Self-reported heath and quality of life is an independent predictor of overall and cardiovascular morbidity and mortality, and incident coronary heart disease. However, less is known regarding how gender differences in cardiovascular risk factors impact quality of life perception.
MethodsPrimary healthcare users (n=261, 158 women) were screened for cardiovascular risk factors and completed the Medical Outcomes Study Short Form (SF-36).
ResultsWomen had significantly lower alcohol consumption, body mass index and exercise frequency than men, but more prevalent psychiatric history, depressive and anxiety symptoms, and negative affectivity. Prevalences of hypertension, diabetes, dyslipidemia and type D personality were similar between genders. Women reported significantly worse quality of life on most SF-36 subscales and gender differences were apparent in predictors of quality of life. Moreover, high negative affectivity was an independent predictor of worse general health for women, whereas high social inhibition and high anxiety had a comparable role for men.
ConclusionGender specifics in cardiovascular risk factors should be considered in prevention strategies. Women reported significantly worse quality of life, putting them at higher risk for cardiovascular morbidity and mortality. Therefore, gender differences in predictors of quality of life warrant further investigation.
A perceção de qualidade de vida é um preditor independente de mortalidade geral, morbilidade e mortalidade cardiovascular, e incidência de doença cardíaca coronária. Contudo, permanece por esclarecer qual o impacto que as diferenças específicas de género nos fatores de risco cardiovascular têm na perceção de qualidade de vida.
MétodosDuzentos e sessenta e um utentes dos cuidados primários (158 mulheres) foram rastreados para fatores de risco cardiovascular e preencheram a versão portuguesa do Medical Outcomes Study Short Form (SF-36).
ResultadosAs mulheres apresentaram um padrão de menor consumo de álcool, índice de massa corporal e frequência de exercício físico, mas maior prevalência de antecedentes psiquiátricos, sintomatologia depressiva e ansiosa, e afetividade negativa. As prevalências de hipertensão, diabetes, dislipidemia e personalidade tipo D foram semelhantes entre homens e mulheres. Globalmente, as mulheres apresentaram piores índices de qualidade de vida na maioria das subescalas do SF-36 e encontraram-se diferenças de género nos preditores de qualidade de vida. Enquanto nas mulheres, a elevada afetividade negativa foi um preditor independente de pior saúde geral, nos homens, esse efeito foi verificado para índices elevados de inibição social e ansiedade.
ConclusõesAs especificidades de género nos fatores de risco cardiovascular devem ser tidas em consideração nas estratégias de prevenção primária. As mulheres apresentam qualidade de vida significativamente pior, o que as coloca em maior risco de morbilidade e mortalidade cardiovascular, pelo que as diferenças de género nos preditores de qualidade de vida devem ser investigados.
Cardiovascular disease (CVD) remains the leading cause of premature death in Europe. Unhealthy lifestyles and psychosocial burden are commonly associated with CVD, and not surprisingly, most of its mortality is preventable through appropriate changes in lifestyle.1 It is well established that psychosocial risk factors interact with biomedical vulnerabilities in the development of CVD, and approximately one third of the attributable risk of acute myocardial infarction can be related to major life events, depression or stress related to work, family or finances. Furthermore, when several psychosocial risk factors cluster in the same individual, the risk for both cardiac events and severe atherosclerosis is substantially increased.2
Men and women have similar biomedical risk factors for CVD, but their relative weight and impact on the pathophysiology of the disease differ markedly.3 Prevention strategies could benefit from taking these risk profile differences into account. Further, gender differences in both disease progression and impact of risk factors could explain why prevalence rates, symptom profiles and medical outcomes still have different prevalences between genders.4,5 Specifically, women with ischemic heart disease have worse outcomes than men regardless of age,4 but usually present much less severe anatomical obstructive lesions and better preserved systolic function.4,6 Clearly, other factors are at play in this apparent contradiction.
