The association of the Mediterranean diet and exercise appears to have a protective role, reducing cardiovascular risk. This study investigated the effects of education sessions on the Mediterranean diet and an exercise program in modifying eating behaviors, body composition and abdominal fat.
MethodsAn experimental study was performed on 20 subjects with known coronary heart disease randomly assigned to experimental (n=10) and control (n=10) groups. Both groups received education sessions on the Mediterranean diet, but the experimental group also followed an eight-week program of specific exercises. A semiquantitative food frequency questionnaire was administered to analyze food intake, bioimpedance was used to measure weight, fat mass and lean mass, and waist circumference was measured to calculate waist-to-height ratio.
ResultsAfter eight weeks, protein (p<0.05) and cholesterol (p<0.05) intake in the experimental group had decreased significantly compared with the control group. Between the beginning and end of the study, there were significant decreases in the control group in carbohydrate (p<0.05) and saturated fat intake (p<0.05). In both groups the percentage of total fat (p<0.05) and fat mass (p<0.05) was significantly decreased. In the experimental group the waist-to-height ratio was significantly reduced (p<0.05).
ConclusionThe Mediterranean diet reduced carbohydrate and saturated fat intake, reflected in reduced fat mass. The association of the exercise program showed additional benefits in reduction of protein and cholesterol intake and abdominal fat.
A associação da dieta mediterrânica e de exercício físico parecem apresentar um papel protetor na diminuição do risco cardiovascular. Este estudo pretende verificar os efeitos de sessões de educação fundamentadas na dieta mediterrânica e de um programa de exercícios na modificação de comportamentos alimentares, composição corporal e gordura abdominal.
MétodosEstudo experimental composto por 20 indivíduos, com doença arterial coronária conhecida, distribuídos aleatoriamente em dois grupos: experimental (n=10) e controlo (n=10). Ambos os grupos foram sujeitos às sessões de educação para a saúde, mas o grupo experimental executou um programa suplementar de exercícios específicos durante oito semanas. Foi utilizado o questionário semiquantitativo de frequência alimentar para análise da ingestão de alimentos, a bioimpedância para medição do peso, massa gorda e massa magra, e o perímetro da cintura para cálculo da razão cintura-estatura.
ResultadosApós as oito semanas, o grupo experimental ingeriu significativamente menos proteínas (p<0,05) e colesterol (p<0,05) em comparação com o grupo controlo. Do momento inicial para o final, verificou-se apenas no grupo controlo uma diminuição significativa na ingestão de hidratos de carbono (p<0,05) e de gorduras saturadas (p<0,05). Ambos os grupos diminuíram significativamente a percentagem de gordura total (p<0,05) e massa gorda (p<0,05). O grupo experimental diminuiu significativamente a razão cintura-estatura (p<0,05).
ConclusãoA dieta mediterrânica reduziu a ingestão alimentar de hidratos de carbono e gorduras saturadas, refletindo-se na redução da massa gorda. A associação do programa de exercícios demonstrou benefícios acrescidos na diminuição da ingestão de proteínas e de colesterol, assim como na redução da gordura abdominal.
Cardiovascular disease is the leading cause of death in Europe. It is responsible for over four million deaths annually,1 and is one of the main causes of morbidity in Portugal and in Europe as a whole.1,2
Cardiac rehabilitation (CR) is a multidisciplinary intervention that includes components designed to reduce cardiovascular risk, encourage healthy behaviors, reduce physical impairment and promote an active lifestyle. The main elements of a CR program are counseling on exercise and control of modifiable cardiovascular risk factors such as hypertension, smoking, dyslipidemia, diabetes, sedentary lifestyle, obesity, alcohol abuse, stress and depression.2,3
Lifestyle and diet are considered the main modifiable factors in cardiovascular prevention, with health benefits being achieved by increasing exercise levels and adopting a healthier diet.4,5
The Mediterranean diet is characterized by plentiful plant foods such as bread, pasta and rice, green vegetables and legumes, fresh fruit, olive oil as the main source of fats, moderate quantities of fish, poultry, dairy products and eggs, small quantities of red meat and moderate consumption of wine, usually with meals. The diet is notable for its low levels of saturated fatty acids and high levels of monounsaturated fats, complex sugars, dietary fiber and antioxidants.6 It protects against coronary artery disease and is associated with reduced cardiovascular mortality.6,7 As well as its antioxidant and anti-inflammatory properties, which appear to be behind the reduction in cardiovascular risk,4,8 the Mediterranean diet may also help control weight and combat obesity.9 The absolute quantity of body fat is less important than its anatomical distribution, with greater accumulation of adipose tissue in the abdominal region (male pattern) being associated with metabolic complications.10,11 The energy imbalance that leads to overweight is due not only to unhealthy eating habits but also to a sedentary lifestyle.12
In a study of 28 European countries, the European Association for Cardiovascular Prevention & Rehabilitation showed that only 4% of eligible patients participated in phase II or phase III CR programs.13 This low rate of access to CR, together with the poor adherence associated with such programs, suggests that home-based CR is an attractive alternative in individuals at low cardiovascular risk. Properly structured and monitored home-based CR programs appear to be more effective than hospital-based programs in maintaining exercise levels and improving adherence.14,15
The aim of the present study was to investigate the effects of the Mediterranean diet in isolation and in conjunction with a home-based exercise program in modifying eating behaviors, body composition and abdominal fat in individuals with coronary heart disease participating in a phase IV (maintenance) CR program.
