A low-risk GRACE score identifies patients with a lower incidence of major cardiac events, however it can erroneously classify patients with severe coronary artery disease as low-risk. We assessed the prevalence, clinical outcomes and predictors of left main and/or three-vessel disease (LM/3VD) in non-ST-elevation acute myocardial infarction (NSTEMI) patients with a GRACE score of ≤108 at admission.
MethodsUsing data from the Portuguese Registry on Acute Coronary Syndromes, 1196 patients with NSTEMI and a GRACE score of ≤108 who underwent coronary angiography were studied. Independent predictors of LM/3VD and its impact on in-hospital complications and one-year mortality were retrospectively analyzed.
ResultsLM/3VD was present in 18.2% of patients. Its prevalence was higher in males and associated with hypertension, diabetes, previous myocardial infarction, heart failure and peripheral arterial disease (PAD). Although there were no differences in in-hospital complications, these patients had higher mortality (0.9 vs. 0.0%) and more major adverse cardiac and cerebrovascular events (MACCE) (4.1 vs. 2.5%, p=0.172), and higher one-year mortality (2.4 vs. 0.5%, p=0.005). Independent predictors of LM/3VD were age (OR 1.03; 95% CI 1.01-1.0, p=0.003), male gender (OR 2.56; 95% CI 1.56-4.17, p<0.001), heart rate (1.02; 95% CI 1.01-1.03, p<0.001), PAD (OR 3.21; 95% CI 1.47-7.00, p<0.001) and heart failure (OR 3.38; 95% CI 1.02-11.15, p=0.046).
ConclusionsLM/3VD was found in one in five patients. These patients had a tendency for higher in-hospital mortality and more MACCE, and higher one-year mortality. Simple clinical variables could help predict this severe coronary anatomy.
Um baixo Score GRACE está associado a menor incidência de eventos cardíacos major porém pode erradamente classificar de baixo risco doentes com doença coronária severa. Pretendeu-se avaliar a prevalência, prognóstico e preditores de doença do tronco comum/três vasos em doentes com enfarte agudo do miocárdio sem elevação do segmento ST e Score GRACE≤108 pontos à admissão.
MétodosUtilizando dados do Registo Nacional de Síndromes Coronárias Agudas, estudámos 1196 doentes com enfarte agudo do miocárdio sem elevação do segmento ST e GRACE≤108 que realizaram coronariografia. Analisados retrospetivamente os preditores independentes de doença do tronco comum e/ou três vasos e o seu impacto prognóstico.
ResultadosDoença do tronco comum e/ou três vasos ocorreu em 18,2%. A prevalência foi superior no género masculino e associou-se a hipertensão, diabetes, enfarte prévio, insuficiência cardíaca e doença arterial periférica. Apesar da ausência de diferenças nas complicações hospitalares, tiveram mais eventos cardiocerebrovasculares major (4,1 versus 2,5%, p=0,172), maior mortalidade hospitalar (0,9 versus 0,0%) e a um ano (2,4 versus 0,5%, p=0,005). Considerados preditores de doença do tronco comum e/ou três vasos: idade (OR 1,03 [1,01-1,05], CI 95%,p=0,003), género masculino (OR 2,56 [1,56-4,17], CI 95%, p<0,001), frequência cardíaca (OR 1,02 [1,01-1,03], CI 95%, p<0,001), doença arterial periférica (OR 3,21 [1,47-7,00], CI 95%, p<0,001) e insuficiência cardíaca (OR 3,38 [1,02-11,15], CI 95%, p=0,046).
