To characterize specific knowledge on cardiovascular disease, particularly stroke and myocardial infarction (MI), and its relationship with sociodemographic factors, health literacy and clinical history, among the Portuguese population.
MethodsIn a cross-sectional study conducted in 2012, a total of 1624 Portuguese-speaking residents of mainland Portugal, aged between 16 and 79 years, were assessed through face-to-face interviews using a structured questionnaire.
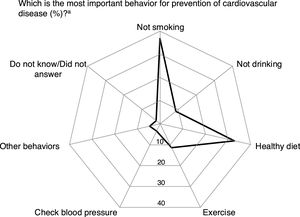
ResultsAround 30% of participants were unable to estimate the risk of MI or stroke. On average, those who responded estimated that 34.2% and 35.6% of Portuguese will suffer a stroke or MI, respectively, during their lifetime. “Not smoking” (36.8%) and a “healthy diet” (32.8%) were identified as the most important behaviors for prevention of cardiovascular disease, and less than half of the participants responded that the most appropriate option in the presence of acute cardiovascular signs or symptoms was to call the emergency number. “Dependence on daily activities” (90.7%) and “impaired speech” (89.8%) were frequently recognized as consequences of stroke, while “heart failure” (86.4%) and “dependence on daily activities” (85.3%) were the most frequently identified consequences of MI. Overall, participants with adequate health literacy revealed more appropriate cardiovascular health-related knowledge.
ConclusionsThere are important gaps in cardiovascular health-related knowledge in the Portuguese population. Health education strategies and practices should be sensitive to the differences in health literacy described herein, in order to improve cardiovascular health knowledge among the Portuguese population.
Caracterizar o conhecimento específico sobre a doença cardiovascular (DCV), nomeadamente o acidente vascular cerebral (AVC) e o enfarte agudo do miocárdio (EAM), da população portuguesa, de acordo com fatores sociodemográficos, literacia em saúde e história clínica.
MétodosNum estudo transversal realizado em 2012, foram avaliados 1624 residentes em Portugal continental, entre 16 e 79 anos, através de entrevistas presenciais com questionário estruturado.
ResultadosCerca de 30% dos participantes não conseguiram estimar o risco de AVC e EAM. Em média, os que responderam estimaram que 34,2% e 35,6% dos portugueses sofrerão um AVC ou um EAM durante a sua vida, respetivamente. «Não fumar» (36,8%) e uma «dieta saudável» (32,8%) foram identificados como os comportamentos mais importantes para prevenção da DCV e menos de metade dos participantes respondeu «telefonar para o 112» como opção correta perante a presença de sinais ou sintomas de eventos cardiovasculares agudos. A «dependência nas atividades diárias» (90,7%) e as «perturbações da fala» (89,8%) foram frequentemente reconhecidas como consequências de AVC, enquanto a «insuficiência cardíaca» (86,4%) e «dependência nas atividades diárias» (85,3%) foram as consequências de EAM identificadas com maior frequência. Em geral, participantes com literacia em saúde adequada revelaram um conhecimento em saúde cardiovascular mais apropriado.
ConclusõesVerificaram-se importantes lacunas no conhecimento específico sobre a doença cardiovascular da população portuguesa. As estratégias e práticas de educação em saúde devem ser sensíveis às diferenças descritas de acordo com o nível de literacia em saúde, de forma a melhorar o conhecimento em saúde cardiovascular da população portuguesa.
