Cardiac rehabilitation (CR) programs have a central role in cardiovascular medicine, encompassing a comprehensive framework able to holistically address various facets of cardiovascular disease. However, several obstacles to their optimal application have been reported. Over the years, the Portuguese Society of Cardiology has periodically conducted a national survey on the state of CR in Portugal.
ObjectivesThis study reports the results of the 2019 survey on CR.
MethodsIn December 2019 a voluntary questionnaire was sent to centers offering CR programs, consisting of several items concerning this intervention.
ResultsIn 2019, 25 centers provided structured CR programs. A total of 2182 patients underwent phase II programs, representing an increase of 13% from the previous survey. Of these, 67.2% were referred due to ischemic heart disease, and 14.5% due to heart failure. Acute coronary syndromes (ACS) comprised 49.3% of referrals, leading to an estimated 9.3% CR coverage. A total of 606 patients participated in phase III programs (a decrease of 37%). Drop-out rates ranged from 0-68%; 91% of centers presented drop-out rates <25%.
ConclusionThe present survey shows an increase in the number of centers and patients undergoing phase II CR, and an increase in the estimated CR coverage after ACS. Despite this, the level of increase means that overall patient representation remained below the optimal range, while the data also showed a decrease in the number of patients in phase III programs. These findings reinforce the importance of optimization of CR entry and maintenance, in order to improve the uptake of this pivotal intervention.
A reabilitação cardíaca (RC) apresenta um papel central na medicina cardiovascular. Contudo, diversos obstáculos à sua aplicação têm sido descritos. Ao longo dos anos, a Sociedade Portuguesa de Cardiologia tem realizado um inquérito nacional referente ao estado da RC em Portugal.
ObjetivosO presente estudo apresenta os resultados do questionário nacional de 2019.
MétodosEm dezembro de 2019 um questionário voluntário englobando itens relacionados com esta intervenção foi enviado aos centros que apresentavam programas de RC.
ResultadosEm 2019, vinte e cinco centros apresentavam programas estruturados de RC. Um total de 2 182 indivíduos participou em programas de fase II de RC, representando um acréscimo de 13% face ao último inquérito. Destes, 67,2% foram referenciados por doença cardíaca isquémica e 14,5% por insuficiência cardíaca. As síndromas coronárias agudas (SCA) representaram 49,3% das referenciações, com uma cobertura estimada de 9,3%. Um total de 606 doentes participou em programas de fase III (um decréscimo de 37%). As taxas de desistência variaram entre 0-68%; 91% dos centros apresentaram taxas de desistência < 25%.
ConclusãoO presente inquérito demonstra um aumento no número de centros e de doentes a participarem em programas de fase II de RC, com um aumento da cobertura estimada após SCA. Apesar destes resultados, a representação mantém-se abaixo dos valores ótimos, sendo que os dados demonstram uma redução no número de doentes em programas de fase III. Estes resultados reforçam a importância da otimização da inclusão em programas de RC e compliance, por forma a permitir uma maior implantação desta intervenção.
Cardiovascular disease (CVD) is a significant cause of morbidity and mortality.1,2 Although significant advances have been made in terms of prevention, diagnosis, and overall management, leading to improved outcomes, CVD still represents an important healthcare burden.1–4 As such, optimized prevention measures across the cardiovascular continuum are of pivotal importance.3,4 In this context, cardiac rehabilitation (CR) programs play a central role in contemporary cardiovascular medicine.3,4 Although exercise training (ET) is a critical component of this intervention, over the years CR programs have evolved into a broadly multidisciplinary and multi-layered framework, providing a holistic and integrative approach to the complex cardiovascular patient.4–7 As well as ET, some of the core components of these structured programs presently include the identification and control of cardiovascular (CV) risk factors as well as overall therapeutic optimization and counseling regarding adherence, nutritional assessment, smoking cessation counseling, psychological assessment and intervention, and educational sessions, as well as other ancillary interventions such as socioeconomic support and vocational advice.5,6,8
Several publications have reported extensively on the plethora of beneficial effects associated with structured CR programs in terms of morbidity and mortality, especially in the setting of ischemic heart disease (IHD),9–11 and also on parameters such as control of CV risk factors, functional capacity and quality of life.12–15 Given these data, current guidelines on different CV diseases such as IHD and heart failure (HF) strongly support the use of CR, which is a class I, level A recommendation in these two settings, as a pivotal aspect of optimal patient management.3,4,16–18 While their role across a broad range of CVD is presently consensual, several obstacles to the optimal application of CR programs have also been described. Among these are differences in program design, as well as suboptimal patient representation (particularly among certain subgroups such as the elderly, women, and those living far from healthcare centers) and adherence.4,10,19,20
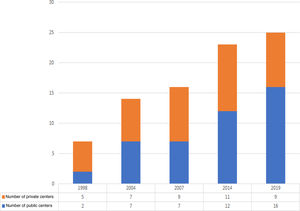
Over the course of the last two decades, the Working Group on Exercise Physiology and Cardiac Rehabilitation of the Portuguese Society of Cardiology (SPC) has periodically assessed the state of CR in Portugal, by performing a national survey.8,21–23 Initially carried out in 1998 and subsequently updated in 2004, 2007 and 2013-14, this survey has enabled the growth of this intervention in Portugal to be analyzed and tracked, as well as providing an important and pragmatic insight into its most central challenges. This paper presents the results of the 2019 national survey on CR, and compares some of its indicators with previous results, in order to provide an overview of the current state of CR in Portugal.
