Inflammatory mechanisms are known to play an important role in coronary artery disease. The present study aimed to investigate the importance of the neutrophil-to-lymphocyte ratio (NLR) in terms of in-hospital mortality and its association with currently used risk scores in patients with non-ST-elevation acute coronary syndrome (NSTE-ACS).
MethodsThree hundred and seventeen patients with NSTE-ACS were included. The patients were divided into tertiles according to their NLR values (NLR <2.6, NLR=2.6–4.5, and NLR >4.5). Clinical and angiographic risk was evaluated by the SYNTAX and GRACE risk scores.
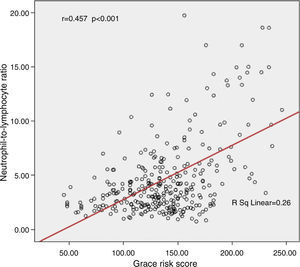
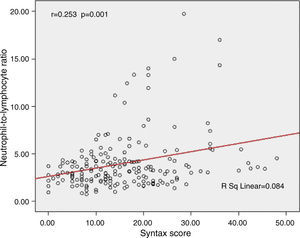
ResultsThe GRACE risk score was significantly higher in the group with high NLR values compared to those with moderate or low NLR (161.5±40.3, 130.5±32.3, and 123.9±34.3, respectively, p<0.001). Similarly, the SYNTAX score was significantly higher in the group with high NLR values (20.4±10.1, 15.5±10.5, and 13.4±7.8, respectively, p=0.003). Moreover, both GRACE (r=0.457, p<0.001) and SYNTAX scores (r=0.253, p=0.001) showed a significant positive correlation with NLR.
ConclusionNLR has been found to be correlated with clinical and angiographic risk scores. Low NLR might be a good predictor for low in-hospital mortality and simple coronary anatomy in NSTE-ACS patients.
Sabe-se que os mecanismos inflamatórios têm um papel importante na doença arterial coronária. O presente estudo visa investigar a importância do rácio neutrófilo/linfócito (RNL) relativamente à mortalidade hospitalar e à sua associação com os scores de risco atuais em doentes com síndromes coronárias agudas sem elevação do segmento-ST (SCA-NSTE).
MétodosForam incluídos 317 doentes com SCA-NSTE. Os doentes foram divididos em tercis de acordo com os seus valores de RNL (RNL < 2,6, RNL = 2,6-4,5 e RNL > 4,5). Os scores de risco clínicos e angiográficos foram avaliados pelos métodos de risco SYNTAX e GRACE.
ResultadosO score de risco GRACE foi significativamente mais elevado no grupo com valores RNL elevados comparado com os grupos com RNL moderado ou baixo (161,5 ± 40,3, 130,5 ± 32,3 e 123,9 ± 34,3, respetivamente, p<0,001). Do mesmo modo, o score SYNTAX foi significativamente superior no grupo com valores RNL elevados (20,4 ± 10,1, 15,5 ± 10,5 e 13,4 ± 7,8, respetivamente, p=0,003). Por outro lado, tanto o score de risco GRACE (r=0,457, p<0,001) como o score SYNTAX (r=0,253, p=0,001) mostraram uma correlação positiva significativa com RNL.
ConclusãoVerificou-se que o RNL está correlacionado com os scores de risco clínicos e angiográficos. Um RNL baixo pode ser um bom fator preditor de mortalidade intra-hospitalar e de anatomia coronária simples em doentes com enfarte do miocárdio sem elevação do segmento ST.
The content and intensity of treatment, and the need for intervention, are closely linked to disease severity in the treatment of patients with coronary artery disease (CAD). Clinical and angiographic risk scores have been developed to aid decision-making. Current guidelines recommend the GRACE and SYNTAX risk scoring systems for patients diagnosed with non-ST-elevation acute coronary syndrome (NSTE-ACS).1,2 The GRACE risk score includes parameters such as ECG changes, initial cardiac markers, and serum creatinine, in addition to clinical characteristics such as age, heart rate, systolic blood pressure, and degree of heart failure.3 The SYNTAX risk score grades the severity and complexity of lesions on coronary angiography.2 It also has an important role in decisions as to whether to perform percutaneous coronary intervention.
