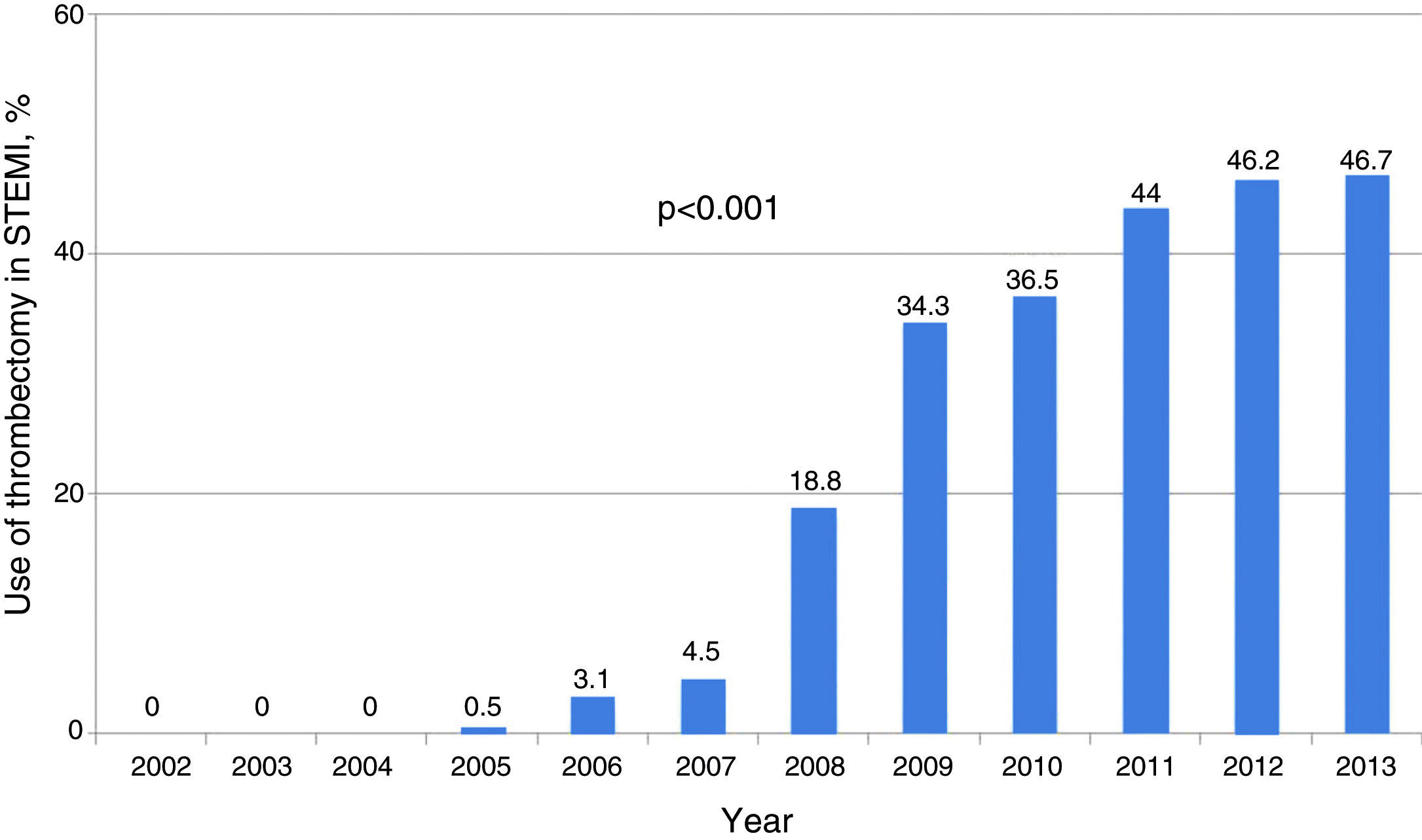
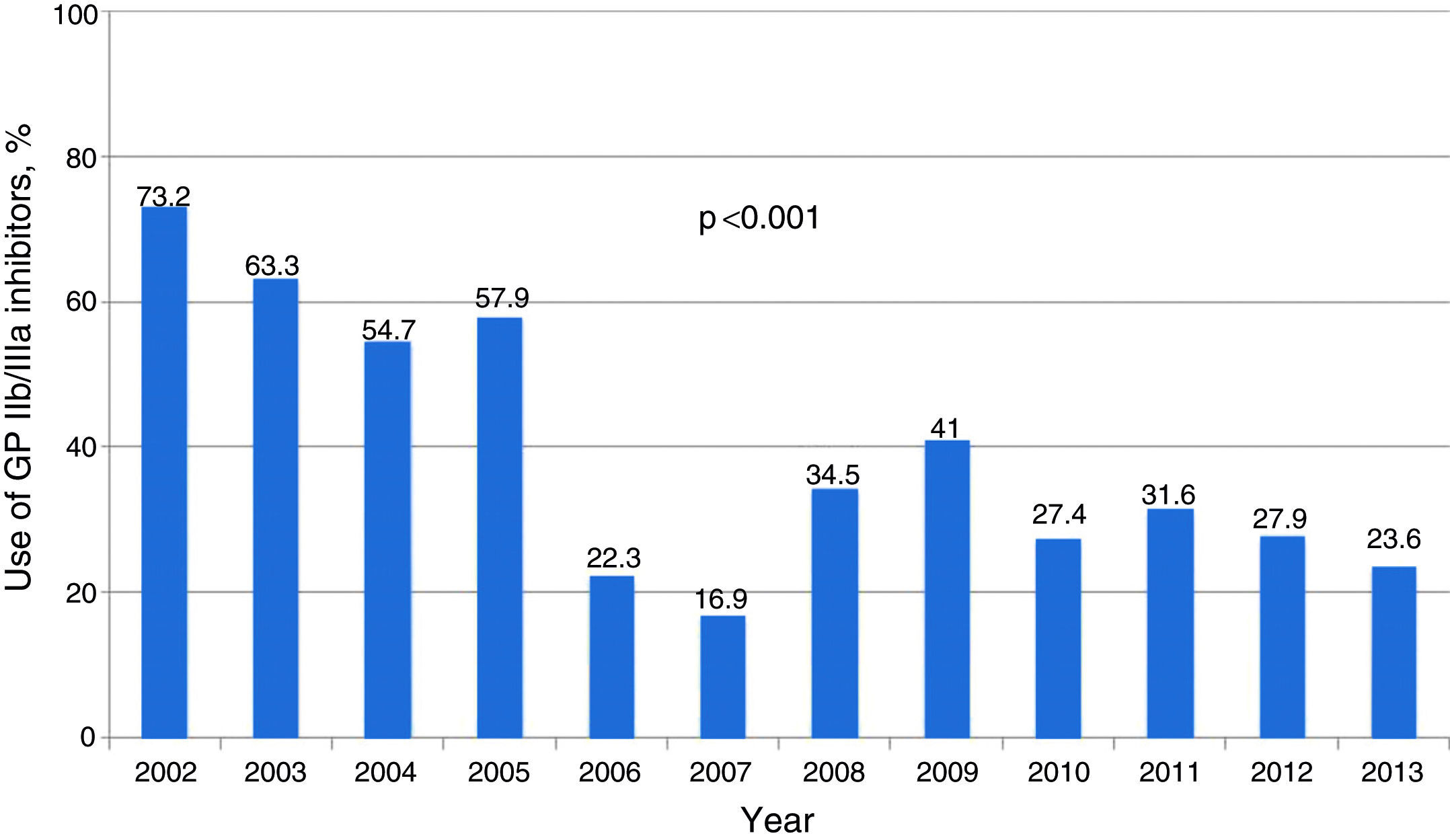
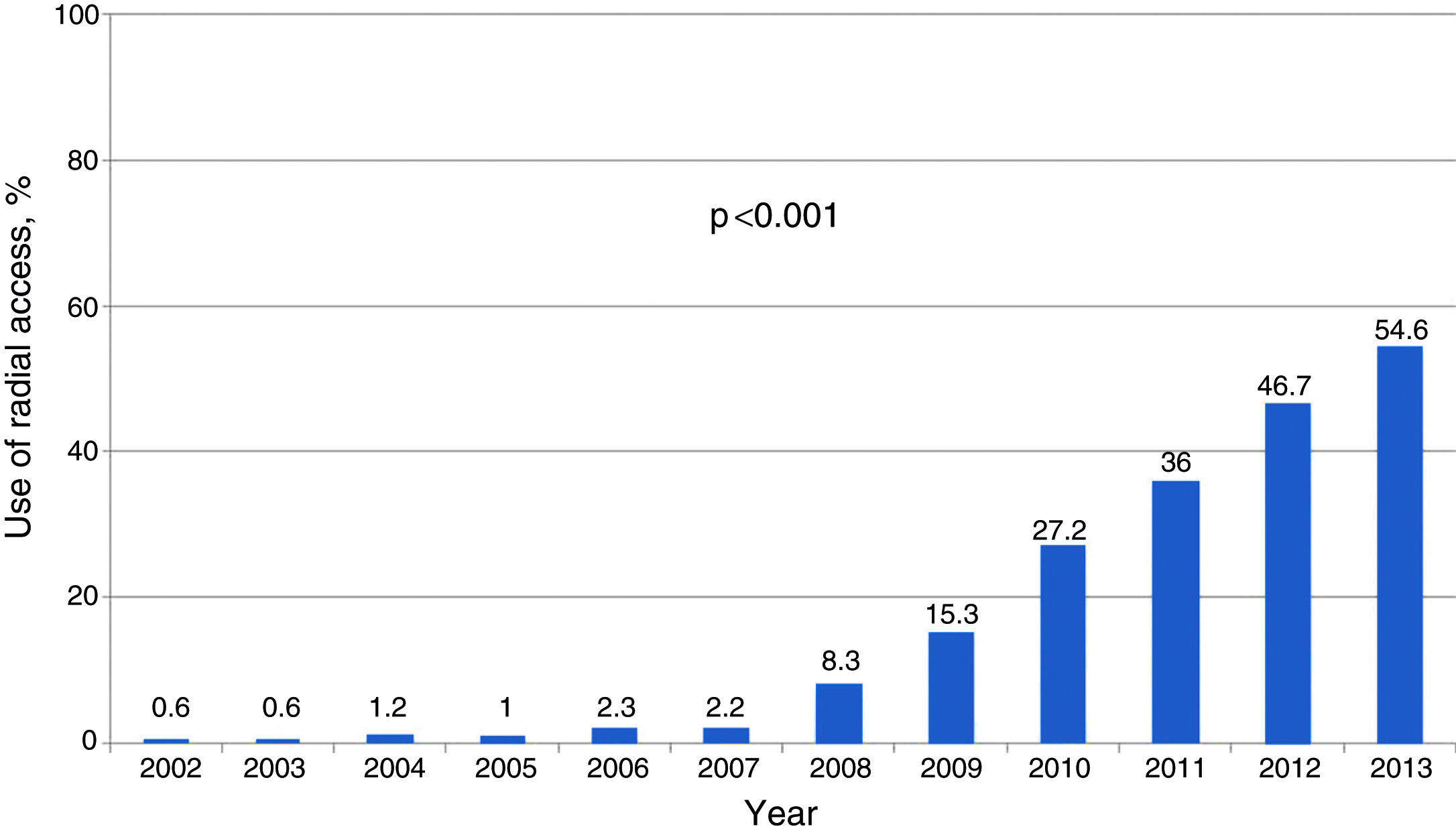
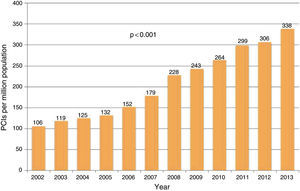
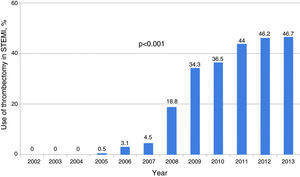
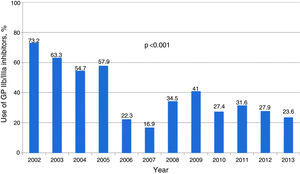
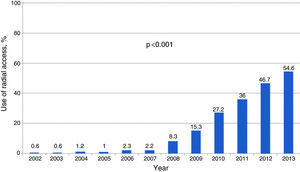
ResultsIn 2013, 3524 primary percutaneous coronary intervention (p-PCI) procedures were performed (25% of all procedures), an increase of 315% in comparison to 2002 (16% of all interventions). Between 2002 and 2013 the rate increased from 106 to 338 p-PCIs per million population per year. Rescue angioplasty decreased from 70.7% in 2002 to 2% in 2013. During this period, the use of drug-eluting stents grew from 9.9% to 69.5%. After 2008, the use of aspiration thrombectomy increased, reaching 46.7% in 2013. Glycoprotein IIb-IIIa inhibitor use decreased from 73.2% in 2002 to 23.6% in the last year of the study. Use of a radial approach increased steadily from 8.3% in 2008 to 54.6% in 2013.
ConclusionDuring the reporting period there was a three-fold increase in primary angioplasty rates per million population. Rescue angioplasty has been overtaken by p-PCI as the predominant procedure since 2006. New trends in the treatment of STEMI were observed, notably the use of drug-eluting stents and radial access as the predominant approach.
