Purulent pericarditis is a rare entity, defined as the presence of neutrophilic pericardial effusion which is infected by a bacterial, fungus or parasite agent. The diagnosis can be challenging, especially if patients have taken previous antibiotic therapy; on the other hand the recognition of this pathology is often made late, with the onset of severe symptoms or signs of cardiac tamponade or even only at the autopsy. The authors describe the case of a 82-year-old woman with history of extensive laceration of the right lower limb from a dog bite in July 2016, admitted to the Cardiology Department one month later for Acute Pericarditis. During hospitalization she maintained recurrent fever peaks despite the treatment with non-steroidal anti-inflammatory drugs and colchicine. She collected blood cultures and repeated echocardiogram showed increased pericardial effusion with no signs of hemodynamic compromise. Blood cultures revealed the presence of Pasteurella multocida. Due to clinical suspicion of purulent pericarditis, pericardiocentesis was performed with drainage of liquid compatible with exudate and the patient was presented to the Cardiothoracic Surgery Department for pericardiotomy and adequate drainage of the liquid. Histological examination confirmed the diagnosis of Acute Pericarditis. It should be noted that Pasteurella is a very frequent agent (50-90%) in the gastrointestinal tract and nasopharynx of many domestic animals, namely dogs.
The authors emphasize the need to aggressively treat this pathology, since untreated death is inevitable.
A pericardite purulenta é uma entidade rara, definida como a presença de derrame pericárdico neutrofílico infetado por um agente bacteriano, fungo ou parasita. O diagnóstico pode ser desafiante, especialmente se os doentes fizeram antibioterapia previamente; por outro lado, o reconhecimento dessa patologia é feito, muitas vezes, tardiamente, quando do aparecimento de sintomas graves ou sinais de tamponamento ou mesmo apenas na autópsia. Os autores descrevem o caso de uma mulher, 82 anos, com antecedentes de laceração extensa do membro inferior direito por mordedura de cão em julho de 2016, internada no Serviço de Cardiologia um mês depois por suspeita de pericardite aguda. Durante o internamento manteve picos febris recorrentes apesar da terapêutica com anti-inflamatórios não esteroides e colchicina. Colheu rastreio sético e repetiu ecocardiograma, que revelou aumento do derrame pericárdico, sem sinais de compromisso hemodinâmico, e as hemoculturas revelaram a presença de Pasteurella multocida. Por suspeita clínica de pericardite purulenta fez pericardiocentese com drenagem de líquido compatível com exsudado e foi apresentada ao Serviço de Cirurgia Cardiotorácica para pericardiotomia e drenagem adequada do líquido purulento. O exame histológico confirmou o diagnóstico de pericardite aguda. De salientar que a Pasteurella é um agente muito frequente (50-90%) no trato gastrointestinal e nasofaringe de muitos animais domésticos, nomeadamente cães.
Os autores realçam a necessidade de tratar agressivamente essa patologia, uma vez que se não tratada a morte é inevitável.
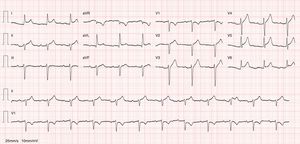
The authors describe the case of an 82-year-old woman with history of essential hypertension, implant of a dual-chamber pacemaker, hypothyroidism, spondylodiscitis from Enterococcus faecalis in July 2015 and extensive laceration of the right leg resulting from a dog bite, for which she received empiric antibiotic therapy with flucloxacillin in July 2016. She was admitted to the emergency department of our hospital in August 2016 due to pleuritic chest pain and fever developing over the previous 24-48 hours. Physical examination revealed pericardial friction rub on heart auscultation, herpetic lesion in the posterior thoracic region and fever (39°C). An electrocardiogram showed sinus rhythm with generalized ST-segment elevation and indication of PR depression (Figure 1). The laboratory work-up showed leukocytosis (16.20×10E9/l) with neutrophilia (90%), elevated C-reactive protein at 20.96 mg/dl (reference range <0.5 mg/dl), elevated procalcitonin at 12.3 ng/ml (reference range <0.1 ng/ml) and peak troponin I at 0.05 ng/ml (reference range <0.04 ng/ml). Chest X-ray did not show any significant abnormalities. Baseline echocardiography showed good biventricular systolic function with no segmental contractility abnormalities and mild pericardial effusion with no hemodynamic compromise. There were no significant valve abnormalities and no findings suggestive of acute aortic syndrome. The patient was admitted to the Cardiology Department due to suspected acute pericarditis.
During the hospital stay, she continued to have fever spikes despite empiric treatment with non-steroidal anti-inflammatory drugs and colchicine. Septic work-up was thus ordered and empiric antibiotic therapy was initiated. The echocardiography was repeated and showed increased pericardial effusion (severe) with no imminent signs of cardiac tamponade (Figures 2 and 3). Due to the clinical suspicion of purulent pericarditis, she underwent pericardiocentesis with drainage of 400 ml of seropurulent fluid. The biochemical analysis of the fluid revealed an exudate (pH 6.68; glucose 18 mg/dl; pericardial-fluid:serum glucose ratio 0.1; lactate dehydrogenase 9600 and presence of >1000/μl neutrophils with predominantly polymorphonuclear cells—Table 1). Blood cultures revealed Pasteurella multocida. After the case was discussed with the Infectious Diseases Department, the antibiotic therapy was changed to ceftriaxone. The patient was sent to the Cardiothoracic Surgery Department for subxiphoid pericardiotomy and suitable pericardial drainage. Microscopic examination revealed pericardium with fibroblastic proliferation and neutrophilic infiltrate in adherent masses of fibrin. The histological diagnosis was acute pericarditis. The patient was asymptomatic when discharged to outpatient care and was referred to the outpatient office. There is no record of new hospital stays to date.