ConclusõesDoença do tronco comum e/ou três vasos ocorre em cerca de um em cada cinco doentes. Verificou-se tendência para maior mortalidade hospitalar e eventos cardio-cerebrovasculares major, e maior mortalidade anual. Variáveis clínicas simples podem ajudar a predizer esta anatomia coronária severa.
acute coronary syndrome
coronary artery bypass grafting
coronary artery disease
Global Registry of Acute Coronary Events
left anterior descending artery
left main and/or three-vessel disease
major adverse cardiac and cerebrovascular events
non-ST-elevation acute coronary syndrome
non-ST-elevation myocardial infarction
odds ratio
peripheral arterial disease
Portuguese Registry on Acute Coronary Syndromes
Thrombolysis In Myocardial Infarction
Non-ST-elevation acute coronary syndrome (NSTE-ACS) is a heterogeneous clinical entity in which prospective risk stratification is essential to identify patients at high risk of adverse events1,2 and to offer them, if appropriate, an early invasive strategy to improve short and long-term prognosis.3,4
Current clinical guidelines from the European Society of Cardiology5 and the American Heart Association/American College of Cardiology6 recommend the use of risk scores. Both recommend the use of the Global Registry of Acute Coronary Events (GRACE) score at admission to predict the risk of in-hospital mortality. The GRACE score is derived from eight clinical, electrocardiographic and laboratory variables: five semiquantitative (age, systolic blood pressure, heart rate, Killip class and serum creatinine level) and three dichotomous (cardiac arrest during presentation, ST-segment deviation and elevated cardiac enzymes), and ranges from 1 to 372 points.2 It has good accuracy for predicting in-hospital death in this cohort of patients.
Patients with NSTE-ACS and a GRACE score ≤108 points at admission are classified as low-risk, defined as <1% risk of in-hospital death,2 and as suitable for initially conservative management.5,6 However, risk scores, including GRACE, are not intended to determine the severity of coronary artery disease (CAD) and, if an initial conservative approach is adopted in accordance with the calculated risk, this may result in failure to identify patients with severe CAD requiring revascularization, such as left main and/or three-vessel disease (LM/3VD).7
Several studies have evaluated the performance of clinical risk scores for detecting and predicting the severity of CAD.
In patients with NSTE-ACS, the TIMI risk score has a modest ability to predict obstructive CAD, defined as the presence of at least one ≥50% stenosis,8,9 while a TIMI score >4 shows a modest10 to good11 performance in detecting three-vessel CAD. In one study, sensitivity of 53% and specificity of 83% were demonstrated for this diagnosis (area under the curve [AUC] 0.71; 95% CI 0.61-0.81, p<0.001).11
Variability in accuracy for prediction of CAD using the GRACE score is greater due to the different cut-off points studied. Its performance is good for the detection of multivessel disease (AUC 0.72; 95% CI 0.64-0.80, p=0.001)12 but only modest for three-vessel disease with a cut-off of >11911 or LM/3VD with a cut-off of >117.13 The GRACE score has better predictive ability for three-vessel disease when the cut-off is >133,10 and higher sensitivity but lower specificity than the TIMI risk score.11
This study aimed to determine the prevalence of LM/3VD in non-ST-elevation myocardial infarction (NSTEMI) patients with a GRACE score ≤108 at admission, to assess its impact on clinical outcomes, and to determine its predictors.
MethodsStudy design, population and variablesThis was a retrospective study based on the data of the second phase of the Portuguese Registry on Acute Coronary Syndromes (ProACS). Details of the study design, outcome definitions, patients, and main results of the first phase have been published.14,15 Data are collected from all participating centers in Portugal and entered in a web-based platform at discharge and at one-year follow-up. Information is recorded on demographics, cardiovascular risk factors, clinical presentation, laboratory and imaging results, coronary angiography and revascularization, medication and in-hospital adverse events (reinfarction, congestive heart failure, cardiogenic shock, atrial fibrillation, advanced atrioventricular block, resuscitated cardiac arrest, stroke, major bleeding and death).