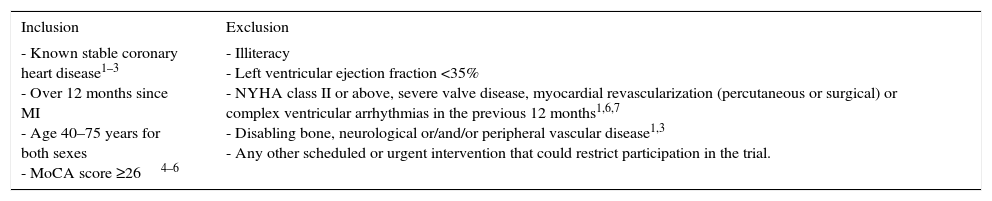
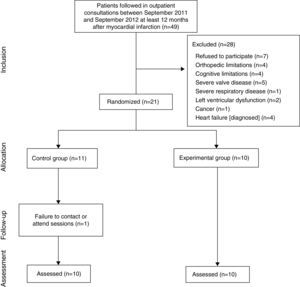
MethodsStudy populationThe sample in this randomized controlled trial was composed of 20 subjects with known coronary heart disease at least a year after myocardial infarction (MI) who were followed in outpatient cardiology consultations between September 2011 and September 2012. They all participated in phase I CR during post-MI hospitalization and an eight-week training phase at the hospital. Patients were invited individually to participate in the trial around nine months after the end of the training phase, in accordance with the inclusion and exclusion criteria (Table 1).
Inclusion and exclusion criteria.
| Inclusion | Exclusion |
|---|---|
| - Known stable coronary heart disease1–3 - Over 12 months since MI - Age 40–75 years for both sexes - MoCA score ≥264–6 | - Illiteracy - Left ventricular ejection fraction <35% - NYHA class II or above, severe valve disease, myocardial revascularization (percutaneous or surgical) or complex ventricular arrhythmias in the previous 12 months1,6,7 - Disabling bone, neurological or/and/or peripheral vascular disease1,3 - Any other scheduled or urgent intervention that could restrict participation in the trial. |
MI: myocardial infarction; MoCA: Montreal Cognitive Assessment; NYHA: New York Heart Association.
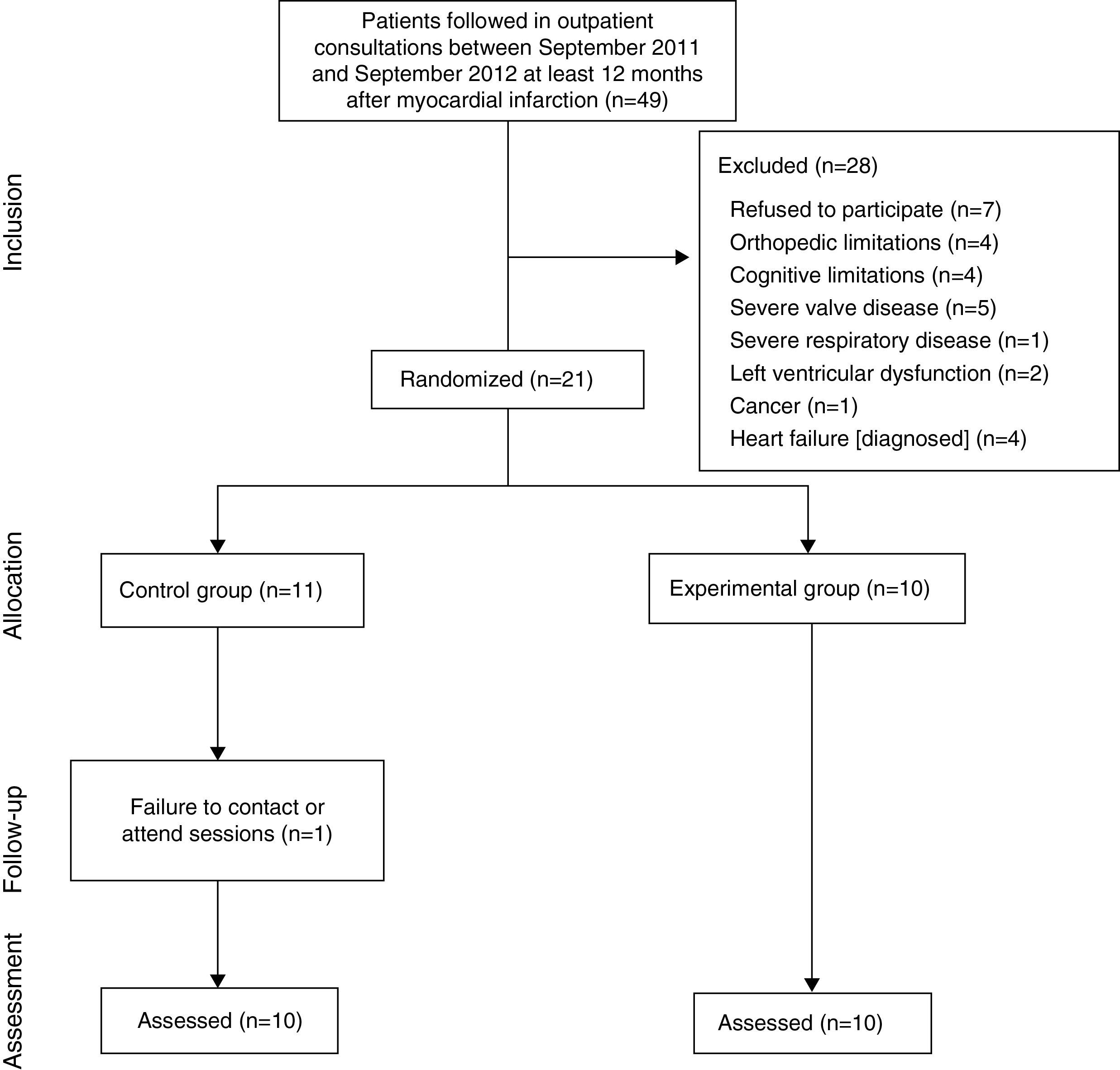
A total of 21 subjects agreed to participate in the study and were randomized to two groups using Microsoft Excel® 2010: an experimental group (EG), 10 participants following a home-based exercise program and education sessions on the Mediterranean diet; and a control group (CG) consisting of 11 participants who received the dietary education sessions but did not follow an exercise program (Figure 1). However, one member of the CG was excluded for failure to remain in contact and to attend the assessment sessions, and so the CG also had 10 participants by the end of the study.