Foi nosso objetivo reportar a evolução da angioplastia coronária no tratamento do enfarte agudo do miocárdio com supradesnivelamento do segmento ST (ICP-P), entre 2002-2013.
MétodosOs dados prospetivos multicêntricos do Registo Nacional de Cardiologia de Intervenção (RNCI) e os dados oficiais da Direção Geral de Saúde (DGS) foram conjugados para estudar as ICP-P realizadas entre 2002-2013.
ResultadosEm 2013 realizaram-se 3524 angioplastias primárias (ICP-P), representando um crescimento de 315% relativamente ao ano de 2002. Em 2002 a ICP-P representava 16% do total de angioplastias coronárias, passando a representar 25% nos anos de 2012-2013. Entre 2002-2013 o número de procedimentos por milhão de habitantes aumentou de 106 para 338 e a angioplastia de recurso decresceu de 70,7 para 2%. Durante o período em análise, a utilização de stents eluidores de fármaco cresceu de 9,9 para 69,5%. Após 2008, observou-se uma utilização crescente da trombectomia de aspiração, atingindo 46,7% em 2013. Os inibidores das glicoproteínas IIb/IIIa registaram um decréscimo no seu uso, sendo de 73,2% em 2002 e de 23,6% em 2013. O acesso radial cresceu de 8,3% em 2008 até 54,6% em 2013.
ConclusõesDurante o período em análise, a taxa de angioplastia coronária por milhão de habitantes triplicou. A angioplastia de recurso foi ultrapassada pela angioplastia primária a partir de 2006. Observaram-se novas tendências no tratamento do enfarte agudo do miocárdio com supradesnivelamento do segmento ST, salientando-se a utilização de stents eluidores de fármacos e o acesso radial.
Primary percutaneous coronary intervention (p-PCI), when performed in a timely fashion and by experienced teams, is the best treatment option for ST-elevation myocardial infarction (STEMI).1 The aim of the present paper was to report trends in coronary angioplasty for the treatment of STEMI in Portugal, based on data from the Portuguese National Registry of Interventional Cardiology (RNCI) of the Portuguese Society of Cardiology (SPC) and official data on interventional cardiology from the Directorate-General for Health (DGS).2