Characteristics of pericardial fluid.
| Parameter | Value |
|---|---|
| pH | 6.68 |
| Glucose | 18.0 mg/dl |
| Total proteins | 4.7 mg/dl |
| LDH | 9600 U/l |
| Adenosine deaminase | 2853 |
| Cell count | >1000.0/μl (polymorphonuclear) |
| KB – direct test and PCR | Negative |
KB: Koch bacillus (Mycobacterium tuberculosis); LDH: lactate dehydrogenase; PCR: polymerase chain reaction.
Purulent pericarditis (PP) is a rare condition (<1% of cases of pericarditis) and is defined as neutrophilic pericardial effusion infected by a bacterial, fungal or parasitic agent.1
The most common culprits are staphylococci, streptococci and pneumococci, and the main associated lesions are empyema (50%) and pneumonia (33%). Staphylococcus aureus and fungi are the most common culprits in immunosuppressed individuals or following thoracic surgery. Contamination can occur through hematogenous dissemination or direct contamination from the retropharyngeal space, valves or subphrenic space. Diagnosis can be challenging, especially if patients have previously received antibiotic therapy prior to the collection of cultures. Moreover, diagnosis is delayed until severe symptoms or signs of cardiac tamponade arise, or is often made at autopsy.2–5
Acute cardiovascular decompensation (dyspnea, tachycardia and hypotension) or septic symptoms are the most common forms of presentation. Interestingly enough, it can also be insidious, with no signs of pericardial involvement until cardiac tamponade arises.3–5
Clinical suspicion of PP is an indication for urgent pericardiocentesis. Diagnosis is made by direct microscopic examination and by collecting pericardial fluid for biochemical, cytological and microbiological testing. A low pericardial-fluid:serum glucose ratio (mean 0.3) and an elevated concentration of white blood cells, with predominance of neutrophils, differentiates PP from tuberculous pericarditis (glucose ratio 0.7) and neoplastic pericarditis (ratio 0.8).3,4
Intravenous antibiotic therapy should be initiated empirically until microbiological results are received. Purulent effusions are very often loculated and have a tendency to rapidly accumulate. Draining pericardial fluid is therefore crucial. According to the European Society of Cardiology, subxiphoid pericardiotomy (IIB) and intrapericardial thrombolysis (IIa) should be considered for loculated effusions in order to provide suitable drainage. Pericardiectomy should be considered for dense adhesions, purulent loculated effusions, recurrence of tamponade and progression to constriction (IIa).3,4
PP should be treated aggressively. If left untreated, it leads to death.3 Despite aggressive medical treatment, mortality remains high (20–30%). It may progress to cardiac tamponade and septic shock. Moreover, it may progress to constrictive pericarditis and persistent PP. Constrictive pericarditis is characterized by a thickened, adherent pericardium, which leads to decreased pericardial compliance and ensuing hemodynamic compromise. Pericardial fibrosis is caused by subacute/chronic inflammation, which leads to proliferation of fibroblasts and deposition of collagen. Persistent PP is defined as chronic or recurrent pericardial effusion despite drainage of the fluid and appropriate antibiotic therapy.1,3,4
Pasteurella multocida is a Gram-negative bacteria present in the gastrointestinal tract and nasopharynx of many animals. Approximately 50% to 90% of domestic dogs and cats carry Pasteurella species in their saliva and nasal secretions.6
A review of the literature from the last 30 years revealed that over the years there have been 20 to 30 deaths per year worldwide due to Pasteurella infection. However, this rate seems to be increasing, and in almost all cases death seems to be associated with a complication of infections acquired through animal exposure. Among the Pasteurella species, Pasteurella multocida is the most common, especially in cases that involve severe septic symptoms.7,8
Common symptoms of Pasteurella infections resulting from animal bite in humans include edema, cellulitis or purulent drainage from the skin lacerations. Leukocytosis and neutrophilia are very common, and inflammatory symptoms may quickly progress to fulminant septic symptoms or other severe complications, such as osteomyelitis, endocarditis and meningitis.7,8
Antibiotic treatment generally consists of the combination of amoxicillin and clavulanic acid; doxycycline and metronidazole for patients allergic to penicillin; clindamycin and a fluoroquinolone; or ceftriaxone alone. The relatively low incidence of Pasteurella infection, despite the high prevalence of Pasteurella species in domestic animals, supports the idea that Pasteurella is an opportunistic pathogen for humans. Given the low incidence of human infection (as mentioned above), immunization or vaccination against Pasteurella infection is done through animal disease control.7,8
ConclusionInteraction between humans and domestic animals is unlikely to decrease in the future, and evidence suggests that Pasteurella multocida infection can progress to severe septic cases that involve the heart. The authors stress the importance of promptly diagnosing the complications of this infection. This is particularly true for purulent pericarditis, which if left untreated leads to death.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ferreira R, Martins J, Adrega T, Pinto S, Nunes S, Pancas R, et al. Pericardite purulenta e Pasteurella multocida: uma associação raríssima. Rev Port Cardiol. 2018;37:353.e1–353.e4.