Takotsubo syndrome (TTS) is an acquired transient type of systolic dysfunction which mimics myocardial infarction clinically and electrocardiographically. TTS is also known as stress cardiomyopathy, broken heart syndrome, apical ballooning, reversible acute heart failure, neurogenic stunned myocardium or acute catecholamine cardiomyopathy. This case report describes an uncommon presentation of myocardial stunning after an anesthetic procedure.
A 14-year-old girl with a history of pineal cyst and hemiplegic migraine was admitted for control brain magnetic resonance imaging. During anesthesia induction with propofol she suffered bradycardia, which was reversed with atropine, followed by tachyarrhythmia, reversed with lidocaine and precordial thump. Within hours she developed pulmonary edema and global respiratory failure due to acute left ventricular dysfunction. A transthoracic echocardiogram showed a dilated left ventricle with global hypokinesia and depressed left ventricular systolic function (ejection fraction <30%). The electrocardiogram showed persistent sinus tachycardia and nonspecific ST-T wave abnormalities. Cardiac biomarkers were elevated (troponin 2.42 ng/ml, proBNP 8248 pg/ml). She was placed on diuretics, angiotensin-converting enzyme inhibitors, digoxin and dopamine. The clinical course was satisfactory with clinical, biochemical and echocardiographic improvement within four days. Subsequent echocardiograms showed no ventricular dysfunction. The patient was discharged home on carvedilol, which was discontinued after normalization of cardiac function on cardiac magnetic resonance imaging.
Few cases of TTS have been described in children, some of them triggered by acute central nervous system disorders and others not fulfilling all the classical diagnostic criteria. In this case the anesthetic procedure probably triggered the TTS.
A síndrome Takotsubo (STT) é uma forma adquirida e transitória de disfunção sistólica, cuja apresentação clínica e eletrocardiográfica mimetiza um enfarte agudo do miocárdio. A STT é também conhecida como miocardiopatia de stress, síndrome do «coração partido», balonamento apical, insuficiência cardíaca aguda reversível, miocárdio «atordoado» (forma neurogénica) ou miocardiopatia aguda das catecolaminas. Os autores descrevem uma apresentação rara de STT após procedimento anestésico.
Adolescente de 14 anos, sexo feminino, com antecedentes pessoais de enxaqueca hemiplégica e quisto pineal, submetida a ressonância magnética (RM) cranioencefálica de controlo. Durante a indução anestésica com propofol verificou-se bradicardia, revertida com atropina, seguida de taquidisritmia ventricular, revertida com lidocaína e murro pré-cordial. Nas primeiras horas de internamento evoluiu para edema pulmonar associado a insuficiência respiratória global por disfunção ventricular esquerda aguda. O ecocardiograma transtorácico mostrou dilatação do ventrículo esquerdo com hipocinesia global e fração de ejeção reduzida (<30%). O eletrocardiograma revelou taquicardia sinusal persistente e alterações inespecíficas do segmento ST. Os biomarcadores cardíacos encontravam-se elevados (troponina 2,42 ng/ml, proBNP 8248 pg/ml). Foi medicada com diuréticos, IECA, digitálico e dopamina, com melhoria clínica, bioquímica e ecocardiográfica ao quarto dia. Os ecocardiogramas subsequentes mostraram normalização da função ventricular. A doente teve alta medicada com carvedilol, que suspendeu após normalização da função cardíaca e RM cardíaca não ter revelado alterações.
Estão descritos poucos casos de STT em idade pediátrica. Alguns são desencadeados por patologia aguda do sistema nervoso central, mas nem todos cumprem os critérios de diagnóstico clássicos. Neste caso, o procedimento anestésico poderá ter desencadeado a STT.
Takotsubo syndrome (TTS) is one of the unclassified cardiomyopathies, nonfamilial form.1 It is an acquired transient type of systolic dysfunction which mimics myocardial infarction clinically and electrocardiographically.2 TTS is also known as stress cardiomyopathy, broken heart syndrome, apical ballooning, reversible acute heart failure, neurogenic stunned myocardium or acute catecholamine cardiomyopathy.3
Various pathophysiological mechanisms have been proposed but the most widely accepted is an excess of catecholamines, leading to disruption of contraction and ventricular function,1 which return to baseline values within days or weeks.4 The clinical setting depends on the extent of myocardium affected and associated complications, which can include chest pain, dyspnea, palpitations, diaphoresis, nausea, vomiting or neurological symptoms.1,3
The authors describe a case of TTS in a pediatric patient after an anesthetic procedure, which presented as heart failure and acute pulmonary edema.
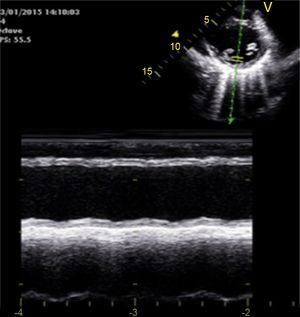
Case reportA 14-year-old girl with a history of hemiplegic migraine and pineal cyst was admitted for control brain magnetic resonance imaging (MRI). During anesthesia induction with propofol she suffered bradycardia, which was reversed with atropine, followed by ventricular tachyarrhythmia, reversed with lidocaine and precordial thump. Within hours she developed pulmonary edema (Figure 1) and global respiratory failure (PaO2/FiO2 156, pCO2 57 mmHg) and hypotension (systolic/diastolic blood pressure 89/56 mmHg). The transthoracic echocardiogram showed a dilated left ventricle with global hypokinesia of the mid and basal segments but sparing the apex, resulting in moderate to severe impairment of left ventricular global systolic function and reduced ejection fraction (<30%) (Figures 2 and 3). The electrocardiogram (ECG) showed persistent sinus tachycardia and nonspecific ST-T wave abnormalities in V4 and V5 (Figure 4). Cardiac biomarkers were elevated (total creatine kinase [CK] 217 UI/l, troponin I 2.42 ng/ml and pro-brain natriuretic peptide [proBNP] 8284 pg/ml). The patient was placed on diuretics and captopril, with dopamine to optimize renal function (maximum 2 μg/kg/min) and digoxin in the first 24 h.