The RNCI, established by the SPC in 2002, is centralized in the National Center for Data Collection in Cardiology (CNCDC), under the aegis of the Portuguese Association of Cardiovascular Intervention (APIC) of the SPC. The aim of this multicenter, voluntary, prospective patient registry is to provide a continuous record of percutaneous procedures and patient characteristics in Portugal,3 based on the Cardiology Audit and Registration Data Standards (CARDS).4
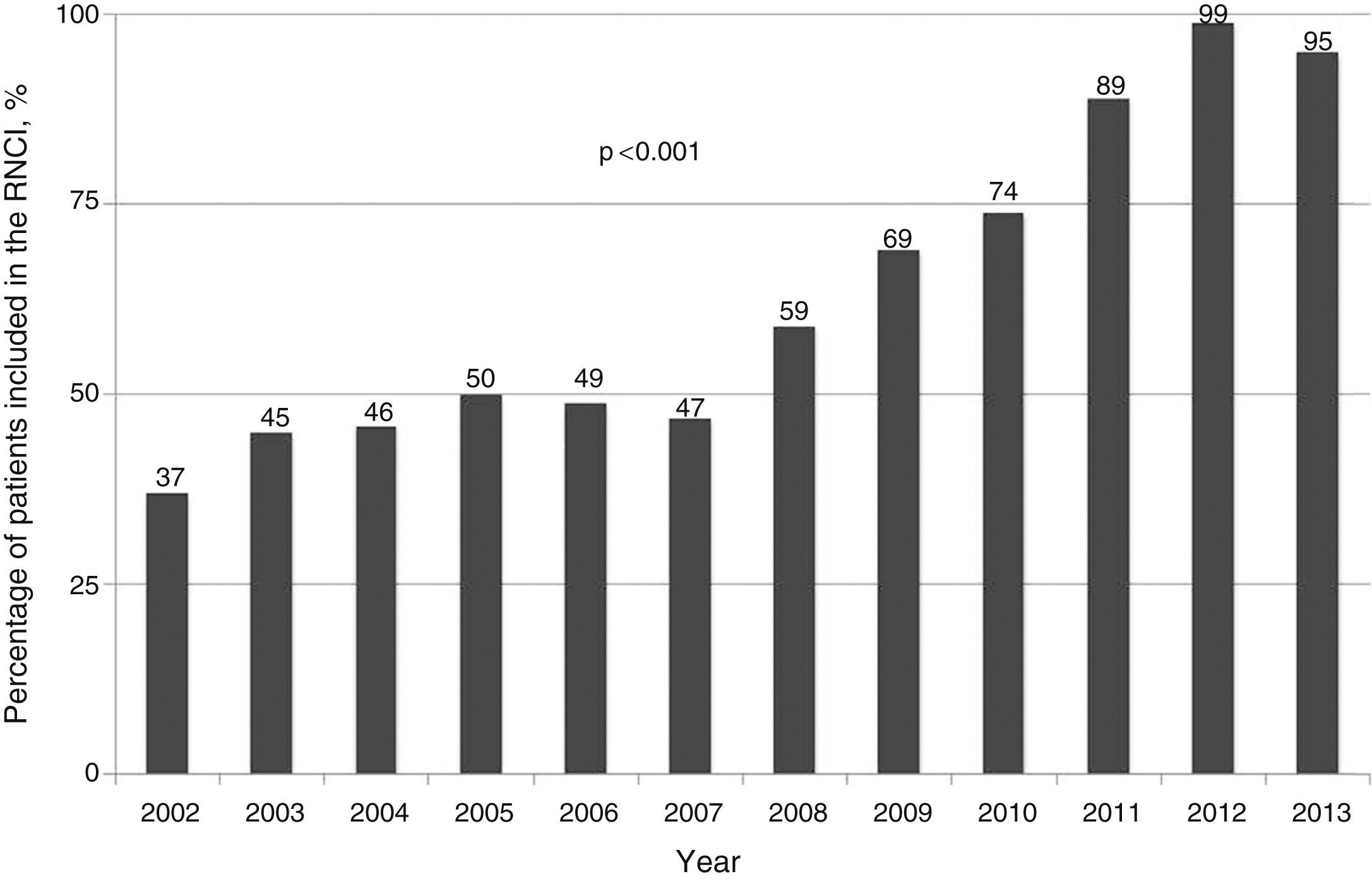
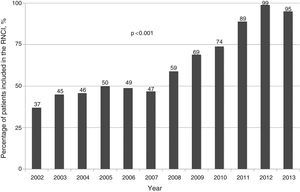
MethodsThe percentage of patients included in the RNCI has progressively increased. In the first year of the registry (2002), the sample represented only 37% of all interventions in that year, while the proportion reached 99% in 2012 and 95% in 2013 (Figure 1).
The RNCI data were complemented by official figures published by the DGS, collected by annual surveys of interventional cardiology centers, regarding the total number of coronary angioplasties and p-PCIs and use of fibrinolysis. The other data presented, expressed as numbers and percentages, are based on the RNCI.