Cardiovascular disease (CVD) is the main cause of death worldwide and is projected to remain among the most important contributors to mortality up to 2030.1 Worldwide, approximately 17.3 million people died from CVD in 2013, representing nearly one-third of the overall number of deaths and 45% of those due to non-communicable diseases.2 Among these, 8.1 million deaths were due to coronary heart disease (CHD) and 6.4 million to stroke, which constitute the leading and third leading causes of disability worldwide, respectively.2 In Europe, CVD is responsible for 45% of all deaths each year, with 2.8 million deaths attributed to CHD and stroke.3 In Portugal, CVD is the main cause of mortality, with stroke and CHD accounting for 6.1% and 6.0%, respectively, of total disability-adjusted life years in 2015.4
Despite the high burden of CVD, there has been a considerable decline in mortality in recent decades.5 These reflect downward trends in exposure to behavioral risk factors such as smoking, as well as increasing use of evidence-based pharmacological treatments for control of hypertension and cholesterol levels, and interventional therapies and techniques for better management of patients in the acute phase.6–9 However, patterns of variation in mortality are heterogeneous,5 with many countries, including Portugal, still presenting considerable potential for further decreases in morbidity and mortality from stroke and CHD,5,10 through both ‘high-risk’ and ‘population’ strategies.11
Behaviors that increase the risk of CVD are modulated by individuals’ health-related knowledge and risk perception,12 and therefore understanding limitations in specific knowledge is essential to develop strategies aimed at the empowerment of the population for self-care and better use of available health resources.13,14
We therefore aimed to characterize specific knowledge on the frequency, prevention, control and consequences of cardiovascular disease, particularly stroke and myocardial infarction (MI), and its relationship with sociodemographic factors, history of CVD and health literacy, among the Portuguese population.
MethodsThis analysis is based on a cross-sectional study conducted between January and May 2012, with the primary objective of assessing knowledge and health behaviors in a representative sample of Portuguese-speaking residents of mainland Portugal, aged between 16 and 79 years, as previously described in detail.15 Briefly, a stratified probabilistic sampling procedure was used to select 150 geographical units, among which a total of 585 starting points were designated for the selection of households through standard random route procedures. In each selected household, the resident whose previous birthday was closest to the date of the interview was invited to participate. A total of 1624 valid interviews were obtained (response rate: 70.8%).
Face-to-face interviews were conducted to collect data on sociodemographic characteristics, clinical history, health literacy and specific knowledge on the frequency, prevention, control and consequences of CVD.
A personal history of hypertension, stroke or MI was considered present when participants recalled a medical diagnosis of these conditions.
To assess the perceived risk of stroke and MI, participants were asked “For every 100 Portuguese, how many will suffer from stroke and how many will suffer from MI during their lives?” and the quantitative estimates were used as continuous variables in data analysis.
Regarding behaviors for CVD prevention, participants were asked to select the most important from a list of different behaviors, namely “not smoking”, “not drinking”, “healthy diet”, “regular exercise”, “regular blood pressure measurement”, and “other behaviors”, which included the intake of multivitamins, regular weighing, regular blood tests and general check-ups. The proportion of participants identifying each behavior as the most important was presented.
Awareness of the most appropriate action in the presence of an alarm sign or symptom of a potential cardiovascular event was obtained through the question “In the presence of each of the following symptoms or signs (chest pain or facial drooping) state how to proceed”. The options were “call emergency number”, “go to emergency department”, “call Saúde 24 (the national health helpline)”, “schedule an appointment with physician”, “go to pharmacy” and “take a ‘wait and see’ approach”. Only the option “call emergency number” was considered correct.
To assess knowledge on the potential consequences of CVD, participants were asked to indicate whether each of five options – “paralysis”, “dependence in daily activities”, “impaired speech”, “dementia” and “epilepsy” – could result from stroke. Similarly, participants were also asked to state whether each of five options – “angina pectoris”, “heart failure”, “impaired driving”, “impaired sexual activity” and “dependence in daily activities” – could result from MI. In both questions, the possible answers were “yes”, “no”, “do not know” and “did not answer” for each response category and for data analysis the latter two options were recoded as “no”.
Health literacy was assessed using the Newest Vital Sign (NVS) instrument.16 This tool was designed to assess health literacy skills, specifically reading and numeracy skills. The number of correct answers was used to compute a score ranging from 0 to 6 (0-1: high likelihood of limited literacy [HLLL], 2-3: possibility of limited literacy and 4-6: adequate literacy [AL]). Participants who reported that they were unable to read or write were classified as having HLLL.