Several studies have shown the role of inflammation in the pathophysiology of atherosclerosis,4,5 and inflammatory mediators such as C-reactive protein (CRP) can be used for risk stratification in CAD.4 The neutrophil-to-lymphocyte ratio (NLR) is a new marker recently shown to be effective in CAD and certain non-cardiac diseases. Previous studies have demonstrated that NLR is associated with adverse events in stable coronary disease,6 long-term mortality in patients with ST-segment elevation myocardial infarction (STEMI),7 and in-hospital and six-month mortality in acute coronary syndrome.8 NLR has also been shown to be a predictor of poor prognosis in patients with NSTE-ACS.9 However, the association between NLR and clinical risk scores, and whether it is a determinant of lesion complexity, particularly in CAD, have not been investigated. In the present study, we aimed to investigate the importance of NLR in terms of hospital mortality, and its association with currently used risk scores in patients with NSTE-ACS.
MethodsStudy populationIn this study, patients admitted to the cardiology clinic at Ondokuz Mayis University with NSTE-ACS between January 2006 and January 2012 were retrospectively assessed. The inclusion criterion was the NSTE-ACS diagnosis code in the electronic patient database. The medical history of all patients with the NSTE-ACS diagnosis code was obtained and assessed by the investigators. Exclusion criteria included inconclusive NSTE-ACS diagnosis according to medical records, hematological disease, autoimmune disease, infectious or inflammatory disease, severe renal disease (glomerular filtration rate <30 ml/min/1.73 m2), severe liver disease, and ongoing treatment with immunosuppressive agents.
Definition of non-ST-elevation acute coronary syndromeNSTE-ACS was defined as the presence of T-wave inversion or ST-segment depression and/or positive troponin I in the absence of electrocardiographic (ECG) ST elevation in patients presenting with angina or equivalent. Positive troponin was defined as troponin I >0.1 ng/ml.
Coronary angiographyCoronary angiography was performed using standard techniques. Selective cine angiographic images of the coronaries were recorded with a digital angiographic system (ACOM.PC, Siemens AG, Germany).
Risk scoringFor the SYNTAX score,10 the severity of coronary atherosclerotic lesions was assessed with at least three projections in all patients. The score for each patient was calculated by a team of two experienced cardiologists who scored all coronary lesions with ≥50% stenosis in vessels ≥1.5 mm. The online SYNTAX score calculation tool was used (http://www.SYNTAXscore.com).
The principle of the GRACE risk score has been described elsewhere.3 The variables used in the calculation of the score include age, heart rate, systolic blood pressure, baseline creatinine level, history of congestive heart failure, in-hospital percutaneous coronary intervention, history of myocardial infarction, ST-segment depression on admission electrocardiography (ECG), and elevated cardiac markers. In the present study, we used a single measurement of serum cardiac troponin I, considering 0.06 ng/ml to be an elevated cardiac marker. ST-segment depression was defined as ST segment >0.5 mV below the isoelectric line in any ECG lead.
Laboratory parametersVenous blood samples, obtained from the patients within an hour of admission to the emergency room, were used for the laboratory analyses. Biochemical parameters were measured using an Abbott Architect c8000 analyzer (Abbott Laboratories, USA) with commercial kits. Total blood cell counts and subtypes were analyzed using an automated blood cell counter (Abbott Laboratories, USA). NLR values were calculated as the ratio of neutrophil to lymphocyte count obtained from the same blood sample. Patients were divided into tertiles according to NLR values (NLR <2.6, NLR=2.6–4.5, and NLR >4.5).
Follow-upClinical records of the patients over the course of hospitalization were reviewed and all-cause mortality before hospital discharge was recorded as in-hospital mortality.
Statistical analysisThe dataset was analyzed using SPSS version 15. The normal distribution of the data was tested using the Kolmogorov-Smirnov test and non-normally distributed data were transformed. One-way ANOVA was used for the comparison of multiple groups. Categorical data were compared using the chi-square test or Fisher's exact test, as appropriate. Correlation between data was tested with Pearson's correlation analysis. Logistic regression analysis was used to test the significance of the data on mortality. Variables were eliminated by forward selection. NLR and the GRACE score criteria were selected as the potential variables for logistic regression analysis, excepting cardiac arrest on admission, which was not assessed because there were no patients with this parameter. Continuous data were expressed as mean ± SD (standard deviation) and categorical data were expressed as percentages. A p value of <0.05 was accepted as statistically significant. Bonferroni's correction was performed when statistical comparisons of the three groups were made as <0.016.