Statistical analysisBaseline characteristics were compared between years by the Kruskal-Wallis test for continuous variables, expressed as means ± standard deviation, and by the chi-square test for categorical variables, expressed as relative and absolute frequencies.
SPSS version 19 was used for the statistical analysis. A value of p<0.05 was considered significant.
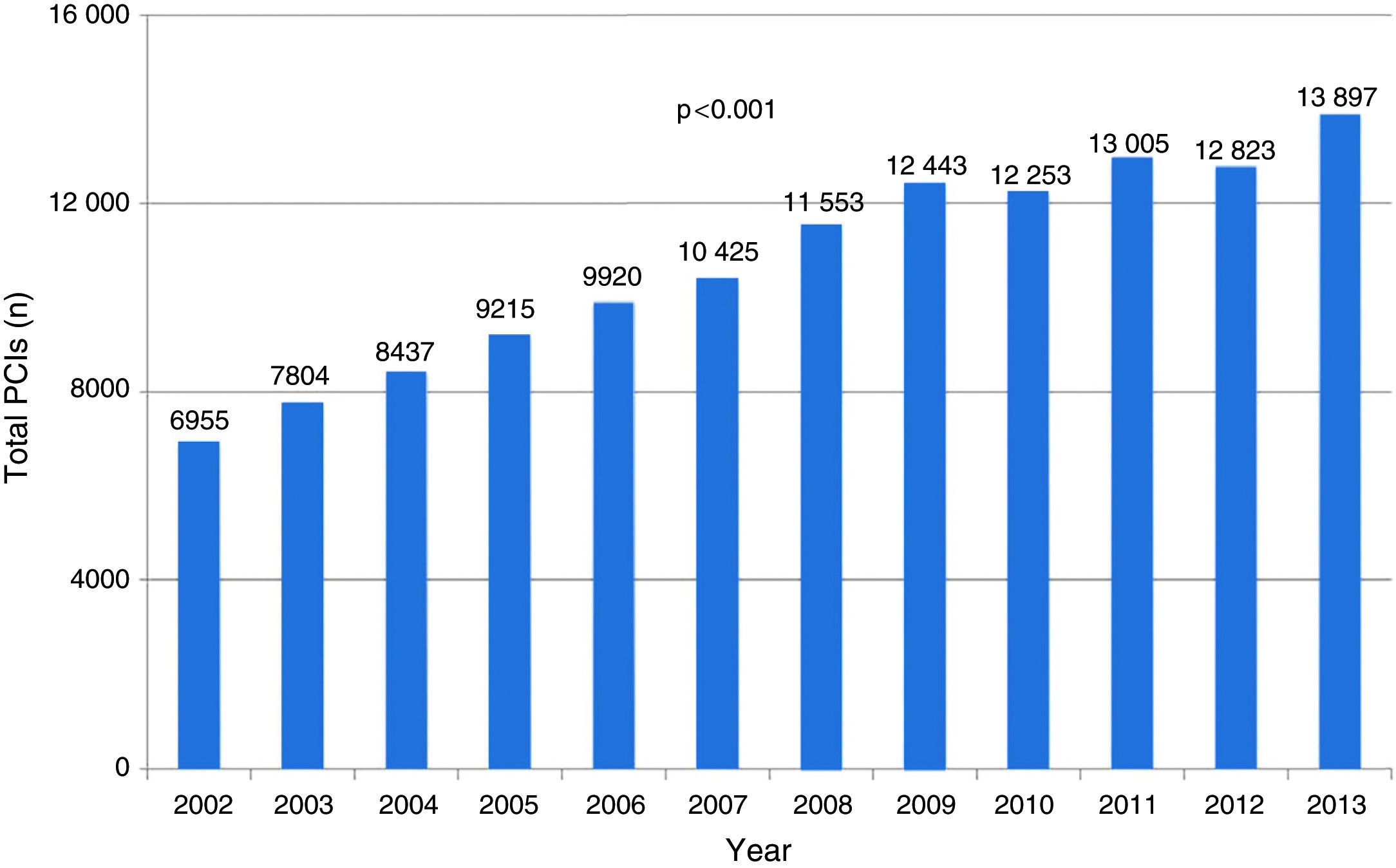
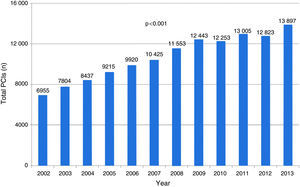
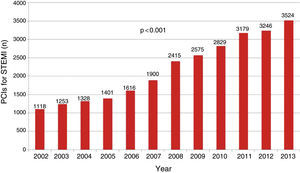
ResultsFigure 2 shows developments in percutaneous coronary intervention (PCI) in Portugal between 2002 and 2013. In absolute terms, p-PCI rates tripled in that period (p<0.001) (Figure 3), with a steady rise from 106 to 338 p-PCIs per million population (p<0.001) (Figure 4).
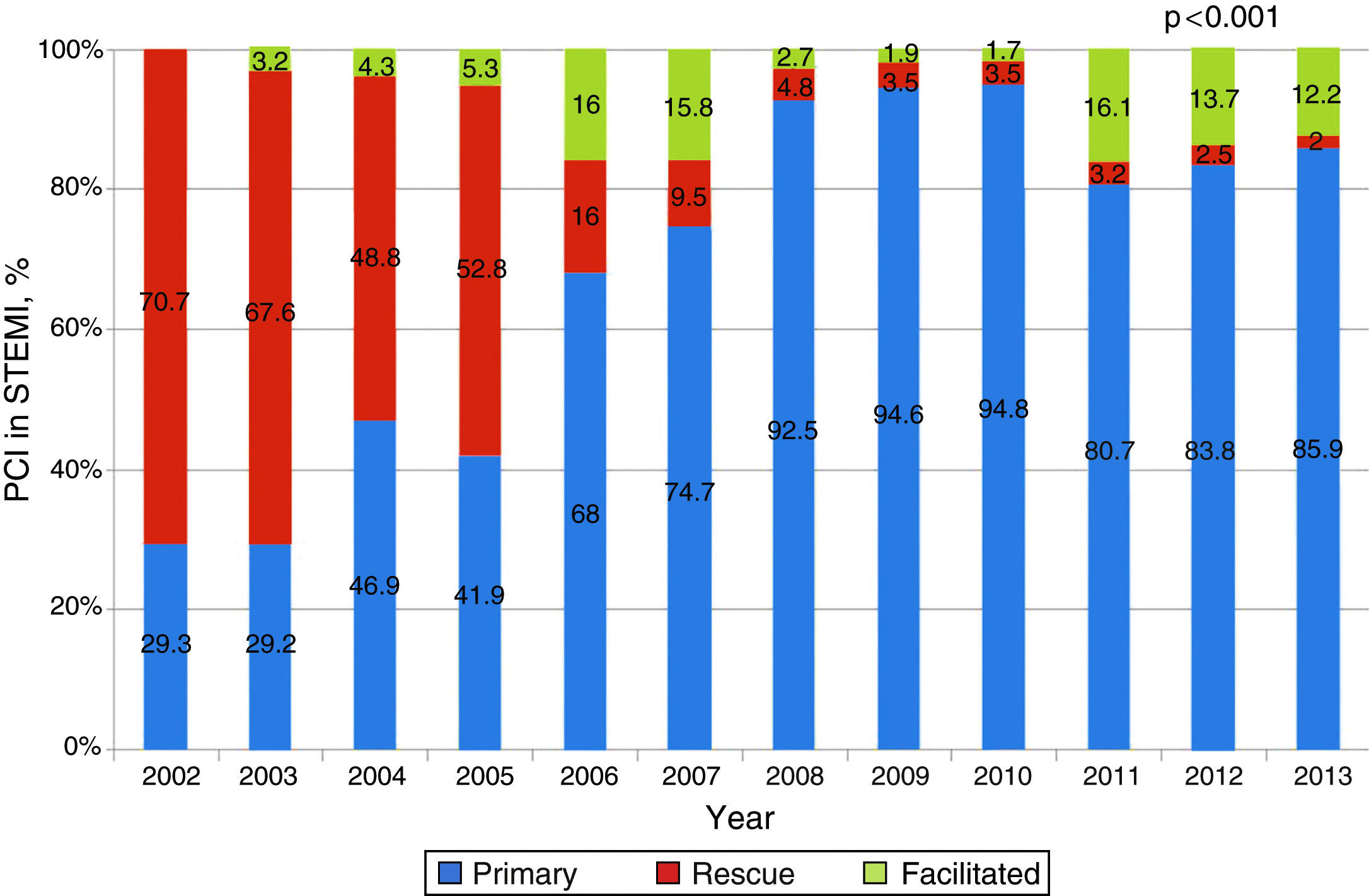
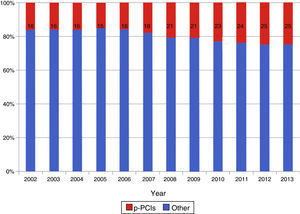
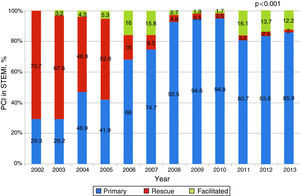
At the beginning of the study period, rescue angioplasty predominated, accounting for 70.7% of PCIs in the context of STEMI, whereas in the last year analyzed it represented only 2.0%, compared to 85.9% for p-PCIs (p<0.001). Between 2002 and 2013 p-PCIs increased from 16% to 25% of the total number of PCIs in Portugal (p<0.001) (Figure 5).