InstrumentsA descriptive questionnaire was administered to all subjects who agreed to take part in the trial to confirm conformity with the inclusion and exclusion criteria. The questionnaire was divided into two parts, the first on demographic characteristics and the second on other medical conditions and/or limitations to participation in the study.
The Montreal Cognitive Assessment was used for cognitive screening, since participants had to understand the study's indications in order to perform the home-based exercise program safely.16
A semiquantitative food frequency questionnaire (FFQ) was applied to determine intake of total fat (kcal), saturated fat (kcal), monounsaturated fat (kcal), polyunsaturated fat (kcal), carbohydrate (kcal), protein (kcal), dietary fiber (g), cholesterol (mg), alcohol (g) and calories (kcal). The questionnaire consisted of a list of 86 individual foods or food groups, the intake of each one, predefined as an average portion, being classified as one of nine levels, ranging from “never or less than once a month” to “six or more times a day”. This FFQ has been validated for the Portuguese population17 and in the present study presented a Cronbach's alpha of 0.70. Food Processor Plus® software (ESHA Research Inc., Salem, OR) was used to convert food intake into nutrients.
Height was measured using a Seca 222 stadiometer (Seca, Birmingham, UK) with 1-mm gradations. A non-elastic tape with 1-mm gradations was used to measure waist circumference; this instrument showed excellent intraobserver reliability, with an intraclass correlation coefficient of 0.98 (3.1).18 Waist-to-height ratio (WHR) was calculated; this correlates strongly with obesity, a value of 0.5 being taken as the cutoff for coronary risk in various populations.19
Body composition was assessed using a TBF-300A body composition analyzer (Tanita Corporation, Arlington Heights, IL). This model, which has four electrodes (foot-to-foot), measures weight (kg), total fat percentage, total fat mass (kg) and total lean mass (kg) and presents a good correlation with the reference method, dual-energy X-ray absorptiometry (r=0.741).20 It has a maximum capacity of 200 kg with a precision of 100 g for weight, fat mass and lean mass and 0.1% for total fat percentage.21,22
The Polar® RS300X heart rate monitor (Polar Electro Oy, Kempele, Finland) was used during the session in which exercises were prescribed and taught.23 The Borg Rating of Perceived Exertion scale (6–20) was used to assess the levels of exertion perceived by the participants.24
ProceduresSubjects were assessed in the outpatient clinic of the cardiology department of Centro Hospitalar de Vila Nova de Gaia at two time points: initial (T0) and final (T1), eight weeks later.
During the face-to-face sessions, all participants, in both EG and CG, were asked to follow a Mediterranean diet based on the National Cholesterol Education Program/American Heart Association Step I diet as recommended for cardiovascular patients.25 The sessions were backed up by leaflets to help them follow the diet at home.
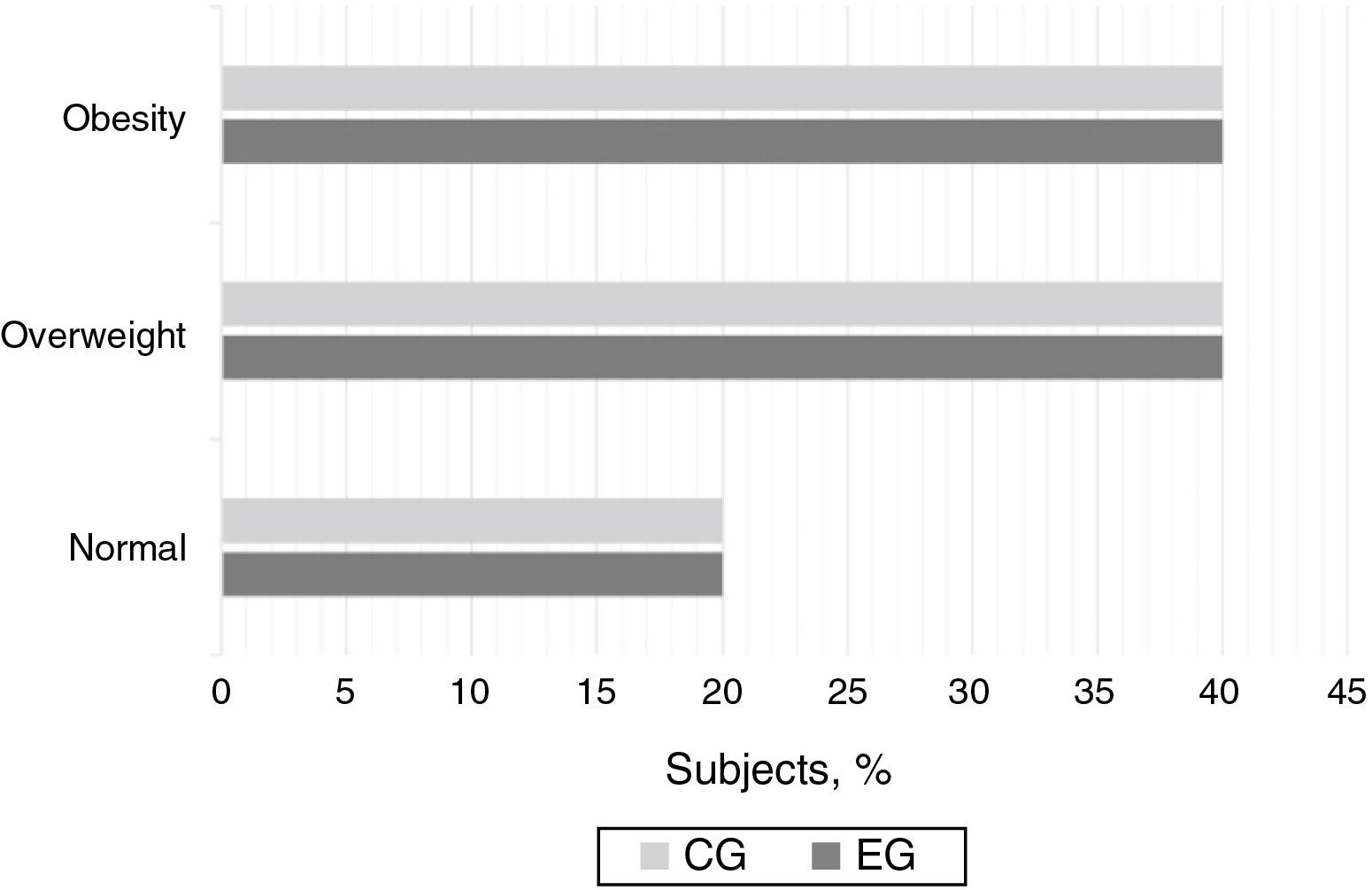
Subjects’ body mass index (BMI) was calculated as weight in kg divided by height in m squared and was classified as normal (18.5–24.9), overweight (25–29.9) or obese (≥30).6,26
Measurements on the bioimpedance scale were taken with the subjects without shoes, wearing as little clothing as possible and with no metal objects. They had also been told not to consume alcohol, caffeine or heavy meals in the 24 hours before the assessment, to urinate half an hour before weighing and to avoid strenuous exercise in the four hours before.22,26