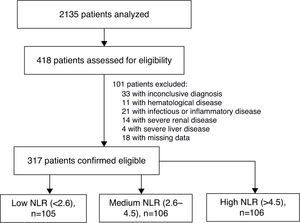
ResultsFor the present study, records were analyzed of 2135 patients admitted to the coronary intensive care unit, of whom 418 patients were admitted with an NSTE-ACS diagnosis code. On the basis of patients’ records, 33 patients with an inconclusive diagnosis, 11 with hematological disease, 21 with infectious and inflammatory disease, 14 with severe renal disease, four with severe liver disease, and 18 with missing data were excluded from the study (Figure 1). As a result, a total of 317 patients were included in the study. Following clinical assessment, 276 (86.8%) patients underwent coronary angiography.
Demographic, clinical, and laboratory characteristics of the patients are presented in Table 1. The patients in the group with high NLR were older and had higher serum glucose levels, lower hemoglobin, lower ejection fraction, higher heart rate, higher Killip class, more ST-segment changes, and higher troponin and creatinine levels.
Baseline characteristics of the study population.
| Low NLR (<2.6), n=105 | Medium NLR (2.6–4.5), n=106 | High NLR (>4.5), n=106 | p | |
|---|---|---|---|---|
| Age, years | 62.8±11.3 | 60.9±13.6c | 67.6±12.5 | <0.001 |
| Gender, male (%) | 76 (72.4) | 78 (73.6) | 83 (79.3) | 0.578 |
| Hypertension (%) | 45 (42.9) | 39 (36.8) | 52 (49.1) | 0.196 |
| Diabetes (%) | 24 (22.9) | 21 (19.8) | 38 (35.8) | 0.019 |
| hs-CRP (mg/l) | 38.9±51.0 | 44.7±60.6 | 80.3±17.9 | 0.423 |
| Serum glucose (mg/dl) | 157.1±89.9 | 143.5±68.7c | 171.0±83.5 | 0.017 |
| Total cholesterol (mg/dl) | 182.8±48.5 | 188.2±41.5 | 169.9±44.6 | 0.027 |
| LDL cholesterol (mg/dl) | 116.9±47.7 | 115.9±33.3 | 104.3±36.2 | 0.075 |
| HDL cholesterol (mg/dl) | 37.6±10.2 | 37.6±9.6 | 36.3±11.7 | 0.287 |
| Triglycerides (mg/dl) | 167.5±104.5 | 170.9±103.6 | 146.5±83.6 | 0.167 |
| Hemoglobin (g/l) | 13.7±1.7b | 13.9±1.7c | 12.7±2.4 | <0.001 |
| Ejection fraction (%) | 55.6±9.0a,b | 49.4±11.6 | 47.5±13.8 | <0.001 |
| Heart rate | 74.9±15.2b | 79.2±16.1c | 86.6±17.9 | <0.001 |
| SBP (mmHg) | 152.3±37.1 | 147.5±31.3 | 141.0±33.6 | 0.059 |
| Killip class | ||||
| I | 99 (94.3) | 96 (90.6) | 66 (62.3) | <0.001 |
| II | 6 (5.7) | 8 (7.5) | 26 (24.5) | <0.001 |
| III | 0 | 1 (0.9) | 13 (12.3) | <0.001 |
| IV | 0 | 1 (0.9) | 1 (0.9) | 0.607 |
| ST-segment deviation | 76 (72.4)a,b | 92 (86.8) | 94 (88.7) | 0.003 |
| Elevated cardiac markers | 80 (76.2) | 90 (84.9) | 95 (89.6) | 0.028 |
| Troponin I (ng/ml) | 10.1±16.9a,b | 19.7±27.9 | 29.2±31.5 | <0.001 |
| Creatinine (mg/dl) | 1.04±0.83b | 1.5±2.5c | 2.05±2.6 | <0.001 |
| GRACE risk score | 123.9±34.3b | 130.5±32.3c | 161.5±40.3 | <0.001 |
| SYNTAX score (n=276) | 13.4±7.8b | 15.5±10.5c | 20.4±10.1 | 0.003 |
| CRP (mg/l) (n=146) | 42.4±63.2 | 51.1±83.7 | 96.8±165.5 | 0.045 |
| NLR | 1.89±0.44a,b | 3.53±0.54c | 8.63±4.39 | <0.001 |
CABG: coronary artery bypass grafting; CRP: C-reactive protein; HDL: high-density lipoprotein; hs-CRP: high-sensitivity C-reactive protein; LDL: low-density lipoprotein; NLR: neutrophil-to-lymphocyte ratio; PCI: percutaneous coronary intervention; SBP: systolic blood pressure.
