Oral anticoagulation (OAC) is an effective treatment in the prevention of thromboembolic events in patients with atrial fibrillation (AF). The aim of this review was to estimate the prevalence of OAC therapy in patients with AF in Portugal.
MethodsMEDLINE, the Index of Portuguese Medical Journals and SIBUL (the Bibliographic Catalog of the Integrated Library System of the University of Lisbon) were searched for Portuguese observational studies reporting the proportion of anticoagulated patients with AF. The pooled estimated prevalence of anticoagulated patients and respective 95% confidence interval (CI) were determined by means of a meta-analysis.
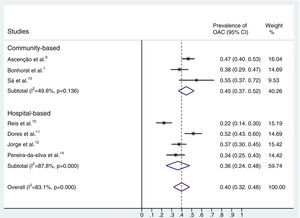
ResultsSeven studies were included for analysis, of which four were conducted in a hospital environment and three in the general community. These studies enrolled a total of 891 patients with AF. The pooled estimated prevalence of anticoagulated patients was 40% (95% CI: 32–48%).
ConclusionsThe prevalence of OAC in Portuguese AF patients is low. There is a need to promote change in OAC prescribing habits for AF patients in Portugal, in accordance with international guidelines.
A anticoagulação oral é uma terapêutica eficaz na prevenção de eventos tromboembólicos, em doentes com fibrilhação auricular (FA). A presente revisão pretendeu estimar a prevalência da terapêutica anticoagulante oral em doentes com FA em Portugal.
MétodosFoi realizada uma pesquisa nas bases de dados MEDLINE, Índex de Revistas Médicas Portuguesas e Catálogo Bibliográfico do Sistema Integrado de Bibliotecas da antiga Universidade Clássica de Lisboa (SIBUL). Estudos observacionais nacionais que reportavam a proporção de doentes anticoagulados com fibrilhação auricular foram incluídos. A estimativa combinada de prevalência de doentes com FA anticoagulados e o respetivo intervalo de confiança 95% (IC95%) foi determinada com recurso a meta-análise.
ResultadosDos sete estudos incluídos, três estudos foram realizados em ambiente hospitalar e quatro foram realizados na comunidade em geral. Do total de 891 doentes com FA, a estimativa de prevalência de doentes anticoagulados foi de 40% (IC95% 32-48%).
ConclusõesA prevalência de doentes com FA anticoagulados na população estudada é baixa. É necessário promover a mudança dos hábitos de prescrição de anticoagulantes em doentes com FA em Portugal, em concordância com as recomendações internacionais.
Atrial fibrillation (AF) is the most common arrhythmia in clinical practice, with an estimated prevalence of 2.5% in the Portuguese population aged 40 and over according to the FAMA study. The prevalence increases with age, reaching 6.6% in the group aged 70 and over and 10.5% in those aged 80 and over.1
In the FAMA study, a third of patients with AF were not aware that they had the condition. As AF can remain silent until complications occur,2,3 clinical screening is indicated for individuals aged 65 or over.4 The main complications of AF are thromboembolic events, particularly stroke. For prevention of such events oral anticoagulation therapy (OAC) is recommended in patients with thromboembolic risk factors.4
The aim of this review was to estimate the prevalence of OAC therapy in patients with AF in Portugal by means of a systematic review and meta-analysis of epidemiologic studies.
MethodsSelection criteriaObservational studies performed in mainland Portugal and/or the islands of Madeira and the Azores that enrolled patients with AF or atrial flutter (whether paroxysmal, persistent or permanent) and reported the proportion of anticoagulated patients were included. Studies on specific populations or on specific interventions such as AF ablation were excluded since inclusion of patients who are not representative of the general AF population would introduce bias.
Databases and searchesMEDLINE, the Index of Portuguese Medical Journals and SIBUL (the Bibliographic Catalog of the Integrated Library System of the University of Lisbon) were searched. The search included review of the references lists of the studies and literature reviews found, but did not include abstracts of posters or oral communications at congresses.
Selection of studies and data extractionPotentially eligible studies were selected independently by two of the authors using the above inclusion and exclusion criteria and entered in a data extraction form showing the demographic characteristics of the study, the thromboembolic risk factors of the population and the proportion of anticoagulated patients.
The selected studies were assessed qualitatively using criteria related to sampling, measurement and analysis.5 No study was excluded on the basis of possible bias.
Any disagreement between the investigators was resolved by consensus.
Data synthesisThe Stata® Statistical Software Package, version 11.0 (StataCorp LP, College Station, TX), was used to synthesise the results through meta-analysis and to determine the pooled estimated prevalence of anticoagulated AF patients. In studies that stratified the population's thromboembolic risk, the denominator of prevalence was the proportion of patients indicated for OAC. The results of the individual and pooled studies were expressed in percentages (prevalence) and 95% confidence intervals (CI). Inverse-variance weighting was used to aggregate the results of each study. As considerable heterogeneity between studies was expected, the random-effects model of DerSimonian and Laird6 was used by default.