Statistical analyses were performed using STATA 11.1 (College Station, TX, 2009). Adjusted mean differences in the estimated number of people affected by stroke and MI, according to sociodemographic characteristics, health literacy and history of CVD (hypertension, stroke and MI), with respective 95% confidence intervals (95%CIs), were computed by multiple linear regression. To estimate the associations between explanatory factors and health-related knowledge variables, adjusted prevalence ratios (PRs) and 95% CIs were computed using Poisson regression. All models were adjusted for age, gender, educational level and health literacy. The product of design and population weights was used for weighting in all analyses.
The survey was approved by the Ethics Committee of the University of Porto.
ResultsParticipants in our sample were evenly distributed in terms of gender. More than 60% were less than 50 years of age, 42.5% had less than five years of schooling and 45.9% presented HLLL (Table 1). A previous diagnosis of hypertension was reported by 14.1% of participants, and 2.8% reported prior stroke or MI (1.8% for stroke and 1.8% for MI).
Characteristics of study participants.
| n | Unweighted (%) | Weighted (%) | |
|---|---|---|---|
| Overall | 1624 | - | - |
| Gender | |||
| Female | 998 | 61.4 | 50.3 |
| Male | 626 | 38.6 | 49.7 |
| Age, years | |||
| <30 | 233 | 14.4 | 27.7 |
| 30-39 | 224 | 13.8 | 16.6 |
| 40-49 | 236 | 14.5 | 19.1 |
| 50-59 | 283 | 17.4 | 14.4 |
| 60-69 | 358 | 22.0 | 12.9 |
| 70-79 | 290 | 17.9 | 9.3 |
| Education, years | |||
| 0-4 | 793 | 48.9 | 42.5 |
| 5-9 | 301 | 18.6 | 18.4 |
| 10-12 | 313 | 19.3 | 25.2 |
| >12 | 216 | 13.3 | 13.9 |
| Health literacy (NVS) | |||
| HLLL | 786 | 48.4 | 45.9 |
| PLL | 471 | 29.0 | 28.6 |
| AL | 367 | 22.6 | 25.5 |
| Hypertension | |||
| No | 1330 | 81.9 | 85.9 |
| Yes | 294 | 18.1 | 14.1 |
| Previous stroke | |||
| No | 1589 | 97.8 | 98.2 |
| Yes | 35 | 2.2 | 1.8 |
| Previous MI | |||
| No | 1591 | 98.0 | 98.2 |
| Yes | 33 | 2.0 | 1.8 |
AL: adequate literacy; HLLL: high likelihood of limited literacy; MI: myocardial infarction; NVS: Newest Vital Sign; PLL: possibility of limited literacy.
Nearly 30% of the participants did not answer or did not know how to answer the questions regarding perceived risk of stroke and MI. The proportion of non-responses was approximately two times higher among older participants and nearly 40% lower among those with AL. Subjects with a previous diagnosis of stroke were less likely to estimate the lifetime risk of stroke in the population (PR=0.41, 95% CI: 0.21-0.79). The respondents stated that, on average, 34.2% and 35.6% of the Portuguese population would suffer a stroke or MI, respectively, during their lifetime (Table 2). The risk estimates provided by men were approximately 8% lower than those provided by women, and for stroke those provided by participants older than 69 were 9.6% higher than the estimates by younger participants.
Perceived risk of stroke and myocardial infarction, according to sociodemographic characteristics, health literacy and history of cardiovascular disease.