GRACE risk score was significantly higher in the high NLR group than in those with moderate or low NLR (161.5±40.3, 130.5±32.3 and 123.9±34.3, respectively, p<0.001). Similarly, SYNTAX score was significantly higher in the group with high NLR (20.4±10.1, 15.5±10.5 and 13.4±7.8, respectively, p=0.003). Moreover, both GRACE risk score (r=0.457, p<0.001) and SYNTAX score (r=0.253, p=0.001) showed a significant positive correlation with NLR (Figures 2 and 3). Analysis of the NLR subgroups revealed a correlation between NLR, GRACE and SYNTAX scores only in the high NLR group (r=0.483, p<0.001, and r=0.495, p=0.001, respectively).
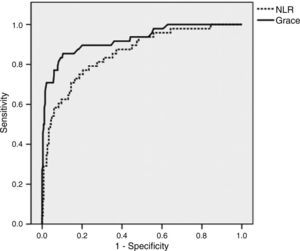
The high NLR group had higher in-hospital mortality than both the low and the moderate NLR groups (35.8%, 7.5% and 1.9%, p<0.001). Receiver operating characteristic (ROC) analysis showed that NLR >4.5 had 75% specificity and 75% sensitivity for in-hospital mortality (Figure 4), with a positive predictive value of 79.2% and a negative predictive value of 95.3% (area under the curve [AUC]=0.857). On the other hand, ROC analysis showed that a GRACE score >140 had 61% specificity and 92.2% sensitivity for in-hospital mortality, with a positive predictive value of 91.6% and a negative predictive value of 97.7% (AUC=0.926). ROC analysis showed that a CRP value of 36.7 had 78.6% specificity and 70.9% sensitivity for in-hospital mortality, with a positive predictive value of 0.79% and a negative predictive value of 96.9% (AUC=0.815). Furthermore, multivariate regression analysis showed that NLR was an independent predictor of in-hospital mortality (OR: 1.182; 95% confidence interval [CI]: 1.042–1.340; p=0.009). Additionally, NLR >4.5 had higher odds ratios for in-hospital mortality (OR: 11.457; 95% CI: 5.415–24.229; p<0.001). Other independent variables were age, Killip class, and troponin I value (Table 2).
Effects of different variables on in-hospital mortality in multivariate logistic regression analysis.
| Variable | Univariate logistic regression | Multivariate logistic regression | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| NLR | 1.183 | 1.030–1.359 | 0.017 | 1.182 | 1.042–1.340 | 0.009 |
| Age (years) | 1.114 | 1.055–1.176 | <0.001 | 1.115 | 1.057–1.175 | <0.001 |
| Heart rate (bpm) | 0.999 | 0.971–1.029 | 0.971 | |||
| SBP (mmHg) | 1.001 | 0.985–1.017 | 0.879 | |||
| Creatinine (mg/dl) | 1.012 | 0.847–1.209 | 0.899 | |||
| Killip class | 29.005 | 9.287–90.587 | <0.001 | 29.794 | 9.871–89.931 | <0.001 |
| Troponin I | 1.018 | 1.001–1.036 | 0.042 | 1.019 | 1.002–1.036 | 0.024 |
| ST-segment deviation | 1.556 | 0.161–15.012 | 0.702 | |||
CI: confidence interval; NLR: neutrophil-to-lymphocyte ratio; OR: odds ratio; SBP: systolic blood pressure.
In this study, we found higher GRACE and SYNTAX risk scores and in-hospital mortality in patients with high NLR values. In addition, NLR correlated with GRACE and SYNTAX scores. The present study is the first to demonstrate an association between coronary artery lesion complexity and NLR in patients with NSTE-ACS.