It is well established that psychosocial factors such as negative affect and personality traits can increase the risk for CVD.2 However, it is unknown whether they also impact cardiovascular health differentially by gender, thereby contributing to higher CVD morbidity and mortality among women. Specifically, depression is an established risk factor for both CVD patients and healthy individuals, increasing both cardiac morbidity and mortality,7–9 while anxiety has been identified as an independent risk factor for CVD in the community.10,11 Similarly, type D personality is a stable personality construct marked by negative affectivity and social inhibition that combine to produce sustained high levels of mental distress and increased physical symptoms in both CVD patients and healthy participants.12–14 Overall, these psychosocial factors have been consistently linked to CVD risk, but little progress has been made in examining their differential impact by gender.
Self-reported health is an independent predictor of overall and cardiovascular mortality in most studies, and individuals who assess their health as fair or poor have a higher mortality risk than those whose assessment is better.15,16 Moreover, after controlling for sociodemographic characteristics, health care access and risk factors, self-reported health is still a significant and independent predictor of both global morbidity onset15 and CVD incidence.17,18 Specifically, the Medical Outcomes Study Short Form (SF-36) has been shown to predict mortality in community samples.19,20 In particular, the physical component summary of the SF-36 (derived from the sum of scores obtained on the physical functioning, role-physical, bodily pain and general health subscales) exhibits a strong association with mortality, estimates being independent of other physical factors like obesity, physical inactivity or a low-fiber diet.19,20
This study aimed to assess how gender patterns of known cardiovascular risk factors (biomedical and psychosocial) influence self-reported quality of life in a sample of primary health care users without a CVD diagnosis. To the best our knowledge, this study is pioneering in bridging these two important issues.
MethodsParticipantsAs part of a prospective study, 261 primary health care users (158 women) were recruited in various health provision settings in the northern region of Portugal. The study design was explained to each participant and written informed consent was obtained. Exclusion criteria comprised either documented or self-reported CVD.
InstrumentsParticipants were interviewed and assessed for various demographic, behavioral, clinical and psychosocial measures. Questionnaires were used to collect these data.
The Hospital Anxiety and Depression Scale (HADS) is a self-evaluation questionnaire which comprises two subscales, one measuring depression (HAD-D) and the other measuring anxiety (HAD-A).21,22 The HADS has been validated for the Portuguese population.23 A HADS cutoff score greater than 7 in any of the subscales indicates the presence of symptoms, e.g. HAD-D ≥8 indicates depressive symptoms.
Type D personality was assessed using a Portuguese version of the Type D Scale-14 (DS14), which comprises 14 items, seven assessing negative affectivity and seven assessing social inhibition.24 A score of at least 10 on both subscales identifies individuals as having type D (or distressed) personality.25
Quality of life was assessed using the Portuguese version of the Medical Outcomes Study Short Form SF-36,26,27 which comprises 36 questions across eight subscales of functional health and well-being: physical functioning, role-physical, bodily pain, general health, mental health, role-emotional, social functioning and vitality.
Data reduction and analysisUnivariate analysis was used to compare demographic, behavioral, clinical and psychometric variables between genders. Differences between proportions were examined with chi-square tests, while mean comparisons were conducted with Student's t tests. A multivariate logistic regression analysis (backward stepwise method) was conducted to quantify independent associations of previously identified correlates with gender. Adjusted odds ratios (OR) with 95% confidence intervals are reported. A series of multivariate linear regression analyses were conducted separately by gender to identify putative predictors of quality of life scores. The statistical significance level was set at p<0.05.
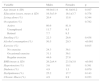
ResultsUnivariate analysisSociodemographic and clinical variables were compared by gender (Table 1). No differences were found regarding age, educational level, living status or occupation. Women presented significantly lower alcohol consumption (p<0.001), lower body mass index (p<0.001) and less exercise activity (p<0.05) than men. Regarding psychosocial measures (Table 2), women scored significantly higher than men for HAD-D (p<0.05), which was corroborated by a greater proportion of women (19% vs. 9.7%) exceeding the scale cutoff for depression (p<0.05). A history of antidepressant medication use (p=0.05) and psychiatric referral and/or complaints (p<0.05) was also more common among women. The prevalence of type D personality was similar between genders, although women scored significantly higher than men in negative affectivity (p=0.05). Finally, women had lower scores in all SF-36 dimensions, indicating an overall perception of poorer health and well-being, and this was statistically significant for all dimensions with the exception of general health (p=0.505).