Figure 6 shows the percentages for primary, rescue and facilitated angioplasty for the treatment of STEMI.
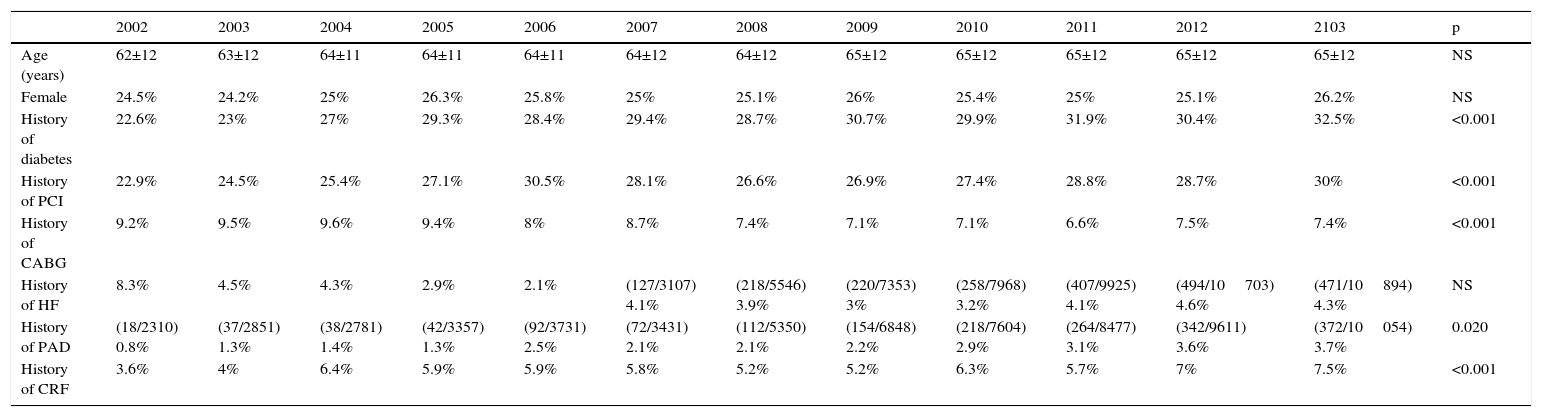
Changes in demographic characteristics and clinical history of the treated population are shown in Table 1. There were no statistically significant differences in age, gender or history of heart failure, but changes were seen in history of diabetes, PCI and chronic renal failure, all of which increased over the period under analysis, and in history of coronary artery bypass grafting, which fell in the same period.
Demographic characteristics and clinical history of the study population.
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2103 | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | 62±12 | 63±12 | 64±11 | 64±11 | 64±11 | 64±12 | 64±12 | 65±12 | 65±12 | 65±12 | 65±12 | 65±12 | NS |
| Female | 24.5% | 24.2% | 25% | 26.3% | 25.8% | 25% | 25.1% | 26% | 25.4% | 25% | 25.1% | 26.2% | NS |
| History of diabetes | 22.6% | 23% | 27% | 29.3% | 28.4% | 29.4% | 28.7% | 30.7% | 29.9% | 31.9% | 30.4% | 32.5% | <0.001 |
| History of PCI | 22.9% | 24.5% | 25.4% | 27.1% | 30.5% | 28.1% | 26.6% | 26.9% | 27.4% | 28.8% | 28.7% | 30% | <0.001 |
| History of CABG | 9.2% | 9.5% | 9.6% | 9.4% | 8% | 8.7% | 7.4% | 7.1% | 7.1% | 6.6% | 7.5% | 7.4% | <0.001 |
| History of HF | 8.3% | 4.5% | 4.3% | 2.9% | 2.1% | (127/3107) 4.1% | (218/5546) 3.9% | (220/7353) 3% | (258/7968) 3.2% | (407/9925) 4.1% | (494/10703) 4.6% | (471/10894) 4.3% | NS |
| History of PAD | (18/2310) 0.8% | (37/2851) 1.3% | (38/2781) 1.4% | (42/3357) 1.3% | (92/3731) 2.5% | (72/3431) 2.1% | (112/5350) 2.1% | (154/6848) 2.2% | (218/7604) 2.9% | (264/8477) 3.1% | (342/9611) 3.6% | (372/10054) 3.7% | 0.020 |
| History of CRF | 3.6% | 4% | 6.4% | 5.9% | 5.9% | 5.8% | 5.2% | 5.2% | 6.3% | 5.7% | 7% | 7.5% | <0.001 |
CABG: coronary artery bypass grafting; CRF: chronic renal failure; HF: heart failure; PAD: peripheral artery disease.