Statistical heterogeneity was assessed using the I2 test, which calculates the percentage of total variation across studies that is due to heterogeneity rather than chance.7 An I2 of ≥50% indicates significant heterogeneity.8
In a separate analysis, estimates of prevalence were calculated as a function of the environment of the study (community or hospital).
ResultsSeven studies were included for analysis.1,9–14 Supplementary Data Figure 1 shows the flowchart for study selection. Three studies were cross-sectional1,9,13 and four were longitudinal (three retrospective cohort studies10–12 and one prospective cohort study15). Three were conducted in the general community1,9,13 and four in a hospital environment.10–12,14 These studies enrolled a total of 891 AF patients eligible for OAC. Sample size ranged between 21 and 261 individuals, most of them elderly (mean age varying between 77 and 85.5 years) and thus generally at high thromboembolic risk. Three studies included patients with significant valve disease or mechanical valves: in Jorge et al., 29% of the population had at least moderate valve disease or mechanical valves,12 in Ascenção et al., 20% had mitral stenosis,9 and in Dores et al., 6% of the population had valvular AF.11 Thromboembolic risk stratification was performed using the CHADS2 and CHA2DS2-VASc scores and the risk categories proposed in the 2006 American College of Cardiology/American Heart Association/European Society of Cardiology (ACC/AHA/ESC) guidelines32 (Table 1). Two studies did not report using any risk stratification tools.1,10
Main characteristics of the selected studies.
| Study | Study designEnvironment | Study period | Patients eligible for OAC (n) | Mean/median age (years) | Indication for OAC |
| Ascenção et al.9 | Cross-sectionalCommunity (general practitioner sentinel network) | June 2003–November 2003 | 243 | 84% >65 | CHADS2 ≥2, mitral stenosis or intracavitary thrombus |
| Reis et al.10 | RetrospectiveHospital (HFF) | January 1996–December 2004 (data from 2004) | 108 | 78.6 | – |
| Bonhorst et al.1 | Cross-sectionalCommunity | – | 119 (previous diagnosis of AF)/69% total AF | 77 | – |
| Dores et al.11 | RetrospectiveHospital (HSFX) | October 2006–October 2007 | 126 | 77 | Moderate to high risk according to 2006 ACC/AHA/ESC guidelines |
| Jorge et al.11 | RetrospectiveHospital (HUC) | December 2005–June 2007 | 161 | 80.9 | CHADS2 ≥2 |
| Sá et al.12 | Cross-sectionalCommunity (USFSaúde em Família, Maia) | 2011 | 31 | 85.5 | CHA2DS2-VASc ≥2 |
| Pereira-Da-Silva et al.14 | RetrospectiveHospital (CHLC) | April 2011–October 2011 | 103 | 79.6 | CHA2DS2-VASc ≥2 |
ACC/AHA/ESC: American College of Cardiology/American Heart Association/European Society of Cardiology; AF: atrial fibrillation; CHLC: Centro Hospitalar Lisboa Central; HFF: Hospital Prof. Dr. Fenando Fonseca; HSFX: Hospital São Francisco Xavier; HUC: Hospitais da Universidade de Coimbra; OAC: oral anticoagulation; USF: Family Health Unit.
The main characteristics of the studies included are shown in Table 1. The quality of the methodology in all seven studies was reasonable. The main source of possible bias was the lack of representativeness of the sample – some studies were performed exclusively in a hospital environment or analyzed patient subgroups. A qualitative analysis of the risk of bias is presented in Supplementary Data Figure 2. The meta-analysis of the results reveals that the prevalence of OAC therapy in Portuguese patients with AF is 40% (95% CI: 32–48%), higher in community-based (45%; 95% CI: 37–52%) than in hospital-based studies (36%; 95% CI: 24–48%), although this difference was without statistical significance (p=0.20). These results are presented in Figure 1.
To assess the effect of including studies that used different risk stratification tools, we analyzed the results for different subgroups. The differences between the estimates obtained by different methods were not significant (p=0.31); the prevalence of anticoagulated patients was higher (44% [37–51%] vs. 30% [15–45%]) in studies that reported using risk stratification tools than in those that did not, but this was also not statistically significant (p=0.10).
DiscussionAF is an important public health issue, particularly in Portugal, since it is a risk factor for stroke, a significant cause of morbidity and mortality in this country.15 The risk of stroke is five times higher in patients with AF, increasing with age.16 Over 15% of strokes are due to AF and they are generally more severe than those not associated with AF.17,18 Stroke attributable to AF is associated with a 30-day mortality of 25% and one-year mortality of 50%.17 These patients have longer hospital stays and greater use of health resources.19,20
There is solid evidence that OAC reduces the risk of thromboembolic events. Use of vitamin K antagonists is associated with a significant reduction of 64% in relative risk for stroke,21 and the new oral anticoagulants (direct thrombin and Xa inhibitors) have been shown to be at least as effective as vitamin K antagonists.