Univariate comparison of participants’ sociodemographic and clinical characteristics by gender.
| Variable | Males | Females | p |
|---|---|---|---|
| Age (mean ± SD) | 44.0±11.4 | 41.8±10.2 | 0.107 |
| Education (years, mean ± SD) | 16.5±3.9 | 16.1±3.7 | 0.378 |
| Living alone (%) | 20.4 | 15.8 | 0.344 |
| Occupation (%) | 0.782 | ||
| Active | 80.6 | 81.0 | |
| Unemployed | 11.7 | 9.5 | |
| Retired | 7.7 | 9.5 | |
| Smoking (%) | 22.3 | 26.6 | 0.438 |
| Alcohol consumption (%) | 50.5 | 20.3 | <0.001 |
| Exercise (%) | 0.015 | ||
| No exercise | 24.3 | 36.1 | |
| Occasional exercise | 31.1 | 36.1 | |
| Regular exercise | 44.6 | 27.8 | |
| BMI (mean ± SD) | 26.2±4.4 | 23.5±3.8 | <0.001 |
| Hypertension (%) | 3.6 | 10.1 | 0.391 |
| Diabetes (%) | 4.9 | 1.3 | 0.079 |
| Dyslipidemia (%) | 25.2 | 17.7 | 0.143 |
| Chronic illness (%) | 4.9 | 8.9 | 0.223 |
BMI: body mass index; SD: standard deviation.
Univariate comparison of participants’ psychometric outcomes by gender.
| Variables | Males | Females | p |
|---|---|---|---|
| Depression | |||
| HADS-D (mean ± SD) | 2.8±3.2 | 3.8±4.0 | 0.022 |
| HADS-D ≥8 (%) | 9.7 | 19.0 | 0.042 |
| Antidepressant medication (%) | 5.8 | 13.3 | 0.053 |
| Psychiatric history (%) | 16.5 | 27.2 | 0.044 |
| Anxiety | |||
| HADS-A (mean ± SD) | 4.5±3.8 | 5.1±4.2 | 0.236 |
| HADS-A ≥8 (%) | 22.3 | 25.9 | 0.506 |
| Type D personality (DS14) | |||
| Type D (NA ≥10 and SI ≥10) (%) | 22.3 | 18.4 | 0.432 |
| NA (mean ± SD) | 7.4±6.4 | 9.1±7.6 | 0.054 |
| SI (mean ± SD) | 8.0±6.6 | 7.7±6.8 | 0.743 |
| Quality of life (SF-36 components) | |||
| Physical functioning (mean ± SD) | 94.5±11.9 | 90.7±16.5 | 0.031 |
| Role-physical (mean ± SD) | 97.8±10.6 | 90.6±24.7 | 0.001 |
| Bodily pain (mean ± SD) | 89.8±13.3 | 82.6±20.4 | 0.001 |
| General health (mean ± SD) | 76.5±15.6 | 73.1±18.8 | 0.116 |
| Mental health (mean ± SD) | 79.7±15.6 | 71.6±20.5 | <0.001 |
| Role-emotional (mean ± SD) | 91.6±26.7 | 77.28±37.0 | <0.001 |
| Social functioning (mean ± SD) | 89.4±16.0 | 83.04±21.0 | 0.006 |
| Vitality (mean ± SD) | 72.0±15.6 | 63.4±20.1 | <0.001 |
DS14: Type D Scale-14; HADS-A: Hospital Anxiety and Depression Scale – Anxiety; HADS-D: Hospital Anxiety and Depression Scale – Depression; NA: negative affectivity; SF-36: Medical Outcomes Study Short Form; SI: social inhibition.