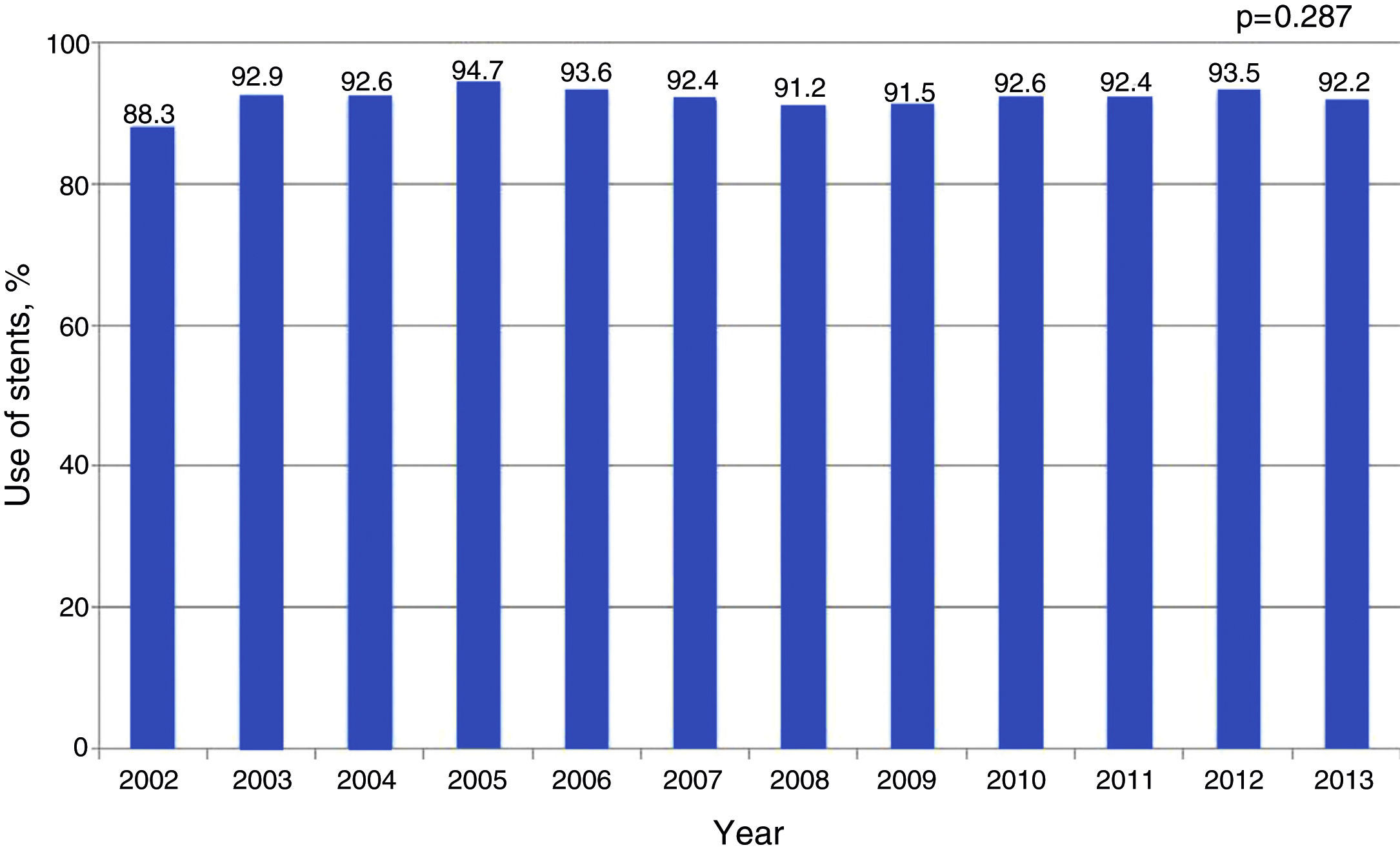
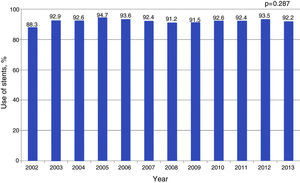
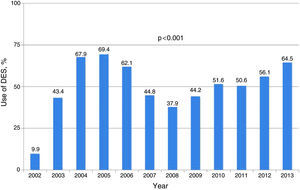
Throughout the period under analysis, stents were used in the majority of interventions (Figure 7), the rate of use being 92.2% in 2013 (p=0.287). Drug-eluting stents (DES) were used in 9.9% of interventions in 2002, the year they were first introduced in Portugal, rising to 43.4% in the following year and peaking in 2005, when they were used in 69.5% of interventions (p<0.001). In 2013 the rate was 64.5% (Figure 8).
Aspiration thrombectomy was little used before 2008, when it underwent a considerable increase, rising from 4.5% to 18.8%. In 2013 thrombectomy was used in 46.7% of p-PCIs (p<0.001) (Figure 9).
In 2002, glycoprotein IIb/IIIa inhibitors were used in 73.2% of p-PCIs, but this figure fell significantly from 2006 (22.5%) onward (Figure 10), and was 23.6% in 2013 (p<0.001).