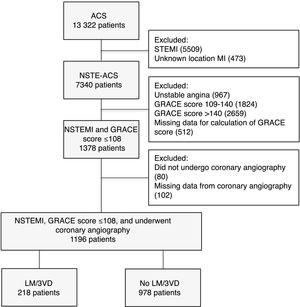
Between October 1, 2010 and November 4, 2015, a total of 13322 patients with a diagnosis of acute coronary syndrome (ACS) were included in the ProACS. After exclusion of patients with STEMI, unknown location myocardial infarction, unstable angina or GRACE score >109, or missing data for calculation of the GRACE score, 1378 had a diagnosis of NSTEMI and a GRACE score ≤108 at admission, of whom only the 1196 patients who had undergone coronary angiography were included. Detailed information on the study selection process is shown in Figure 1.
Flowchart of patient selection. ACS: acute coronary syndrome; GRACE: Global Registry of Acute Coronary Events; LM/3VD: left main and/or three-vessel disease; MI: myocardial infarction; NSTE-ACS: non-ST-segment elevation acute coronary syndrome; NSTEMI: non-ST-segment elevation acute myocardial infarction; STEMI: ST-segment elevation myocardial infarction.
The total proportion of missing data on baseline characteristics was low (3.7% of the total variables) and all the patients and information on their baseline characteristics were included.
CAD was defined as the presence of a ≥50% stenosis in any major vessel (left main, left anterior descending [LAD], left circumflex or right coronary artery).
For the purpose of this study, the patients were divided in two groups: the LM/3VD group (patients with angiographic evidence of LM/3VD) and the non-LM/3VD group (all other patients).
The primary endpoint was defined as major adverse cardiac and cerebrovascular events (MACCE) (in-hospital mortality, reinfarction, non-fatal stroke or heart failure) and the secondary endpoint as the need for coronary artery bypass grafting (CABG) during hospitalization.
Statistical analysisBaseline characteristics were compared between patient groups using the Student's t test for continuous variables and the chi-square test or Fisher's exact test for categorical variables. Continuous variables were expressed as mean ± standard deviation or median and interquartile range (IQR). Categorical variables were expressed as absolute or relative frequencies.
Multivariate logistic regression analysis was performed to assess independent predictors of LM/3VD in this population and its influence on in-hospital mortality or MACCE. The variables included were age; gender; admission creatinine, heart rate, blood pressure and Killip class; cardiovascular risk factors; previous medical history (excluding previous CABG); ST-segment deviation or T-wave inversion; and left ventricular function. Odds ratios (OR) and hazard ratios were calculated with 95% confidence intervals (CI). The logistic regression included only patients without missing data regarding the main variables (1098 out of 1196 patients, 91.8%).
Survival at one-year follow-up, describing cumulative mortality since admission, was analyzed using Kaplan-Meier curves with the log-rank test. Multivariate Cox regression was performed. The number of patients with complete one-year follow-up was 528 (44.1%).
IBM SPSS Statistics® version 19.0 was used for the statistical analysis and a two-tailed p-value of <0.05 was considered statistically significant.
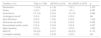
ResultsBaseline characteristicsIn this cohort of patients with NSTEMI and GRACE score ≤108 at admission, the incidence of LM/3VD was 18.2% (n=218). The baseline and admission characteristics of the study population are summarized in Table 1, which also shows univariate associations with the presence of LM/3VD.
Baseline and admission characteristics of the study population.