| For every 100 Portuguese, how many will have this disease during their lives? | ||||||||
|---|---|---|---|---|---|---|---|---|
| Stroke | Myocardial infarction | |||||||
| Don’t know/did not answer | No. of people affected | Don’t know/did not answer | No. of people affected | |||||
| % | PR (95% CI)a | Mean | β (95% CI)a | % | PR (95% CI)a | Mean | β (95% CI)a | |
| Overall | 29.9 | --- | 34.2 | --- | 29.7 | --- | 35.6 | --- |
| Gender | ||||||||
| Female | 29.2 | [reference] | 38.4 | [reference] | 30.4 | [reference] | 40.0 | [reference] |
| Male | 30.6 | 1.09 (0.90 to 1.32) | 29.8 | −8.26 (−11.37 to −5.15) | 29.0 | 0.98 (0.80 to 1.21) | 31.3 | −8.13 (−11.44 to −4.83) |
| Age (years) | ||||||||
| <30 | 20.3 | [reference] | 31.6 | [reference] | 19.3 | [reference] | 33.4 | [reference] |
| 30-39 | 19.5 | 0.95 (0.60 to 1.51) | 33.9 | 2.73 (−2.78 to 8.24) | 20.1 | 1.01 (0.63 to 1.63) | 36.5 | 3.68 (−2.13 to 9.50) |
| 40-49 | 37.4 | 1.67 (1.11 to 2.52) | 35.2 | 3.07 (−2.40 to 8.54) | 37.8 | 1.73 (1.14 to 2.63) | 36.2 | 2.29 (−3.64 to 8.22) |
| 50-59 | 30.6 | 1.33 (0.89 to 1.99) | 35.4 | 2.92 (−2.59 to 8.44) | 33.7 | 1.48 (0.99 to 2.21) | 36.9 | 2.52 (−3.94 to 8.98) |
| 60-69 | 34.0 | 1.47 (0.97 to 2.22) | 34.7 | 1.69 (−5.31 to 8.68) | 32.1 | 1.40 (0.92 to 2.12) | 34.5 | −1.19 (−8.85 to 6.47) |
| 70-79 | 55.5 | 2.27 (1.49 to 3.46) | 41.4 | 9.59 (0.91 to 18.26) | 51.7 | 2.09 (1.36 to 3.22) | 42.2 | 8.43 (−0.60 to 17.46) |
| Education (years) | ||||||||
| <5 | 36.9 | [reference] | 35.3 | [reference] | 36.9 | [reference] | 37.0 | [reference] |
| 5-9 | 33.5 | 1.21 (0.91 to 1.62) | 34.8 | 1.67 (−3.80 to 7.14) | 34.1 | 1.19 (0.90 to 1.58) | 34.9 | −2.24 (−8.14 to 3.66) |
| 10-12 | 21.5 | 0.91 (0.63 to 1.32) | 31.8 | −1.10 (−7.27 to 5.07) | 20.9 | 0.86 (0.59 to 1.25) | 33.9 | −3.24 (−10.22 to 3.75) |
| >12 | 19.6 | 0.90 (0.59 to 1.40) | 34.3 | 1.61 (−5.04 to 8.25) | 17.9 | 0.77 (0.49 to 1.22) | 35.6 | −1.93 (−9.33 to 5.48) |
| Health literacy (NVS) | ||||||||
| HLLL | 37.7 | [reference] | 34.6 | [reference] | 37.5 | [reference] | 34.2 | [reference] |
| PLL | 28.3 | 0.87 (0.68 to 1.11) | 36.3 | 1.83 (−2.42 to 6.08) | 26.9 | 0.82 (0.64 to 1.06) | 39.6 | 6.19 (1.70 to 10.68) |
| AL | 17.8 | 0.61 (0.42 to 0.87) | 31.5 | −1.92 (−6.60 to 2.75) | 18.8 | 0.66 (0.48 to 0.91) | 33.6 | 1.34 (−3.62 to 6.31) |
| Hypertension | ||||||||
| No | 27.9 | [reference] | 33.6 | [reference] | 27.6 | [reference] | 35.2 | [reference] |
| Yes | 42.1 | 1.11 (0.87 to 1.42) | 38.8 | 1.69 (−2.68 to 6.06) | 42.6 | 1.14 (0.88 to 1.48) | 39.2 | 1.02 (−3.54 to 5.57) |
| Previous stroke | ||||||||
| No | 30.2 | [reference] | 34.1 | [reference] | 29.7 | [reference] | 35.6 | [reference] |
| Yes | 17.4 | 0.41 (0.22 to 0.79) | 36.3 | 0.95 (−6.16 to 8.06) | 29.5 | 0.71 (0.30 to 1.67) | 36.0 | 0.82 (−8.13 to 9.76) |
| Previous MI | ||||||||
| No | 29.8 | [reference] | 34.1 | [reference] | 29.6 | [reference] | 35.5 | [reference] |
| Yes | 38.2 | 0.83 (0.39 to 1.77) | 40.4 | 5.77 (−5.41 to 16.95) | 34.9 | 0.79 (0.35 to 1.75) | 39.9 | 3.80 (−6.11 to 13.71) |
AL: adequate literacy; CI: confidence interval; HLLL: high likelihood of limited literacy; MI: myocardial infarction; NVS: Newest Vital Sign; PLL: possibility of limited literacy; PR: prevalence ratio.