Radial access was infrequent between 2002 and 2007, but began to increase in 2008, from 8.3% in that year to over half (54.6%) in 2013 (p<0.001) (Figure 11).
DiscussionAlthough coronary angioplasty was developed and introduced in the 1980s, the efficacy of p-PCI for the treatment of STEMI was not generally accepted until a decade later.5 In the years 1998 to 2001, 442, 641, 769 and 957 p-PCIs, respectively, were performed in Portugal.6 The data published here complete the picture for p-PCI in Portugal up to 2013. There has been a steady increase in numbers of p-PCI procedures for STEMI, the largest rise (27%) being between 2007 and 2008. Of particular note is the higher proportion of p-PCIs compared to other coronary interventions: at the beginning of the study period, p-PCIs accounted for 16% of centers’ activity, but reached 25% in the last two years of the registry. This increase means greater demands in terms of training and organization, since such procedures are more unpredictable and less easily controlled.
It is also interesting to note the changing role of p-PCI over the years in relation to other types of angioplasty in the context of STEMI. In 2002 no cases of facilitated angioplasty were recorded, and rescue angioplasty accounted for 70.7% of procedures for STEMI. However, the percentage of rescue angioplasty progressively decreased and in 2007 reached single figures. DGS data show an inverse relation between developments in p-PCI and use of fibrinolysis.2
Stenting was routine for STEMI during the period under analysis, over 85% in all years. The rate of DES use in p-PCI was 43.4% in the year following their introduction in Portugal, at a time when there was no consensus concerning their use in STEMI. DES use peaked in 2005 (69.4%), followed by a steep fall (to 37.9% in 2008), due to the concerns expressed at the European Society of Cardiology (ESC) Congress in Barcelona in 2006 about the increased thrombogenicity of DES.7 Subsequently, DES regained ground, reaching 64.5% in 2013, in accordance with the current European guidelines for myocardial revascularization.1
The TAPAS trial8 suggested that routine aspiration thrombectomy was of benefit, and was a factor in the increase in manual aspiration thrombectomy seen from 2008 onward (from 4.5% in 2007 to 18.8% in 2008), reaching 46.7% in the last year of the study period. These figures do not reflect the results of the TASTE9 and TOTAL10 trials, which were published after the time frame of the present study. In agreement with the most recent findings, an analysis of RNCI data did not demonstrate any advantage of aspiration thrombectomy.11
The use of glycoprotein IIb/IIIa inhibitors fell by 68% between 2002 (73.2%) and 2013 (23.6%), possibly due to the introduction of new adjuvant therapies, including bivalirudin and new antiplatelet agents. Low molecular weight heparin has been rarely used throughout the study period.
Radial access was an infrequent approach until 2008, when it increased to 8.3%, and since then has shown significant annual growth, reaching 54.6% in 2013. This is in line with practice in other procedures in Portugal12 and with the good results of the STEMI-RADIAL13 and MATRIX14 trials.
Access to p-PCI in Portugal has shown a positive evolution, with good growth rates and incorporation of innovative technologies. In the European context, Portugal had some of the lowest rates of p-PCI per million population per year in the last decade, especially compared to northern Europe. In a 2010 study by Widimsky et al.,15 Portugal was among the countries performing less than 200 p-PCIs per million population per year, with only 19% of STEMI patients treated by p-PCI and with 37% not reperfused by either angioplasty or fibrinolysis. The main factor in the latter figure may be that 55% of patients were admitted more than 12 hours after symptom onset.16 Equally troubling was the low proportion (23%) of patients who dialed the national emergency number. Other Mediterranean countries presented similar figures, in stark contrast to northern European countries, in which the number of p-PCIs per million population per year was over 600. It was against this background that at the ESC Congress in 2009, the ESC launched the Stent for Life (SFL) initiative,17–19 aimed at reducing mortality from STEMI by achieving a rate of 600 p-PCIs per million population per year. Portugal joined the SFL in 2011 through the Portuguese Association of Cardiovascular Intervention (APIC) of the SPC, and a task force was set up to identify the main barriers to improving the p-PCI program in Portugal.20 In a more recent review by Kristensen et al.,21 published in 2014 and analyzing data for 2010/2011 from 37 European countries in the light of the SFL initiative, Portugal's indicators are much more favorable, approaching the European average. Northern European countries continue to present the highest rates of p-PCI, but the figures for Portugal are similar to those of Belgium (297 per million population per year), Spain (225), Finland (265), Greece (346), Greenland (396), and England and Wales (286). There are several factors behind this improvement: the solid evidence in favor of p-PCI, local cooperation between referring institutions and interventional cardiology centers, a larger and more efficient coronary fast-track system, the actions of the SFL campaign, and innovations that have led to improvements in PCI techniques and adjuvant therapies.
Study limitationsThe RNCI has certain limitations. Inclusion of data from all centers was only achieved in 2013, and the figures presented here are based on the patients included in the registry for specific years, which ranged between 37% in 2002 and 99% in 2012. Not all patients are followed systematically, and so data on in-hospital and post-discharge clinical outcomes cannot be presented. The RNCI also does not currently have either internal or external auditing.
ConclusionsThe rate of primary angioplasty per million population per year in Portugal tripled between 2002 and 2013. Rescue angioplasty was overtaken by p-PCI as the predominant procedure in 2006. New trends in the treatment of STEMI have emerged, notably the use of DES and radial access, both of which became the preferred option in 2013.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
We are grateful to Dr. Adriana Belo, a biostatistician at the CNCDC, for her assistance in processing the data from the RNCI.
Please cite this article as: Pereira H, Campante Teles R, Costa M, et al. Angioplastia primária em Portugal entre 2002-2013. Atividade segundo o Registo Nacional de Cardiologia de Intervenção. Rev Port Cardiol. 2016;35:395–404.