| Variable | Total | LM/3VD | No LM/3VD | p |
|---|---|---|---|---|
| Mean age, years (n) | 54±9 (1196) | 56±8 (218) | 53±9 (978) | <0.001 |
| Male, % (n) | 81.5 (975/1196) | 88.5 (193/218) | 80.0 (782/978) | 0.003 |
| BMI, kg/m2(n) | 28.1±4.4 (1094) | 28.2±4.0% (203) | 28.1±4.5% (891) | 0.749 |
| Smoking, % (n) | 46.6 (557/1196) | 45.0 (98/218) | 46.9 (459/987) | 0.596 |
| Hypertension, % (n) | 59.0 (691/1171) | 69.8 (150/215) | 56.6 (541/956) | <0.001 |
| Diabetes, % (n) | 21.2 (249/1173) | 30.0 (64/213) | 19.3 (185/960) | <0.001 |
| Dyslipidemia, % (n) | 56.6 (643/1137) | 62.6 (129/206) | 55.2 (514/931) | 0.052 |
| Previous MI, % (n) | 16.9 (201/1191) | 24.9 (54/217) | 15.1(147/974) | <0.001 |
| Previous PCI, % (n) | 13.2 (158/1193) | 17.1 (37/217) | 12.4 (121/976) | 0.067 |
| Previous CABG, % (n) | 2.3 (27/1195) | 9.6 (21/218) | 0.6 (6/977) | <0.001 |
| Previous renal failure, % (n) | 1.0 (12/1192) | 1.4 (3/218) | 0.9 (9/974) | 0.468 |
| Previous PAD, % (n) | 2.9 (34/1188) | 7.9 (17/216) | 1.7 (17/972) | <0.001 |
| Previous stroke, % (n) | 3.9 (47/1194) | 4.1 (9/217) | 3.9 (38/977) | 0.860 |
| Previous heart failure, % (n) | 1.3 (15/1194) | 3.2 (7/218) | 0.8 (8/976) | 0.011 |
| GRACE score at admission (n) | 90.3±13.1 (1196) | 92.0±12.4 (218) | 89.9±13.3 (978) | 0.024 |
| Patient presentation | ||||
| Chest pain, % (n) | 97.7 (1168/1196) | 96.3 (210/218) | 98.0 (958/978) | 0.151 |
| Syncope, % (n) | 0.8 (10/1196) | 2.3 (5/218) | 0.5 (5/978) | 0.022 |
| Mean HR, bpm (n) | 73±14 (1196) | 76±15 (218) | 73±14 (978) | 0.005 |
| Mean SBP, mmHg (n) | 151±29 (1196) | 154±29 (218) | 150±28 (978) | 0.035 |
| Killip II-IV, % (n) | 0.5 (6/1196) | 0.5 (1/218) | 0.5 (5/978) | 1.000 |
| ECG | ||||
| Normal, % (n) | 49.7 (594/1196) | 48.2 (105/218) | 50.0 (189/978) | 0.624 |
| T-wave inversion, % (n) | 34.9 (417/1196) | 36.7 (80/218) | 34.5 (337/978) | 0.530 |
| ST-segment deviation, % (n) | 1.8 (22/1196) | 2.3 (5/218) | 1.7 (17/978) | 0.577 |
| Serum creatinine, median mg/dl (n) | 0.8 [IQR 0.7;1] (1196/1196) | 0.8 [IQR 0.7;1] (218/218) | 0.8 [IQR 0.7;1] (978/987) | 0.477 |
| LVEF <50%, % (n) | 17.2 (197/1148) | 21.3 (44/207) | 16.3 (153/941) | 0.084 |
| Medication during hospitalization, % (n) | ||||
| Aspirin | 99.2 (1185/1194) | 99.1 (215/217) | 99.3 (970/977) | 0.671 |
| Clopidogrel | 92.1 (1099/1193) | 92.7 (202/218) | 92.0 (897/975) | 0.743 |
| Enoxaparin | 67.8 (809/1194) | 70.2 (153/218) | 67.2 (656/976) | 0.396 |
| ACEI or ARB | 88.3 (1052/1192) | 90.8 (198/218) | 87.7 (854/974) | 0.192 |
| Statin | 97.0 (1158/1194) | 95.9 (209/218) | 97.2 (949/976) | 0.288 |
| Beta-blocker | 87.7 (1045/1192) | 91.7 (200/218) | 86.8 (845/974) | 0.043 |
ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; BMI: body mass index; BP: blood pressure; CABG: coronary artery bypass grafting; ECG: electrocardiogram; GRACE score: Global Registry of Acute Coronary Events; HR: heart rate; IQR: interquartile range; LM/3VD: left main and/or three-vessel disease; LVEF: left ventricular ejection fraction; MI: myocardial infarction; PAD: peripheral arterial disease; PCI: percutaneous coronary intervention; SBP: systolic blood pressure.