“Not smoking” and a “healthy diet” were identified as the most important behaviors for prevention of cardiovascular disease by 36.8% and 32.8% of the participants, respectively, while only 3.4% reported “check blood pressure” (Figure 1). No significant differences were observed in responses concerning preventive behaviors according to sociodemographic characteristics, health literacy or previous diagnosis of hypertension, stroke or MI, except for physical exercise, which was less frequently identified by respondents over 69 years old (PR=0.39, 95% CI: 0.17-0.89).
Knowledge on behaviors for prevention of cardiovascular diseases.
a Percentage of participants identifying each behavior as the most important for prevention of cardiovascular disease.
Other behaviors included the intake of multivitamins, regular weighing, regular blood tests, and regular general check-ups.
Less than half of the participants answered “call emergency number” as the most appropriate procedure in the presence of facial drooping and chest pain (48.0% and 45.1%, respectively); this was independently associated with greater levels of health literacy (AL: PR=1.44; 95% CI: 1.17-1.76 and AL: PR=1.45; 95% CI: 1.17-1.80, respectively, in comparison with HLLL). Among the other participants, 42.2% and 39.6% answered “go to an emergency department” when faced with an alarm sign or symptom of stroke and MI, respectively, while 1.1% and 0.8% were unable to answer.
Data about knowledge on the consequences of stroke and MI are presented in Figure 2. The most frequently reported consequences were “dependence in daily activities” (90.7%), “impaired speech” (89.8%) and “paralysis” (84.3%) for stroke, and “heart failure” (86.4%), “dependence in daily activities” (85.3%), “impaired driving” (81.6%) and “angina pectoris” (81.5%) for MI.
Table 3 presents the distribution of the two most frequently reported consequences of stroke and MI, according to sociodemographic characteristics, health literacy, and clinical history of the participants. Identification of “dependence in daily activities” as a consequence of stroke was more frequent among those with adequate health literacy (AL vs. HLLL: PR=1.08; 95% CI: 1.01-1.14) and with a previous diagnosis of hypertension (PR=1.05; 95% CI: 1.00-1.09), while “impaired speech” was more likely to be reported by more educated participants (>12 vs. <5 years education: PR=1.10; 95% CI: 1.00-1.21), those with adequate health literacy (AL vs. HLLL: PR=1.07; 95% CI: 1.02-1.13) and with a previous diagnosis of MI (PR=1.12; 95% CI: 1.06-1.18). Regarding the main consequences of MI, participants with adequate health literacy (AL vs. HLLL: PR=1.11; 95% CI: 1.04-1.19) and with a previous diagnosis of MI (PR=1.18; 95% CI: 1.06-1.31) more frequently stated “heart failure”, while those who had experienced stroke were more likely to identify “dependence in daily activities” (PR=1.14; 95% CI: 1.06-1.22).