The low prevalence of anticoagulated patients found in this review underlines the need to promote change in prescribing habits. The prevalence found in this study (40%) is close to that in the Italian ISAF study (46%).22 However, another study in Italy, based on cardiology units, showed a considerably higher prevalence of anticoagulation in AF patients with indication for OAC,23 and other recent studies paint a more optimistic picture. The international prospective GARFIELD registry reported a prevalence of 62% of OAC in patients with AF and CHADS2 score ≥224; the German ATRIUM registry, based on primary care data, found a prevalence of 75% in patients with AF and high thromboembolic risk25; and the PREFER in AF registry, using data from seven European countries, showed a prevalence of 85%.26
Both in clinical trials and in the real world, various reasons have been put forward for the failure of physicians to prescribe OAC for AF patients.24,27
In a hospital-based study, Dores et al. found that 19% of patients with AF were considered to be contraindicated for OAC, the most frequent reasons being previous bleeding dyscrasia, alcoholism, renal disease and inability to control INR.11
Pereira-Da-Silva et al. assessed predictors of non-prescription of OAC in 103 eligible patients with AF and the reasons given by physicians.11 On multivariate analysis, bedridden status or dementia and large number of bleeding risk factors predicted non-prescription. In the 68 patients who were not prescribed OAC, the most frequent reasons were high bleeding risk (56%), perceived lack of benefit (22%), inability to follow the therapeutic regimen (10%) and difficulty in monitoring INR (7%).14 The reasons given for not prescribing new-generation anticoagulants were their high cost (some not being subsidized by the State), lack of expected benefit, and bleeding risk.14
Despite their cost, the new anticoagulants, as well as being cost-effective,28,29 can overcome some of the barriers to prescription, particularly because they do not require regular INR monitoring and have fewer drug-drug and drug-food interactions.
The current European Society of Cardiology guidelines recommend thromboembolic risk stratification using the CHA2DS2-VASc score, a score of 0 indicating that the patient would not benefit from OAC.4,30 Some studies in this review used the previously recommended risk stratification tool, CHADS2,31 or the algorithm proposed in the 2006 ACC/AHA/ESC guidelines.32 Since the latter two exclude or underestimate risk in a proportion of patients who would benefit from OAC, the prevalence of anticoagulation in patients indicated for the therapy could be even lower when based on the CHA2DS2-VASc score.
Furthermore, two studies included a considerable number of patients with significant valve disease or prosthetic valves.9,12 These patients are more likely to be anticoagulated than those with non-valvular AF; even so, the prevalence of OAC was low in both studies.
The considerable heterogeneity found is not uncommon in prevalence studies, due to multiple factors related to patients, institutions and prescribers.
The heterogeneity observed between studies in the community compared to those in a hospital environment may be due to various factors, the most obvious of which is the inclusion of Reis et al.10 in the meta-analysis. This is the oldest of the hospital-based studies, published in 2006 but analyzing OAC in patients admitted in 2004; in this year there were 122 patients hospitalized for AF, of whom 108 were indicated for long-term OAC, but only 22.2% of these were anticoagulated at discharge.10
There are several possible reasons for the low rate of OAC in hospital-based studies, particularly Reis et al., including older age and the presence of comorbidities that would tend to heighten perception of greater bleeding risk. Both these reasons have been put forward as a restraint on physicians prescribing OAC for fear of severe bleeding, or the belief that the thromboembolic risk is lower than the bleeding risk.33 Moreover, some of the studies included in our review predated the publication of the Birmingham Atrial Fibrillation Treatment of the Aged (BAFTA) study in 2007, which showed that warfarin with a target INR of 2.0–3.0 was superior to aspirin in preventing cardiovascular events in patients aged ≥75 years, with no significant differences in bleeding risk.34
LimitationsThe conclusions of this review should be assessed bearing in mind the inherent limitations of the methodology used (a meta-analysis of pooled study results rather than data on individual patients). The inclusion of different population samples, ages, environments (community vs. hospital) and thromboembolic risk stratification tools (CHADS2, CHA2DS2-VASc and the 2006 ACC/AHA/ESC Guidelines), all of which lead to clinical heterogeneity, should be taken into consideration as well as the expected statistical heterogeneity.
ConclusionsThe prevalence of OAC in Portuguese patients with AF is around 40%. Despite the evidence and the recommendations concerning the reduction of thromboembolic risk in AF patients with this therapy, a significant proportion of the population at risk is not anticoagulated. The level of OAC prescription in these patients is an indication of the quality of health care, and there is an obvious need for change.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Caldeira D, Barra M, David C, et al. Prevalência da anticoagulação oral em doentes com fibrilhação auricular em Portugal: revisão sistemática e meta-análise de estudos observacionais. Rev Port Cardiol. 2014;33:555–560.