Patients in the LM/3VD group were slightly older and more frequently male, and had a slightly higher GRACE score and higher prevalences of hypertension, diabetes and previous myocardial infarction, heart failure and peripheral arterial disease (PAD). Although the main presenting symptom was chest pain in both groups, interestingly there was a higher proportion of patients presenting atypically with syncope in the LM/3VD group. There were no differences between groups regarding electrocardiographic data, left ventricular function or serum creatinine.
Coronary angiography and revascularization dataMost patients underwent coronary angiography within 24 hours of admission; median time from admission to coronary angiography was 0 days (IQR 0-1 days). The prevalence of left main disease was 26.5% and that of three-vessel disease was 89.9% in the LM/3VD group, whereas patients in the non-LM/3VD group were more frequently diagnosed with single-vessel disease (55.6%). Patients with LM/3VD were more likely to have an unidentified culprit artery, to undergo two or more coronary angiographies, and to have a higher rate of femoral access but a lower probability of undergoing angioplasty. They were also more frequently planned for CABG. The results are summarized in Table 2.
Coronary angiography, revascularization and secondary endpoint of the study population.
| Variable | Total, % (n) | LM/3VD, % (n) | No LM/3VD, % (n) | p |
|---|---|---|---|---|
| ≥1 coronary angiographies | 5.8 (68/1177) | 26/215 (12.1) | 42/962 (4.4) | <0.001 |
| Femoral access | 197/1174 (16.8) | 61/214 (28.5) | 136/960 (14.2) | <0.001 |
| Diseased vesselsa | ||||
| None | 152/1177 (12.9) | 0/199 (0.0) | 152/978 (15.5) | NA |
| 1 | 544/1177 (46.2) | 0/199 (0.0) | 544/978 (55.6) | NA |
| 2 | 302/1177 (25.7) | 20/199 (10.1) | 282/978 (28.8) | <0.001 |
| 3 | 179/1177 (15.2) | 179/199 (89.9) | 0/978 (0.0) | NA |
| LM (isolated or not) | 53/1178 (4.5) | 53/200 (26.5) | 0/978 (0.0) | NA |
| Culprit artery | ||||
| LM | 1.7 (17/985) | 8.1 (16/198) | 0.1 (1/787) | <0.001 |
| LAD | 32.7 (322/985) | 16.7 (33/198) | 36.7 (289/787) | <0.001 |
| LCx | 24.6 (242/985) | 12.6 (25/198) | 27.6 (217/787) | <0.001 |
| RCA | 209/985 (21.2) | 33/198 (16.7) | 176/787 (22.4) | 0.080 |
| Graft | 0.4 (4/985) | 2.0 (4/198) | 0.0 (0/787) | NA |
| Unidentified | 19.4 (191/985) | 43.9 (87/198) | 13.2 (104/787) | <0.001 |
| Angioplasty performed | 65.9 (788/1195) | 52.8 (115/218) | 68.9 (673/977) | <0.001 |
| CABG | ||||
| Urgent/secondary endpoint | 1.0 (12/1196) | 4.1 (9/218) | 3/978 (0.3) | <0.001 |
| Planned after transfer | 77/1196 (6.4) | 53/218 (24.3) | 2.5 (24/978) | <0.001 |
| Planned after discharge | 2.7 (32/1196) | 8.3 (18/218) | 1.4 (14/987) | <0.001 |
| Planned and performed | 10.1 (121/1196) | 36.7 (80/218) | 4.2 (41/978) | <0.001 |
CABG: coronary artery bypass grafting; LAD: left anterior descending artery; LCx: left circumflex artery; LM: left main; LM/3VD: left main and/or three-vessel disease; NA: not applicable; RCA: right coronary artery.
Patients with missing data were excluded. Patients for whom not all registry fields for the presence of >50% stenosis were completed could not be stratified by number of diseased vessels. Therefore they were not considered in this analysis, such as a patient with LM and LAD stenosis but no information regarding the RCA or LCx.