Table 3 shows the multivariate logistic regression model (Nagelkerke R2=0.32) obtained for the independent correlates of gender. Lower body mass index (p<0.001), less frequent exercise (p<0.01), and less alcohol consumption (p<0.001) were all independently associated with women (Table 3). Further, women were more than twice as likely than men to use antidepressants (OR 2.877, p=0.05) and to exceed the HADS-D cutoff for depression (OR 2.137, p=0.098).
Summary of multivariate model for the independent correlates of gender (multivariate logistic regression analysis).
| Correlates | B | SE | Wald chi-square | df | Odds ratio | 95% CI | p | |
|---|---|---|---|---|---|---|---|---|
| Body mass index | −0.209 | 0.041 | 26.06 | 1 | 0.812 | 0.749 | 0.879 | 0.000 |
| Occasional exercise | −0.364 | 0.371 | 0.964 | 1 | 0.695 | 0.336 | 1.437 | 0.326 |
| Frequent exercise | −1.016 | 0.368 | 7.613 | 1 | 0.362 | 0.176 | 0.745 | 0.006 |
| Alcohol consumption | −1.445 | 0.310 | 21.787 | 1 | 0.236 | 0.128 | 0.432 | 0.000 |
| HADS-D ≥8 | 0.759 | 0.459 | 2.735 | 1 | 2.137 | 0.869 | 5.256 | 0.098 |
| Antidepressant medication | 1.057 | 0.549 | 3.708 | 1 | 2.877 | 0.981 | 8.432 | 0.054 |
CI: confidence interval; df: degrees of freedom; HADS-D: Hospital Anxiety and Depression Scale – Depression; SE: standard error.
Backward likelihood ratio method; female gender coded as 1.
Table 4 displays the results of the multivariate linear regression analysis of participants’ quality of life scores (only statistically significant scores are shown). Among men, an increased sense of ‘physical functioning’ was predicted by lower body mass, more frequent exercise, less prevalent chronic illness and less antidepressant use, alongside a lower score for social inhibition (DS14). In women, living alone, higher education and more exercise predicted better ‘physical functioning’, while higher prevalences of hypertension, diabetes and antidepressant use were related to worse ‘physical functioning’. Role limitations due to physical problems (‘role-physical’ subscale, on which higher scores indicate less limitation due to physical problems) were mainly associated with the prevalence of diabetes in men. In women, higher body mass, higher depression scores (HADS-D) and more antidepressant use predicted more role limitations due to physical problems. Not surprisingly, a higher prevalence of hypertension and other chronic illness was predictive of more pain complaints in men (‘bodily pain’ subscale, on which higher scores indicate less pain complaints), whereas more frequent exercise was predictive of less pain complaints. In women, more pain complaints were predicted by higher body mass, higher prevalences of diabetes and psychiatric referrals, and higher DS14 scores for negative affectivity. In men, better ‘general health’ was predicted by younger age, a lower prevalence of diabetes, and lower anxiety (HADS-A) and social inhibition (DS14) scores, while better ‘mental health’ was solely predicted by lower scores on the anxiety (HADS-A), depression (HADS-D) and negative affectivity (DS14) scales. In women, however, better ‘general health’ was predicted by lower body mass, less prevalence of diabetes and other chronic illness, and lower negative affectivity scores (DS14). Similarly to men, women reporting better ‘mental health’ were those with lower anxiety (HADS-A), depression (HADS-D) and negative affectivity (DS14) scores. Lower depression scores (HADS-D) predicted less role limitations due to emotional problems (a higher score on the ‘role-emotional’ dimension), while better ‘social functioning’ was associated with lower HADS-A scores in anxiety in men. In women, less role limitations due to emotional problems (a higher score on the ‘role-emotional’ dimension) were predicted by less alcohol consumption, and lower depression (HADS-D) and negative affectivity (DS14) scores. Concomitantly, better ‘social functioning’ was also predicted by less alcohol consumption and lower anxiety (HADS-A), depression (HADS-D) and social inhibition (DS14) scores. Finally, men with lower educational level and lower scores on the anxiety (HADS-A), depression (HADS-D) and social inhibition (DS14) scales had a greater sense of ‘vitality’. In women, greater vitality was significantly predicted by lower depression (HADS-D) and negative affectivity (DS14) scores.