The two most frequently reported consequences of stroke and myocardial infarction, according to sociodemographic characteristics, health literacy and history of cardiovascular disease.
| Consequences of stroke | Consequences of MI | |||||||
|---|---|---|---|---|---|---|---|---|
| Dependence in daily activities | Impaired speech | Heart failure | Dependence in daily activities | |||||
| % | PR (95% CI)a | % | PR (95% CI)a | % | PR (95% CI)a | % | PR (95% CI)a | |
| Gender | ||||||||
| Women | 92.1 | [reference] | 88.4 | [reference] | 86.2 | [reference] | 85.7 | [reference] |
| Men | 89.2 | 0.97 (0.93 to 1.01) | 91.2 | 1.03 (0.98 to 1.08) | 86.6 | 1.00 (0.93 to 1.07) | 85.0 | 0.99 (0.94 to 1.04) |
| Age (years) | ||||||||
| <30 | 92.3 | [reference] | 88.4 | [reference] | 87.7 | [reference] | 85.6 | [reference] |
| 30-39 | 87.1 | 0.94 (0.87 to 1.02) | 90.7 | 1.02 (0.95 to 1.10) | 87.2 | 0.99 (0.90 to 1.09) | 83.5 | 0.98 (0.89 to 1.08) |
| 40-49 | 88.5 | 0.98 (0.89 to 1.08) | 93.7 | 1.09 (1.00 to 1.18) | 89.2 | 1.04 (0.94 to 1.15) | 86.0 | 1.02 (0.92 to 1.12) |
| 50-59 | 95.0 | 1.07 (0.99 to 1.15) | 90.5 | 1.06 (0.97 to 1.16) | 90.6 | 1.07 (0.99 to 1.15) | 90.7 | 1.07 (0.98 to 1.17) |
| 60-69 | 90.9 | 1.05 (0.95 to 1.16) | 90.0 | 1.08 (0.97 to 1.20) | 86.1 | 1.04 (0.94 to 1.15) | 84.9 | 1.01 (0.90 to 1.14) |
| 70-79 | 89.3 | 1.04 (0.93 to 1.16) | 83.1 | 1.01 (0.89 to 1.13) | 69.6 | 0.85 (0.72 to 1.01) | 78.9 | 0.94 (0.80 to 1.10) |
| Education (years) | ||||||||
| <5 | 88.4 | [reference] | 87.2 | [reference] | 82.6 | [reference] | 85.0 | [reference] |
| 5-9 | 91.7 | 1.05 (0.96 to 1.16) | 92.1 | 1.05 (0.97 to 1.14) | 89.8 | 1.05 (0.97 to 1.13) | 84.1 | 0.98 (0.89 to 1.07) |
| 10-12 | 91.8 | 1.05 (0.94 to 1.17) | 89.0 | 1.03 (0.93 to 1.14) | 88.8 | 1.03 (0.94 to 1.14) | 87.3 | 1.02 (0.93 to 1.12) |
| >12 | 94.6 | 1.07 (0.96 to 1.19) | 96.8 | 1.10 (1.00 to 1.21) | 90.1 | 1.03 (0.94 to 1.13) | 85.4 | 0.99 (0.89 to 1.10) |
| Health literacy (NVS) | ||||||||
| HLLL | 87.6 | [reference] | 87.3 | [reference] | 81.8 | [reference] | 83.9 | [reference] |
| PLL | 91.7 | 1.04 (0.98 to 1.10) | 88.6 | 1.00 (0.94 to 1.07) | 87.4 | 1.03 (0.97 to 1.10) | 85.4 | 1.00 (0.93 to 1.08) |
| AL | 94.8 | 1.08 (1.01 to 1.14) | 95.7 | 1.07 (1.02 to 1.13) | 93.5 | 1.11 (1.04 to 1.19) | 87.9 | 1.04 (0.97 to 1.12) |
| Hypertension | ||||||||
| No | 90.2 | [reference] | 89.8 | [reference] | 86.9 | [reference] | 85.4 | [reference] |
| Yes | 93.4 | 1.05 (1.00 to 1.09) | 89.7 | 1.03 (0.98 to 1.08) | 83.7 | 1.01 (0.93 to 1.10) | 85.3 | 1.01 (0.92 to 1.11) |
| Previous stroke | ||||||||
| No | 90.6 | [reference] | 89.7 | [reference] | 86.3 | [reference] | 85.1 | [reference] |
| Yes | 94.4 | 1.04 (0.95 to 1.15) | 95.4 | 1.08 (0.98 to 1.19) | 91.0 | 1.09 (0.96 to 1.24) | 97.0 | 1.14 (1.06 to 1.22) |
| Previous MI | ||||||||
| No | 90.6 | [reference] | 89.7 | [reference] | 86.3 | [reference] | 85.6 | [reference] |
| Yes | 93.7 | 1.06 (0.97 to 1.16) | 97.6 | 1.12 (1.06 to 1.18) | 93.7 | 1.18 (1.06 to 1.31) | 74.3 | 0.89 (0.60 to 1.31) |
AL: adequate literacy; CI: confidence interval; HLLL: high likelihood of limited literacy; MI: myocardial infarction; NVS: Newest Vital Sign; PLL: possibility of limited literacy; PR: prevalence ratio.