Waist circumference was measured with the subjects positioned with their arms by their sides and feet shoulder-width apart at the mid-point between the lowest rib and the iliac crest.26
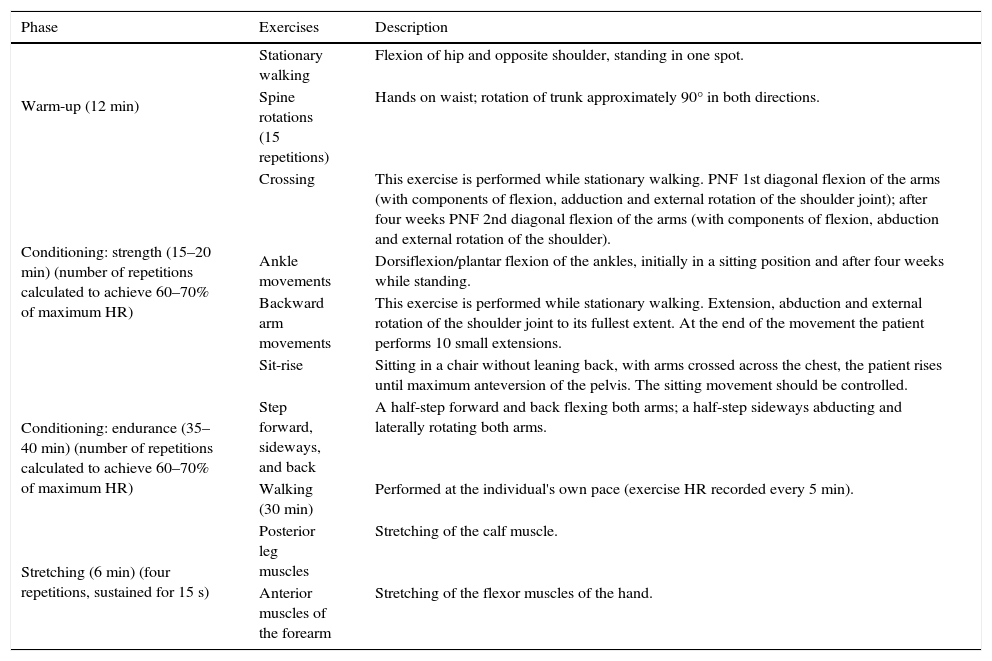
The exercise protocol (Table 2) consisted of 10 exercises and was divided into the following stages: warm-up, conditioning and cool-down.27,28 The exercises were taught during individual face-to-face sessions, backed up by illustrated leaflets to help participants to perform the protocol at home.
Organization and description of the exercise protocol.
| Phase | Exercises | Description |
|---|---|---|
| Warm-up (12 min) | Stationary walking | Flexion of hip and opposite shoulder, standing in one spot. |
| Spine rotations (15 repetitions) | Hands on waist; rotation of trunk approximately 90° in both directions. | |
| Conditioning: strength (15–20 min) (number of repetitions calculated to achieve 60–70% of maximum HR) | Crossing | This exercise is performed while stationary walking. PNF 1st diagonal flexion of the arms (with components of flexion, adduction and external rotation of the shoulder joint); after four weeks PNF 2nd diagonal flexion of the arms (with components of flexion, abduction and external rotation of the shoulder). |
| Ankle movements | Dorsiflexion/plantar flexion of the ankles, initially in a sitting position and after four weeks while standing. | |
| Backward arm movements | This exercise is performed while stationary walking. Extension, abduction and external rotation of the shoulder joint to its fullest extent. At the end of the movement the patient performs 10 small extensions. | |
| Sit-rise | Sitting in a chair without leaning back, with arms crossed across the chest, the patient rises until maximum anteversion of the pelvis. The sitting movement should be controlled. | |
| Conditioning: endurance (35–40 min) (number of repetitions calculated to achieve 60–70% of maximum HR) | Step forward, sideways, and back | A half-step forward and back flexing both arms; a half-step sideways abducting and laterally rotating both arms. |
| Walking (30 min) | Performed at the individual's own pace (exercise HR recorded every 5 min). | |
| Stretching (6 min) (four repetitions, sustained for 15 s) | Posterior leg muscles | Stretching of the calf muscle. |
| Anterior muscles of the forearm | Stretching of the flexor muscles of the hand. |
HR: heart rate; PNF: proprioceptive neuromuscular facilitation.
The exercise protocol was intended to be of moderate intensity, and so the exercises began at 60% of the maximum heart rate attained in exercise testing following the Bruce protocol and progressed to 70%. The home-based CR program was designed to last two months, with at least three sessions a week. Initial training in the exercise protocol and fortnightly face-to-face meetings took place in the outpatient clinic of Centro Hospitalar de Vila Nova de Gaia. Progress in the exercises was monitored after four weeks, participants being assessed individually in terms of exercise heart rate and Borg exertion scale.27,29 These sessions emphasized the importance of subjects self-monitoring their home-based exercise program by means of the Borg scale and measuring heart rate at the radial pulse at the end of each exercise and every 5 min during the walking component. The home-based CR program was monitored remotely every week through text messages, telephone calls or email and by fortnightly face-to-face meetings, in order to encourage adherence to the exercise program and to clarify any questions the participants might have had concerning the exercises or the Mediterranean diet.