An association between cardiovascular disease and NLR has been shown in previous studies.6–9 Increased NLR has been found to be associated with increased mortality,11 no-reflow,12 coronary ectasia,13 and coronary collateral circulation14 in various subgroups with CAD. This is an unsurprising result, given the increased inflammatory response seen during the clinical presentation of CAD as well as in its pathophysiology. The role of neutrophils during the atherosclerotic process is well known4; in particular, proteolytic enzymes released by neutrophils and myeloperoxidase activation, as well as acid phosphatase and free oxygen radicals, have been found to be involved in this process.15–17 Furthermore, Sonmez et al. found an association between NLR and coronary artery lesion complexity in patients with stable CAD and STEMI,18 and Oncel et al. demonstrated an association between GRACE score and NLR in patients with STEMI.19 In the present study, we have shown this association in patients with NSTE-ACS.
Neutrophil infiltration during acute coronary events is associated with impaired microvascular perfusion and expansion of the infarct area, as well as with increased risk of no-reflow in primary angioplasty among patients with STEMI,12 and increased NLR has been suggested as a predictor of increased thrombus load.20 Furthermore, acute coronary syndrome (ACS)-associated decreased lymphocyte levels have been reported to suppress immune response, and may be a predictor of mechanical complications,21 as well as being associated with adverse events and cardiac failure in patients with ACS.22,23 In this regard, NLR is associated with increased inflammation as well as inadequate immune response. The present study shows significantly higher in-hospital mortality in the groups with increased NLR. Furthermore, patients with high NLR also suffer from more severely depressed left ventricular function. On ROC analysis, NLR with a threshold of 4.5 has a high positive and negative predictive value. However, the higher negative predictive value is particularly important; considering that NLR is a non-specific marker, low NLR may be interpreted as a good predictor of good prognosis and survival, which may be more useful than the positive role of increased NLR. Sawant et al.24 have shown an association of NLR and CRP with post-revascularization prognosis in patients with ST-elevation ACS.
The GRACE risk score is a scoring method based on criteria also recommended by current guidelines. It is a good indicator of in-hospital and subsequent prognosis.25 Inflammatory markers such as CRP and dickkopf-1 have been associated with GRACE score in patients with ACS.26,27 Also in our study, higher CRP values were observed in the high NLR group. The present study shows that the GRACE risk score has high positive and negative predictive values, and also correlates well with NLR. An earlier study also demonstrated a significant correlation between NLR and GRACE risk score in patients with STEMI.19 The GRACE risk score includes a series of clinical and laboratory criteria, and the comparison of its ROC curve against the ROC curve of NLR indicates that NLR may be a simple and valuable marker of early survival. In the present study, higher specificity was determined for an NLR value of 4.5 as compared to a GRACE risk score of 140. This might be particularly helpful in identifying patients with low GRACE risk score who are likely to have poor prognosis.
The SYNTAX score provides information on the severity of CAD as well as the complexity of lesions. It is thus important in terms of eligibility of patients for percutaneous intervention.28 Altun et al.29 found a significant association between SYNTAX score and NLR in patients presenting with acute MI. Furthermore, Sonmez et al.30 demonstrated a correlation between NLR and SYNTAX score in patients with stable CAD, while Sahin et al.18 showed an association between SYNTAX score and NLR in patients with STEMI. However, the present study is the first to demonstrate an association between NLR and SYNTAX score in isolated patients with NSTE-ACS. This is most likely related to the sensitivity of coronary lesions and myocardial damage. Histopathological studies have shown increased neutrophils in unstable and ruptured plaques,31,32 while increased neutrophils are thought to impair microvascular circulation, leading to infarct expansion after reperfusion.32
In the present study, a strong correlation between NLR with GRACE and SYNTAX scores has been demonstrated, particularly in the high NLR group. Therefore, in addition to the relation of low and moderate NLR values with low morbidity, it may be assumed that a high NLR would be associated with increased morbidity and a higher atherosclerotic plaque burden.
Study limitationsAlthough a total of 2135 patients admitted to the coronary intensive care unit were screened in the present study, only 418 (19.6%) of them were coded with the diagnosis of NST-ACS. Our study demonstrates an association between NLR and in-hospital mortality, though its role in post-discharge survival and other adverse events could not be assessed due to insufficient retrospective data. Furthermore, since there were a limited number of patients with CRP values in our database, CRP could not be included in the multivariate regression analysis.
ConclusionIn our study, NLR, a new marker, was tested in a large group of patients, and increased NLR was associated with short-term survival in patients with NSTE-ACS. In addition, NLR was found to be correlated with clinical and angiographic risk scores. These results support the relation of low NLR with improved short-term survival and of increased NLR with massive atherosclerotic burden and inflammation.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.