Independent predictors of quality of life dimensions in men and women (multivariate linear regression analysis).
| SF-36 (standardized beta coefficients) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physical functioning | Role-physical | Bodily pain | General health | Mental health | Role-emotional | Social functioning | Vitality | |||||||||
| Predictor variables | M | F | M | F | M | F | M | F | M | F | M | F | M | F | M | F |
| Age | 0.002 | |||||||||||||||
| Living alone | <0.001 | |||||||||||||||
| Education | <0.001 | 0.006 | ||||||||||||||
| Occupation | ||||||||||||||||
| BMI | 0.015 | 0.012 | 0.010 | 0.000 | ||||||||||||
| Hypertension | 0.005 | 0.038 | ||||||||||||||
| Diabetes | 0.004 | 0.005 | 0.027 | 0.043 | 0.001 | |||||||||||
| Dyslipidemia | ||||||||||||||||
| Smoking | ||||||||||||||||
| Exercise | 0.001 | 0.039 | 0.024 | |||||||||||||
| Chronic illness | <0.001 | 0.014 | 0.006 | |||||||||||||
| Alcohol consumption | 0.032 | 0.008 | ||||||||||||||
| Psychiatric history | 0.017 | |||||||||||||||
| Antidepressant medication | <0.05 | 0.011 | 0.010 | |||||||||||||
| HADS-A | 0.035 | <0.001 | <0.001 | <0.001 | 0.011 | 0.002 | ||||||||||
| HADS-D | 0.009 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.001 | <0.001 | ||||||||
| DS 14 – negative affectivity | 0.005 | 0.000 | <0.001 | <0.001 | 0.001 | <0.001 | ||||||||||
| DS 14 – Social inhibition | <0.001 | 0.007 | 0.003 | 0.040 | 0. | |||||||||||
BMI: body mass index; DS14: Type D Scale-14; F: female; HADS-A: Hospital Anxiety and Depression Scale – Anxiety; HADS-D: Hospital Anxiety and Depression Scale – Depression; M: male; SF-36: Medical Outcomes Study Short Form.
Stepwise procedure; female gender coded as 1.
This study sought to examine how gender patterns of cardiovascular risk factors associate with self-reported quality of life in a sample of primary health care users without a CVD diagnosis. Our main findings pinpointed gender differences in risk factors mostly related to participants’ life style and mental/affective status. Specifically, women revealed significantly lower rates of alcohol consumption and exercise but presented more depressive symptoms and negative affectivity. In agreement with these findings, a history of antidepressant use and psychiatric referrals was also more common among women. Further, our multivariate analysis expanded these findings to confirm most of these risk factors as independent correlates for females.