The presence of LM/3VD was not associated with a statistically significant difference in in-hospital adverse events, but there was a trend towards higher absolute values of in-hospital mortality and the primary endpoint of MACCE (Table 3). LM/3VD was also associated with increased length of hospital stay (median five vs. three days, p<0.001) and with more frequent need for CABG during hospitalization (4.1 vs. 0.3%, p<0.001). After multivariate regression analysis, the presence of LM/3VD was not found to be an independent predictor of in-hospital MACCE (OR 1.32, 95% CI 0.56-3.14, p=0.526), however it was an independent predictor of the secondary endpoint (OR 13.22, 95% CI 3.34-52.30, p<0.001).
In-hospital adverse events and in-hospital mortality.
| Variable, n (%) | Total (n=1196) | LM/3VD (n=218) | No LM/3VD (n=978) | p |
|---|---|---|---|---|
| Reinfarction | 11 (0.9) | 4 (1.8) | 7 (0.7) | 0.123 |
| Stroke | 3 (0.3) | 2 (0.9) | 1 (0.1) | 0.087 |
| Heart failure | 21 (1.8) | 5 (2.3) | 16 (1.6) | 0.566 |
| Cardiogenic shocka | 2 (0.2) | 2 (0.9) | 0 (0.0) | NA |
| Atrial fibrillation | 6 (0.5) | 1 (0.5) | 5 (0.5) | 1.000 |
| Atrioventricular block | 9 (0.8) | 4 (1.8) | 5 (0.5) | 0.063 |
| Resuscitated cardiac arrest | 5 (0.4) | 2 (0.9) | 3 (0.3) | 0.227 |
| Major bleeding | 6 (0.5) | 1 (0.5) | 5 (0.5) | 1.000 |
| MACCE | 33 (2.8) | 9 (4.1) | 24 (2.5) | 0.172 |
| In-hospital mortality | 2 (0.2) | 2 (0.9) | 0 (0.0) | NA |
LM/3VD: left main and/or three-vessel disease; MACCE: major adverse cerebrovascular events (defined as in-hospital mortality, non-fatal stroke, reinfarction or heart failure); NA: not applicable.
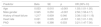
Patients in the LM/3VD group had higher one-year mortality (2.4 vs. 0.5%, p=0.005) but, after multivariate Cox regression analysis, the presence of this coronary anatomy did not confer an increased risk of one-year mortality. The results are displayed in Table 4.
Multivariate Cox regression assessing hazard ratios for one-year mortality.
| Variable | Beta | SE | p | HR (95% CI) |
|---|---|---|---|---|
| LM/3VD | 0.757 | 0.748 | 0.312 | 2.13 (0.49-9.24) |
| Inotropes during hospitalization | 4.213 | 1.287 | 0.001 | 67.55 (5.42-841) |
| Nitrates at discharge | 2.094 | 0.748 | 0.005 | 8.12 (1.88-35.17) |
CI: confidence interval; HR: hazard ratio; LM/3VD: left main and/or three-vessel disease; SE: standard error.
The results are summarized in Table 5. Older age, male gender, higher resting heart rate, previous diagnosis of heart failure and PAD were identified as independent predictors of the presence of LM/3VD. The risk was higher for each 10-bpm increase in heart rate (OR 1.23, 95% CI 1.12-1.36, p<0.001) and for each 10-year increase in age (OR 1.39, 95% CI 1.14-1.69, p<0.001).
Multivariate logistic regression assessing predictors of left main and/or three-vessel disease in patients with non-ST-elevation myocardial infarction and low-risk GRACE score.
| Predictor | Beta | SE | p | OR (95% CI) |
|---|---|---|---|---|
| Age | 0.033 | 0.010 | <0.001 | 1.03 (1.01-1.05) |
| Male gender | 0.945 | 0.250 | <0.001 | 2.56 (1.56-4.17) |
| History of heart failure | 1.217 | 0.609 | 0.046 | 3.38 (1.02-11.15) |
| Heart rate | 0.021 | 0.005 | <0.001 | 1.02 (1.01-1.03) |
| PAD | 1.166 | 0.398 | 0.003 | 3.21 (1.47-7.00) |
CI: confidence interval; OR: odds ratio; PAD: peripheral arterial disease; SE: standard error.