The present study is innovative, providing a characterization of key aspects of health-related knowledge on the frequency, prevention, control and consequences of CVD among the Portuguese population. Interpretation of the results needs to take into account that gaps in specific aspects of such knowledge may be expected to have different impacts on efforts for prevention and control of stroke and MI.
Nearly one third of the participants were unable to estimate the lifetime risk of MI and stroke in the population. The proportion of non-respondents was high, especially among older participants, taking into account the high burden of stroke and MI in the Portuguese population,4 the attention given in the last decade to this subject in health promotion campaigns aimed at the general population,17,18 and the increasing incidence of these conditions with age.19
Overall, the perceived risk of stroke and MI was overestimated, with available studies on the Portuguese population reporting incidence rates of 207.3/100000 and 82.9/100000 population, respectively,20 and prevalence estimates between 1.6 and 3.2%.21–23 However, it would probably be difficult for the general population to distinguish between these measures, and information regarding the risk of stroke and MI comes from methodologically heterogeneous studies carried out in populations with different characteristics. It is estimated that stroke will affect at least one in six middle-aged people during the rest of their lives.24,25 Although similar estimates are presented for men regarding MI, the risk is lower for women, with approximately one in nine middle-aged women suffering MI in their remaining lifetime.26 Despite the higher prevalence of CVD among men,3 in our study women reported a higher perception of risk, as observed in previous studies.27,28 Also, older participants tended to have higher risk perception, which may be due to more frequent provision of information by the health care system about stroke and MI, since they are at greater risk of disease.19
Prevention and control of the main modifiable CVD risk factors, such as smoking, alcohol consumption, unhealthy diet, obesity, hypertension, dyslipidemia, diabetes, psychological stress and a sedentary lifestyle, are fundamental tools to reduce the burden of stroke and CHD.29,30 Participants identified not smoking and a healthy diet as the main preventive behaviors for CVD, although they attributed lower importance to blood pressure control, despite the high prevalence of hypertension in the country.22 However, since participants were asked to select the most important from a list of different behaviors, it is possible that they assumed high blood pressure would be a consequence of unhealthy lifestyles. Recent guidelines on CVD prevention in clinical practice suggest that cognitive-behavioral methods are effective in helping individuals to adopt a healthy lifestyle, emphasizing the implementation of nutrition, exercise, relaxation training, weight management and smoking cessation programs.31 This calls for appropriate and effective communication between patients and health professionals, which will facilitate treatment and prevention of CVD.