EthicsThe trial was approved by the Ethics Committee of Centro Hospitalar de Vila Nova de Gaia (166/2011) and registered at ClinicalTrials.gov (NCT01887080). The participants were informed of the study's aims and procedures and provided written consent in accordance with the Declaration of Helsinki (1964).
Patients in the control group were given the opportunity to undertake the exercise program after the trial ended.
Statistical analysisThe analysis was performed using the software package PASW® Statistics version 20 (IBM Corporation, Somers, NY) for Windows 7®, for a level of significance of 0.05 and 95% confidence interval.30
The sample was characterized by descriptive statistics using medians as a measure of central tendency and interquartile deviation as a measure of dispersion.30
Non-parametric statistics were used, comparing EG and CG at T0 and T1 with the Mann-Whitney test for continuous variables and Fisher's exact test for categorical variables. Comparison within groups (between T0 and T1) was performed using Wilcoxon's test.30
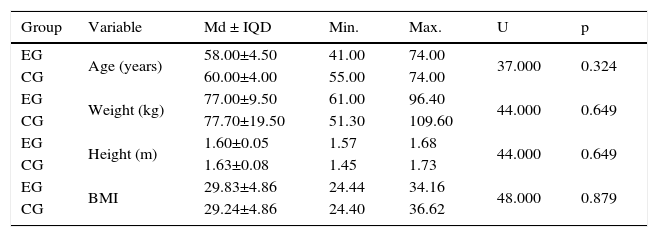
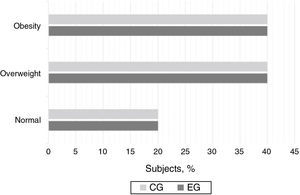
ResultsBoth the EG and the CG consisted of four females and six males. Age, weight, height and BMI at T0 are shown in Table 3. There were no statistically significant differences between the groups at T0.
Median, interquartile deviation, minimum and maximum of age and anthropometric variables at the initial time point of the study in the experimental group (n=10) and the control group (n=10).
| Group | Variable | Md ± IQD | Min. | Max. | U | p |
|---|---|---|---|---|---|---|
| EG | Age (years) | 58.00±4.50 | 41.00 | 74.00 | 37.000 | 0.324 |
| CG | 60.00±4.00 | 55.00 | 74.00 | |||
| EG | Weight (kg) | 77.00±9.50 | 61.00 | 96.40 | 44.000 | 0.649 |
| CG | 77.70±19.50 | 51.30 | 109.60 | |||
| EG | Height (m) | 1.60±0.05 | 1.57 | 1.68 | 44.000 | 0.649 |
| CG | 1.63±0.08 | 1.45 | 1.73 | |||
| EG | BMI | 29.83±4.86 | 24.44 | 34.16 | 48.000 | 0.879 |
| CG | 29.24±4.86 | 24.40 | 36.62 |
BMI: body mass index; CG: control group; EG: experimental group; IQD: interquartile deviation; Max.: maximum; Md: median; Min.: minimum.
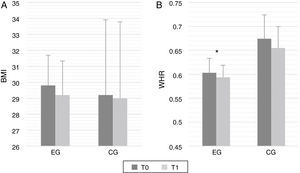
Around 80% of subjects in both groups had a BMI above normal (Figure 2), while WHR was over 0.5 in all individuals.
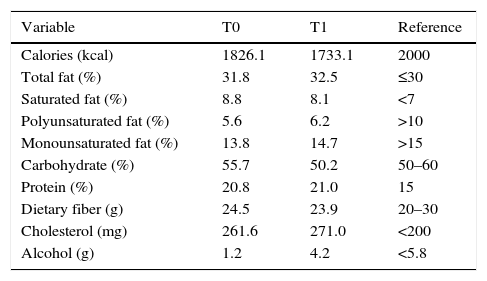
Table 4 presents reference values for the variables analyzed in the FFQ and the values in the present study at T0 and T1.
Reference values for the variables analyzed in the food frequency questionnaire8 and the values at the beginning and end of the study.
| Variable | T0 | T1 | Reference |
|---|---|---|---|
| Calories (kcal) | 1826.1 | 1733.1 | 2000 |
| Total fat (%) | 31.8 | 32.5 | ≤30 |
| Saturated fat (%) | 8.8 | 8.1 | <7 |
| Polyunsaturated fat (%) | 5.6 | 6.2 | >10 |
| Monounsaturated fat (%) | 13.8 | 14.7 | >15 |
| Carbohydrate (%) | 55.7 | 50.2 | 50–60 |
| Protein (%) | 20.8 | 21.0 | 15 |
| Dietary fiber (g) | 24.5 | 23.9 | 20–30 |
| Cholesterol (mg) | 261.6 | 271.0 | <200 |
| Alcohol (g) | 1.2 | 4.2 | <5.8 |
T0: initial time point; T1: final time point.