The major findings of this study are that patients admitted with NSTEMI and a low-risk GRACE score (≤108) have a low risk of in-hospital adverse events despite almost one fifth of them having high-risk coronary anatomy, but that these patients had not only a worse long-term prognosis, with higher one-year mortality, but also higher in-hospital morbidity, as shown by increased length of hospital stay, and a trend for higher absolute values of mortality and MACCE. The findings indicate that these patients are not in fact at such low risk and should be identified promptly.
Another important finding was that simple clinical variables appeared as independent predictors of LM/3VD in this population: two of them included in the GRACE score (age and heart rate), male gender, and important known comorbidities (heart failure and PAD).
The relationship between the GRACE risk score and the severity and complexity of CAD has been studied in several publications,8–13,16,17 however very few stratified patients within the three GRACE risk categories and, to our knowledge, none analyzed predictors of LM/3VD disease in low-risk patients.
In the largest study, Beigel et al.16 assessed 923 consecutive patients with moderate-high risk NSTE-ACS enrolled in the Acute Coronary Syndrome Israeli Survey and found that the major predictors of high-risk coronary anatomy (defined as >50% stenosis in the left main, >70% in the proximal LAD and/or two- or three-vessel disease involving the LAD) were GRACE score >140 (high-risk) (OR 1.88, 95% CI 1.29-2.75, p<0.001), PAD (OR 1.88, 95% CI 1.62-5.8, p<0.001) and chronic renal failure (OR 1.7, 95% CI 1.02-2.80, p=0.03). Likewise, Mahmood et al. found that patients with a GRACE score >133 had a higher likelihood of LM/3VD (OR 3.41, 95% CI 2.16-5.36, p<0.01).10 Other groups have set out to correlate the severity of CAD in NSTE-ACS patients with their GRACE score. GRACE >119 had only moderate accuracy for prediction of three-vessel disease, with sensitivity of 80% and specificity of 55% (AUC 0.68; 95% CI 0.58-0.78, p=0.001),11 while GRACE >117 had modest accuracy for predicting LM/3VD, with sensitivity of 66% and specificity of 59% (AUC 0.66; 95% CI 0.58-0.74, p=0.01).13
By contrast, in a study by Barbosa et al.8 the GRACE score was unable to identify the presence of LM/3VD (AUC 0.59; 95% CI 0.48-0.70, p=0.13), and there were no statistical differences between the three GRACE tertiles regarding the prevalence of LM/3VD (25%, 33% and 37%, respectively; p=0.56). Santos et al.9 also showed that the GRACE score had only moderate predictive ability even for the presence of at least one-vessel disease (AUC 0.62; 95% CI 0.573-0.673, p<0.001).
Two studies assessed the severity of CAD according to the number of diseased vessels stratified by GRACE risk categories. In the study by Cakar et al.,12 356 patients with NSTE-ACS were analyzed retrospectively, 39.6% of them with a low-risk GRACE score. The prevalence of LM/3VD was 15.5%, with no in-hospital mortality and a low rate of reinfarction or revascularization (2.1%). These findings were similar to our study. However, they did not assess potential predictors of severe CAD in this population. In a retrospective study of 95 patients with NSTE-ACS, another group reported that 40% of the population had a low-risk GRACE score, with a prevalence of 39.4% for three-vessel disease and 5.2% for left main disease.17 No report on outcomes was available.
Our search of the literature revealed no studies regarding determination of predictors of LM/3VD in low-risk GRACE populations.
Many simple predictors of worse prognosis are correlated with severe CAD. Clinical variables like increasing age and high resting heart rate are well-known risk factors.18 Both these variables are features of the GRACE score and in our study were also found to be predictors of LM/3VD, which is in line with the literature.19 This could mean that, even for low-risk patients, extra care should be taken regarding tachycardic and elderly patients.