In Portugal, in the presence of signs and/or symptoms suspicious of stroke or MI, the correct procedure is to call the emergency number.32 Although less than half of the participants surveyed selected this option in the presence of facial drooping or chest pain, approximately 40% indicated that they would go directly to the emergency department, which is also a valid procedure. The results presented are in agreement with previous Portuguese studies, which revealed that only between 22.4% and 68.0% of respondents would call the emergency number when faced with a possible stroke or MI.33–35 These low percentages may be due to two main factors: lack of awareness of the importance of calling the emergency number, thus activating fast-track protocols, or the inability to link these signs and symptoms to events such as stroke or MI. One study conducted in Portugal showed that 24% of respondents did not recognize the signs and symptoms of MI.33 Nevertheless, in our population, the likelihood of taking appropriate action, i.e., calling the emergency number in the presence of facial drooping or chest pain, increased with health literacy, which highlights the need to improve health literacy and cardiovascular disease knowledge in the Portuguese population.
As a consequence of downward trends in mortality, the number of survivors from CHD and stroke is increasing, which in turn has led to a greater number of individuals suffering from sequelae.36 There is a wide range of outcomes after a CVD event, from no sequelae to a comatose state, with considerable personal, emotional, professional and financial costs to both individuals and health services.37 Although dependence in daily activities was frequently recognized as a major outcome of stroke and MI, this sequela is in fact more prevalent in stroke.38 This finding may be a consequence of the difficulty among the general population of differentiating MI and stroke. Other potential consequences of stroke, such as epilepsy and dementia, were less frequently reported, possibly because they may be perceived as less severe, or as having other causes. However, previous studies reveal that stroke almost doubles the risk of dementia after the age of 65,39 and is the leading cause of seizures and epilepsy in the elderly.40 Thus, the dissemination of more comprehensive information regarding the global burden of CVD is essential among the general population.
Overall, respondents with AL were more likely to answer the questions and to provide correct responses than those with HLLL. However, a recent study reported that 49% of Portuguese respondents have limited health literacy,41 highlighting the need to assess citizens’ health-related knowledge when planning cardiovascular policy strategies.
This study addressed a topic rarely investigated in Portugal – knowledge of CVD – based on a representative sample of Portuguese-speaking residents of mainland Portugal. However, some limitations should be acknowledged. Health literacy was measured using an instrument designed to assess overall health literacy skills42 that is not specific to cardiovascular health-related knowledge. Thus, the instrument may not be sufficiently sensitive to assess health literacy concerning CVD specifically, given its particular characteristics. Data on the consequences of stroke and MI were obtained from recognition of possible consequences in a list, which could lead to overestimation of knowledge in this domain. It has been shown that closed-ended questions in general yield higher percentages of responses than open-ended questions,43 and the lower proportion of non-respondents in these questions appears to support this assumption. However, taking into account that the main consequences of stroke and MI were considered, significant overestimation is unlikely.
ConclusionEffective prevention and control of CVD risk factors as well as the recognition of signs, symptoms, and what to do when faced with alarm signs of an acute event44 are essential to reduce the burden of CVD. In the present study, the large proportion of non-respondents to questions addressing health-related knowledge on stroke and MI, which are common conditions in Portugal, as well as participants’ lack of knowledge about vital aspects of these diseases, highlight the existence of important gaps in cardiovascular health-related knowledge. However, it was also observed that individuals with adequate health literacy responded more often and more appropriately than those with limited literacy, indicating that health education strategies and practices should be sensitive to these differences in order to improve cardiovascular health knowledge among the Portuguese population.
Conflicts of interestThe authors have no conflicts of interest to declare.
This study was funded by through the Operational Program Competitiveness and Internationalization and national funding from the, under the project ‘Health information of Portuguese population: Knowledge and perceived quality and accessibility of health information sources’ (ref. FCT: HMSP-IISE/SAU-ICT/0004/2009), and the Unidade de Investigação em Epidemiologia – Instituto de Saúde Pública da Universidade do Porto (EPIUnit) (POCI-01-0145-FEDER-006862; ref. UID/DTP/04750/2013); the Postdoc Grant (to EA) and the PhD grant (to ARC) were co-funded by the and Programa Operacional Capital Humano (POCH/FSE).
The English version of the NVS was developed by Pfizer Inc. Pfizer Inc. granted authorization for the translation and assessment of the psychometric properties of NVS for the Portuguese language in the adult population (aged 18 to 64 years).