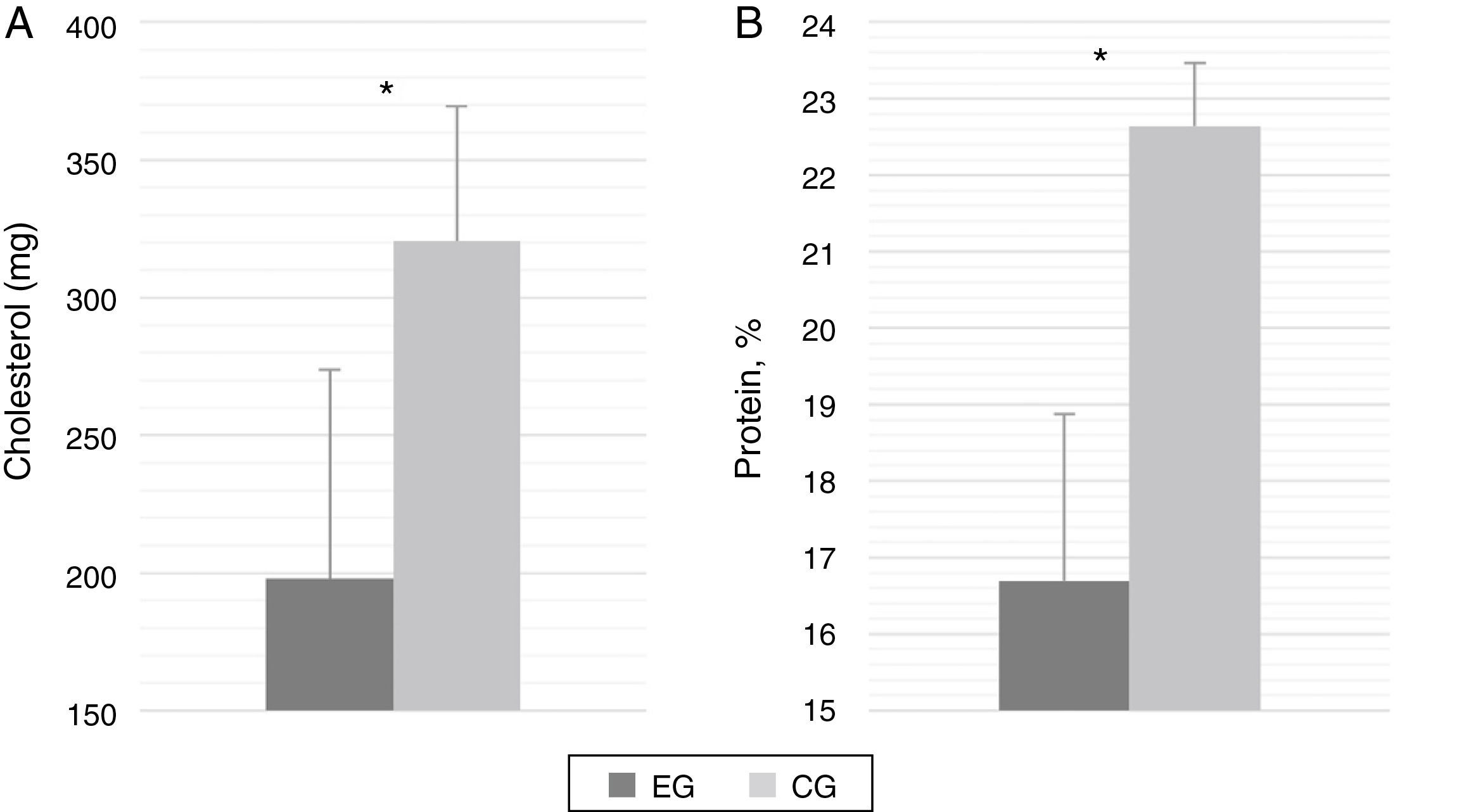
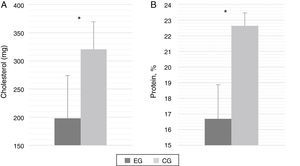
There were no statistically significant differences between the groups in the variables analyzed by the FFQ at T0, but after eight weeks there were significant falls in the EG in intake of protein (p=0.025; U=20.000) and cholesterol (p=0.025; U=20.000) (Figure 3).
There were no significant differences in intake of carbohydrate or saturated fat in the EG between T0 and T1, but significant reductions in these parameters were seen in the CG (p=0.008; Z=−2.505 and p=0.008; Z=−2.505, respectively).
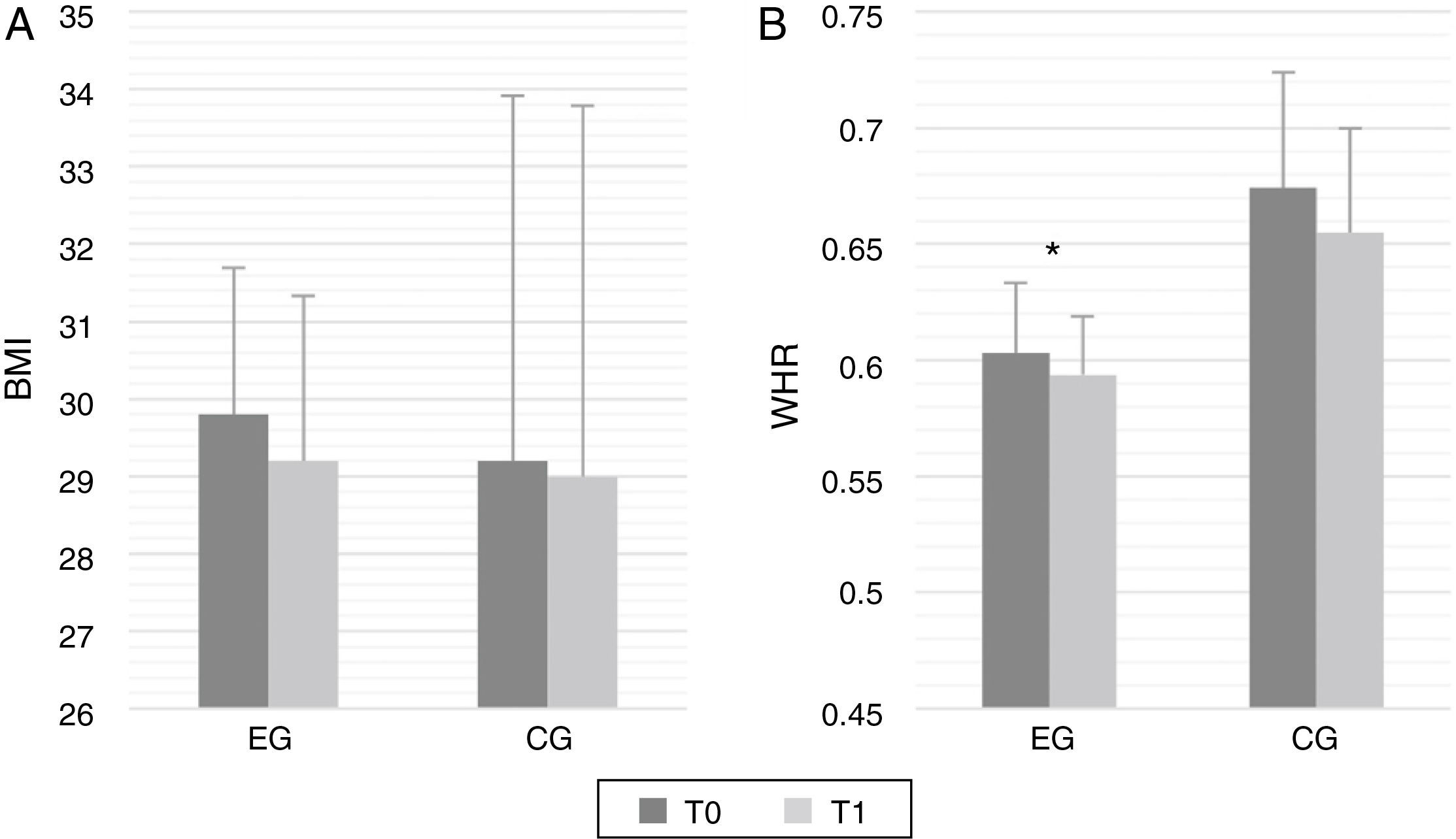