PAD is associated with increased risk for cardiovascular death20 and higher in-hospital mortality in ACS,21 and there are several reports associating its presence with greater severity and complexity of CAD.19,22 In our study, despite the low prevalence of PAD in both groups, which was significantly less than in modern cohorts of ACS patients,23 it was an independent predictor of LM/3VD, as it also was in the study by Beigel et al.16 and in a meta-analysis.19 An ankle-brachial index of <0.9 is known to be a predictor of PAD24 and of multivessel CAD in patients admitted with ACS,25 so this simple measure from the physical examination could potentially improve detection of this important comorbidity.
In heart failure, long-term prognosis is directly related to the angiographic extent and severity of CAD,26,27 in patients with both reduced and preserved systolic function.28 In the setting of ACS, development of acute heart failure is considered a powerful predictor of LM/3VD,19 but less is known about the predictive ability of a previous history of chronic heart failure. However, in our study neither the proportion of patients in Killip class II-IV nor the incidence of new-onset heart failure during hospitalization differed between the groups. There were also no differences in the incidence of left ventricular dysfunction. These findings are not surprising, since the population only included patients with a low-risk GRACE score, which means that most patients would be in Killip class I. Another finding is that a previous history of heart failure was an independent predictor of LM/3VD. Nonetheless, this result should be interpreted with caution, since it reached only a borderline significant p-value and the number of patients affected was low.
We also found that male gender was an independent predictor for the presence of LM/3VD, which is in line with other studies that show that men with myocardial infarction have more severe CAD.29–32
In our study, there were no differences between groups in in-hospital adverse events. Although patients with LM/3VD had non-significantly more MACCE and higher in-hospital mortality, the rates were low, as would be accurately predicted by the GRACE score.2 However, a significant interaction was found with the secondary endpoint of urgent referral for CABG during hospitalization, which was more frequent in the LM/3VD group. Indeed, one reason for the need to be able to predict severe CAD using clinical risk scores is to improve assessment of patients who would most likely be indicated for CABG. This is important because it could have therapeutic implications for the timing and duration of dual antiplatelet therapy.
Study limitationsThis was a retrospective study with all the limitations of this type of study design, however it also reflects the real-world population of patients that clinicians see in daily practice. Another important issue is the definition of CAD used. Many authors agree that CAD should be defined as the presence of >50% luminal stenosis, the cut-off used in this study due to the ProACS design. However, from a physiological standpoint, only >70% stenoses are considered hemodynamically significant and requiring revascularization. This may have led to the inclusion of less severe patients in the LM/3VD group, which could have influenced in-hospital outcomes. Another major limitation is the small number of patients who underwent CABG during hospitalization, and therefore the results should be interpreted with caution. Also, we do not know if post-hospitalization CABG contributed to higher mortality in the LM/3VD group. Nevertheless, even though CABG could have played a role in one-year mortality, it would have been performed as a consequence of having LM/3VD, and thus higher mortality could be attributed, at least in part, to the disease itself.
ConclusionPatients admitted for NSTEMI with a low-risk GRACE score of ≤108 at admission had few in-hospital adverse events and low mortality, even though almost one in five had LM/3VD. Nonetheless, despite this apparently good in-hospital prognosis for hard clinical endpoints, these patients had higher absolute values of in-hospital mortality and MACCE, and LM/3VD was associated with longer hospital stay and higher one-year mortality, and was also an independent predictor for CABG during hospitalization. Simple clinical variables are independent predictors of this high-risk coronary anatomy, like older age, higher resting heart rate, male gender, previous diagnosis of heart failure and PAD, and could help the clinician to identify patients who would benefit from an early invasive strategy.
Conflicts of interestThe authors have no conflicts of interest to declare.






 ACS: acute coronary syndrome;
ACS: acute coronary syndrome; 