Repeat echocardiography was performed daily, and the patient showed clinical and echocardiographic improvement within 48 h and complete recovery of left ventricular systolic function on day 4. Cardiac biomarkers decreased in the first few days (troponin I 0.69 ng/ml on day 2 and 0.44 ng/ml on day 3; proBNP 2842 pg/ml on day 3), with normalization of total CK and troponin I and a significant fall in proBNP (329 pg/ml) on day 6. Diuretics were discontinued on day 9 and the patient was discharged, medicated with carvedilol. Cardiac MRI showed no alterations such as myocarditis scar or infarct scar, and carvedilol was discontinued. Other diagnostic tests showed normal thyroid function and negative viral serologies for CMV, EBV, HSV-1, HSV-2, HSV-6, parvovirus, adenovirus, influenza A and enterovirus. The patient is being regularly followed in pediatric cardiology consultations.
DiscussionThe authors describe the case of an adolescent girl who, in the context of emotional stress triggered by anesthesia induction, developed heart failure with acute pulmonary edema, elevation of cardiac biomarkers and nonspecific electrocardiographic alterations, and subsequently completely recovered cardiac function. This presentation is suggestive of TTS, which most commonly occurs between 60 and 75 years of age and is rare at pediatric ages. There are only 28 reported cases in this age-group, some in the context of acute disorders including cancer of the central nervous system or traumatic brain injury.3 However, TTS can also occur without neurological involvement, in the context of systemic disease including celiac disease or infection, ventricular septal defect or ventricular tachycardia, and even with no known triggering factor.3
Other triggers, such as emotional or physical stress, have been described in adults.1 According to the literature, there has been one case to date of TTS associated with an anesthetic procedure in an adult5 and a few cases in pediatric patients in the postoperative period following neurosurgery, which were considered neurogenic.6,7
The first diagnostic criteria were proposed by the Mayo Clinic in 2004,8 and revised in 2010, and are considered the classic criteria. They are as follows: 1) transient hypokinesis, akinesis or dyskinesis of the left ventricular mid segments, with or without apical involvement, with regional wall motion abnormalities extending beyond a single epicardial vascular distribution; a stressful trigger is often, but not always, present; 2) absence of obstructive coronary disease or angiographic evidence of acute plaque rupture; 3) new electrocardiographic abnormalities (ST-segment elevation and/or T-wave inversion), or modest elevation in cardiac troponin level; 4) absence of pheochromocytoma or myocarditis.9,10 Nevertheless, these criteria are not consensual and various other guidelines have been proposed over the years for the diagnosis of TTS. In 2007 the Japanese Circulation Society published their own guidelines, which included a revised definition of TTS and exclusion and reference criteria for the diagnosis.11 These are now considered outmoded, since they exclude atypical forms of TTS in which cardiac segments other than the apex are involved, which have now been reported in the literature.12 In 2012 the Johns Hopkins diagnostic criteria were published, which include mandatory and optional criteria, and exclude TTS in patients with a history of acute coronary syndrome.13 The Gothenburg criteria were also presented in 2012, in which the main difference from the Mayo Clinic criteria relates to the possibility of under-diagnosing TTS if all patients with coronary disease or pheochromocytoma are excluded. They also highlight the possibility of milder forms of TTS or different degrees of TTS-like cardiac dysfunction in the general population.14 In 2014, in the light of increased clinical experience, new TTS diagnostic criteria were proposed that included two new notions: of formes frustes of TTS and of comorbidities that precipitate or are brought about by TTS, such as acute coronary disease.12
The classic Mayo Clinic diagnostic criteria require cardiac catheterization for a diagnosis of TTS. However, according to some case reports, this may not be necessary in pediatric patients depending on the clinical course and if laboratory and echocardiographic findings are typical and favorable.4,15,16
TTS may present echocardiographically in the classical form (with apical ballooning and involvement of the apical or mid-apical segments) or the inverted form (with involvement of the mid, basal or mid-basal segments).3 The case presented was of the inverted or global form, both reported at pediatric ages.3
Treatment of TTS is basically supportive and includes angiotensin-converting enzyme inhibitors, beta-blockers, calcium antagonists or diuretics,3 which can be used until recovery of cardiac function.1 The prognosis of TTS is good,1,3 and cardiac biomarkers normalize within 5-7 days,15 the ECG within 10 weeks and the echocardiogram within six weeks after onset.3 The time to recovery of cardiac function in pediatric patients is less well established3 but it appears to occur earlier in some cases, even as early as seven days after diagnosis.4,6,15
In the case presented, the anesthetic procedure, together with possible associated emotional stress, may have triggered TTS. The diagnosis should be considered in children and adolescents with signs of cardiac dysfunction in the context of anesthesia induction and/or situations of emotional or physical stress.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Oliveira JF, Pacheco SR, Moniz M, et al. Síndrome Takotsubo após procedimento anestésico em idade pediátrica – um caso clínico. Rev Port Cardiol. 2016;35:375.e1–375e5.