With regard to BMI and WHR, there were no significant differences between the groups at either T0 or T1. WHR decreased significantly in the EG over the course of the trial (p=0.08; Z=−2.505), but no significant changes were seen in BMI (Figure 4).
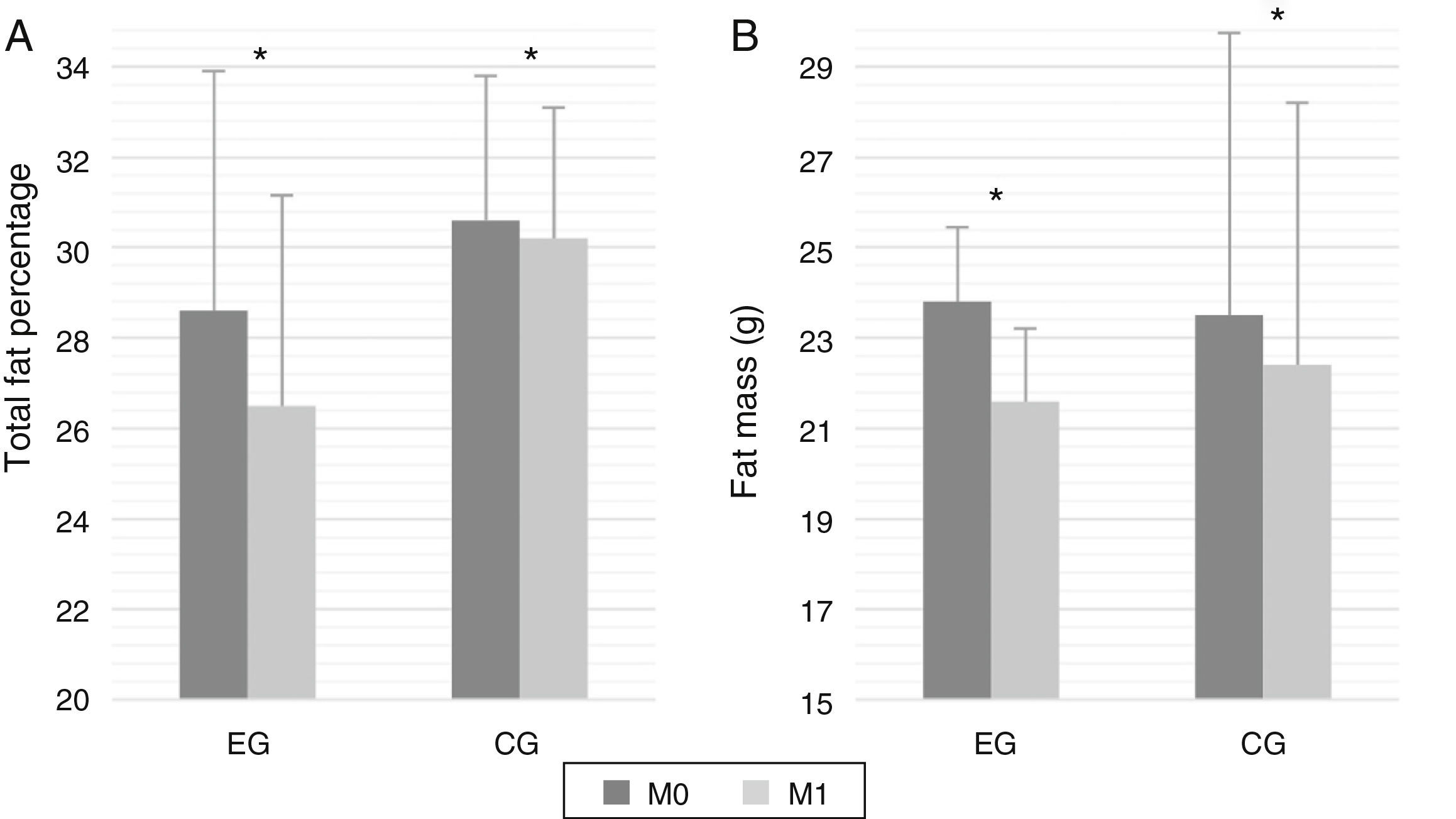
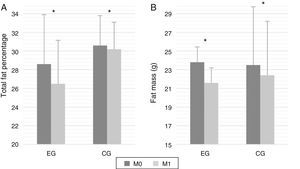
Body composition as shown by bioimpedance did not differ significantly between the two groups at either time point. At the end of the study a significant reduction was seen in total fat percentage in both the EG (p=0.008; Z=−2.558) and the CG (p=0.002; Z=−2.812) (Figure 5A) and in fat mass (p=0.002; Z=−2.827 and p=0.008; Z=−2.519, respectively) (Figure 5B). No changes were seen in lean mass.