Interestingly, traditional biomedical CVD risk factors, such as smoking, hypertension, diabetes and dyslipidemia, did not differ between genders. This finding partially supports the hypothesis of a different pathophysiological impact of CVD risk for female gender, possibly through the deleterious action of psychosocial risk factors like those mentioned above. In line with this suggestion, the quality of life assessment for female participants indicated overall poorer health and well-being, despite the absence of any objective gender difference in biomedical risk factors, which is in agreement with other studies that also reported lower quality of life scores for women.28
It is still not fully understood how educational level can influence the risk for CVD. Several studies have examined this and suggest that education partially affects this risk through increased prevalence of CVD risk factors at lower educational levels.29 In our study, despite the high educational level of the participants, we found a relatively high prevalence of risk factors which are mostly lifestyle dependent. We cannot exclude the possibility that our high educational level sampling masked any latent differences in traditional CVD risk factors. However, 36.1% of the women in our study did not exercise at all, which is higher than expected as studies have shown that lower education or occupation levels are usually associated with a higher prevalence of sedentariness among women.30 Also, no gender differences were found in smoking patterns, with the majority of participants being non-smokers. This follows the trend of western populations, where the prevalence of smoking is declining for both genders and increasing in lower social classes.31
Women had a prevalence of depressive symptoms that was more than twice that reported by men. In addition, psychiatric referrals and antidepressant use were also more prevalent among women. These data are in line with previous evidence showing that women are about twice as likely as men to experience depression.32 In addition, 22.3% of men and 25.9% of women were classified as anxious according to the HADS-A. This finding is apparently at odds with studies indicating a protective effect of educational level against anxiety and depression,33 but it might derive from an overall young sample. Finally, the prevalence of type D personality was similar between genders, replicating previous research.34,35 Nevertheless, women did score significantly higher than men on the negative affectivity subscale of the DS14, which has been considered elsewhere as a key predictor of worse subjective health outcomes.36
This study examined how gender patterns in CVD risk influence self-reported health and quality of life perception. Women reported significantly worse levels of well-being and health across most subscales of the SF-36 questionnaire, with the exception of the general health subscale (for which scores did not reach statistical significance, although they were still lower). Based on the findings of others,15,17,18 this could indicate that, in this study, women faced a higher risk for cardiovascular morbidity and mortality. Firstly, recent evidence indicates that poor self-rated health is strongly associated with cardiovascular mortality, irrespective of prior CVD,16 and with the incidence of coronary heart disease.17,18 Secondly, the physical health component of the SF-36 has been specifically identified as a strong predictor of CVD incidence and death in post-menopausal women.20 Thirdly, although the mechanisms underlying this association remain speculative, the fact is that the SF-36 physical health component exhibits a strong association with mortality, while this effect is independent of other risk factors like obesity, physical inactivity or diet.19,20
Among the gender distinctiveness apparent in the multivariate linear regression profiles of the quality of life scores, role limitations due to physical problems (‘role-physical’) and more pain complaints (‘bodily pain’) were predicted by psychosocial risk factors such as depression and negative affectivity in women, whereas in men these two dimensions appear to depend more on biomedical factors such as diabetes, hypertension, exercise and chronic illness. A recent study with healthy participants found that type D personality was significantly associated with lower quality of life and more physical symptoms, with the negative affectivity component standing out as the key predictor of subjective health outcomes.36 In our study, high negative affectivity was a strong independent predictor of worse general health for women, whereas high social inhibition and high anxiety had a comparable role for men. These results are worth highlighting given the predictive value of the SF-36 physical health component for CVD mortality and morbidity. Indeed, this distinct gender pattern may be the key to the differential impact of psychosocial risk factors on CVD risk, and should therefore be examined.
This study involves a population with highly specific characteristics, which is relevant for the following reasons. Firstly, our participants were relatively young and had a high educational level. While this requires caution regarding the generalization of findings to other populations, the fact is that studies aiming to enhance CVD prevention tend to be conducted with increasingly young samples.37,38 Secondly, our investigation followed an observational cross-sectional design, which precludes any generalization concerning longitudinal trends of the associations found. Thirdly, most of the data collection relied on self-reporting, hence reflecting the individual's assessment of currently experienced symptoms. Although memory bias could have distorted the data, such an effect is likely to be reflected similarly within the whole sample. Finally, multivariate analyses of quality of life scores were conducted separately by gender. On the one hand, sample size was limited in order to run meaningful multivariate linear regression comparisons between genders. On the other hand, the available evidence regarding self-rated health by gender is still inconsistent, with studies indicating no differences,39 a tendency for men to assess their health more positively than women,28 or even the opposite.40
Conclusions and implications for practiceThis study shows that community participants without documented CVD present gender-specific patterns of CVD risk factors and that these impact quality of life differentially. In our view, these gender specifics need to be considered in health prevention strategies, given the predictive value of quality of life for cardiovascular morbidity and mortality.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interest and fundingThe lead author received funding from Fundação para a Ciência e a Tecnologia in the form of a PhD grant (SFRH/BD/70327/2010). The other authors have no conflicts of interest to declare.