The eight-week exercise program consisted of a minimum of 24 sessions (three per week), with a maximum of 36 (up to seven per week); 65% of participants only completed the minimum of 24 sessions.
DiscussionThe large number of patients excluded from the study before randomization was due to the fact that this home-based CR program was intended for patients at low cardiovascular risk who had to be safely monitored remotely while remaining in active control. Furthermore, individuals with comorbidities that could have limited their ability to perform the exercise protocol correctly were also excluded.
The FFQ demonstrated that daily nutrient intake in the study population did not meet recommended levels for a healthy diet, particularly with regard to fat intake. Before the education sessions on the Mediterranean diet, consumption of cholesterol, protein, total fat and saturated fat was excessive, while monounsaturated and polyunsaturated fat consumption was less than recommended. Although most studies focus on individual nutrients, various patterns of eating habits can affect cardiovascular risk and its main risk factors. The Mediterranean diet provides a wide range of nutrients and improves energy balance, thereby reducing cardiovascular risk. This means that rather than focusing on specific nutrients or foods, individuals should aim to improve their diet as a whole.31
Protein and cholesterol intake decreased significantly in the EG compared to the CG, approaching recommended values, after the eight-week exercise program. Recent studies suggest that exercise activates leptin receptor-positive neurons in the ventromedial hypothalamic nucleus, involved in homeostatic control of energy balance, which would explain why exercise increases postprandial satiation.32,33 Another possible explanation is the motivational factor of following a CR program, which gives added incentive to adopt healthy eating habits.
In the present study, there was a significant reduction in carbohydrate and saturated fat intake in those who only attended the education sessions over a two-month period on the Mediterranean diet. This illustrates the importance of including these dietary recommendations in CR programs, in agreement with World Health Organization guidelines for limiting saturated fat intake, given its demonstrated link with cardiovascular disease. The Mediterranean diet has been shown to reduce cardiovascular events and risk factors such as dyslipidemia, hypertension, diabetes and insulin resistance.34
Another point to note is the tendency for total fat intake to increase over the course of the study, but this was the result of increased consumption of monounsaturated and polyunsaturated fat, while saturated fat intake fell, in accordance with recommendations for a healthy diet.
BMI values did not change significantly over the course of the study in either group, but a significant reduction in WHR was seen in the EG, highlighting the importance of associating the Mediterranean diet with exercise for secondary prevention in cardiovascular patients.35 The exercise protocol in this study achieved its purpose, showing that the association of exercise and the Mediterranean diet is more effective than diet modification by itself. This home-based phase IV CR program was intended to promote long-term maintenance of activity levels and behaviors developed during phase III, as well as to encourage lifestyle changes, based on empowerment, the process by which people gain control over the factors and decisions that shape their lives.36
Nevertheless, by the end of the study over 50% of the EG still had a WHR of >0.5, associated with increased cardiovascular risk. This may be due to the short duration of the study (eight weeks) and variation in the number of sessions completed.24–36
The changes observed in body composition in both groups demonstrate the effectiveness of the Mediterranean diet in reducing fat mass. Such changes appear to be due to the lower intake of saturated fatty acids and hydrogenated fat and the higher consumption of monounsaturated fatty acids in this diet, reflecting reduced consumption of animal fat and greater consumption of nuts and vegetable margarine. Depending on energy status, monounsaturated fatty acids are more rapidly oxidized than saturated fatty acids, which increases the use of fatty acids by muscles, reducing the accumulation found with saturated fat and thereby lowering the risk of obesity.37,38 The role of adipose tissue in the production and secretion of a wide range of inflammatory molecules is well documented, and it has been shown that weight loss, particularly of fat mass, reduces macrophage infiltration and thereby improves the inflammatory profile.39 However, in our study there was a greater reduction of fat mass in the EG after eight weeks, which could be due to the effect of exercise on lipolysis of adipocytes and use of fatty acids. In-vitro studies indicate that exercise reduces adipocyte size, an effect that does not appear to be produced by dietary restriction alone.40,41
The quantity of lean mass did not alter in either group, which may be due to the controlled and moderate intake of vegetable protein and, in the case of the EG, the association with endurance training, which could have reduced age-related muscle loss.27,28
Although the benefits of CR programs are well known, the exercise component can be problematic, with low rates of adherence and high dropout rates.42 In the present study, three participants did not adhere to the program and one was excluded due to failure to attend sessions. In the EG, 65% of subjects completed only the minimum number of sessions (three per week). The reasons given by participants were lack of time due to work commitments and weather conditions affecting the walking component.
The small sample size is a limitation of the present study, and larger studies should be performed. Future studies should also include a structured dietary plan for each participant based on calculation of energy requirements and the corresponding distribution of the macronutrients of the Mediterranean diet.
ConclusionEncouragement to follow the Mediterranean diet in individuals with known coronary heart disease was shown to change eating behaviors, with reduced intake of carbohydrate and saturated fat, reflected in lower fat mass. However, the addition of a home-based exercise program was associated with reduced protein and cholesterol intake and decreased fat mass and abdominal fat.
The study therefore appears to support the idea that recommending the Mediterranean diet in order to modify dietary behaviors, together with regular programmed exercise, in patients with coronary heart disease on a phase IV CR program can minimize the risk of developing metabolic disorders and hence reduce cardiovascular risk.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors thank the department of nutritional epidemiology at the University of Porto for their assistance in processing the data from the FFQ, and Dr. Bianca Castro for reviewing the content of the Mediterranean diet.
Please cite this article as: Noites A, Pinto J, Freitas CP, et al. Efeitos da dieta mediterrânica e exercício físico em indivíduos com doença arterial coronária. Rev Port Cardiol. 2015;34:655–664.