MethodsIn December 2019 a voluntary questionnaire was sent to all centers offering CR programs, including the following items: general information on the center, including name, location, type (public or private institution), and year of CR program inception, composition of the team and its coordinators, description of the CR phases offered (i.e. phases I, II and III), program components, total number of participants and distribution by diagnosis in 2019, drop-out rate, and associated reasons for lack of adherence. In addition, a description of the main factors concerning patient enrollment and maintenance in the program was also requested.
The responses were analyzed and compared with the results of the previous surveys.
ResultsCardiac rehabilitation centersAccording to the present survey, a total of twenty-five centers offered structured CR programs in Portugal in 2019 (Table 1). Of these, 11 were in the North region, one in the Central region, twelve in the Greater Lisbon region and one in the South region. Compared to the previous survey,8 there were six new centers. Of these, five were public – Centro Hospitalar Universitário de Lisboa Norte (Hospital de Santa Maria)/Faculdade de Medicina da Universidade de Lisboa, Centro de Reabilitação Cardiovascular da Universidade de Lisboa, Centro Hospitalar de Lisboa Ocidental (Hospital de Santa Cruz), Centro Hospitalar de Leiria, and Centro Hospitalar de Trás-os-Montes e Alto Douro – and one was private (Instituto CUF). Compared to the previous survey, four centers had discontinued CR programs – one public (Hospital de Vila Franca de Xira) and three private (Clínica Dr. Dídio de Aguiar, Instituto de Cardiologia Preventiva de Almada, and Clínica da Cruz Vermelha – Sabrosa).
Cardiac rehabilitation centers in Portugal, 2019.
| Center | Location | Start of activity (year) | Coordinator | |
|---|---|---|---|---|
| Public centers | ||||
| Hospital das Forças Armadas, Pólo de Lisboa | Lisbon | 1988 | Conceição Silveira | Cardiologist |
| Centro Hospitalar de Vila Nova de Gaia/Espinho (Hospital de Gaia) | Vila Nova de Gaia | 1993 | Madalena TeixeiraFátima Miranda | CardiologistPhysiatrist |
| Centro Hospitalar de Vila Nova de Gaia/Espinho (Centro de Reabilitação do Norte) | Vila Nova de Gaia | 2016 | Sofia ViamonteMadalena Teixeira/Eduardo Vilela | PhysiatristCardiologists |
| Centro Hospitalar Universitário do Porto (Hospital de Santo António) | Porto | 2000 | Preza FernandesSandra Magalhães | CardiologistPhysiatrist |
| Centro Hospitalar Entre Douro e Vouga (Hospital de São Sebastião) | Santa Maria da Feira | 2001 | Luís Martins/Fernando PintoCatarina Aguiar Branco | CardiologistsPhysiatrist |
| Unidade Local de Saúde de Matosinhos (Hospital de Pedro Hispano) | Matosinhos | 2001 | Paula Almeida | Physiatrist |
| Centro Hospitalar Universitário de Lisboa Central (Hospital de Santa Marta) | Lisbon | 2004 | Pedro RioJorge DiasVítor Ferreira | CardiologistPhysiatristRehabilitation nurse |
| Centro Hospitalar Universitário de São João | Porto | 2008 | Afonso RochaVítor Araújo/Paula Dias | PhysiatristCardiologists |
| Centro Hospitalar Universitário do Algarve (Hospital de Faro) | Faro | 2012 | Salomé Pereira | Cardiologist |
| Hospital Beatriz Ângelo | Loures | 2013 | Duarte Espregueira Mendes | Cardiologist |
| Centro Hospitalar Universitário de Lisboa Norte/Faculdade de Medicina da Universidade de Lisboaa | Lisbon | 2014 | Ana Abreu | Cardiologist |
| Centro de Reabilitação Cardiovascular da Universidade de Lisboa (CRECUL)b | Lisbon | 2016 | Ana AbreuHelena Santa-Clara | CardiologistExercise physiologist |
| Hospital Garcia de Orta | Almada | 2014 | Luísa BentoSofia Bento | CardiologistPhysiatrist |
| Centro Hospitalar de Lisboa Ocidental (Hospital de Santa Cruz) | Lisbon | 2016 | Miguel Mendes/Anaí DurazzoOlga Galvão/Sofia Santos | CardiologistsPhysiotherapists |
| Centro Hospitalar de Leiria | Leiria | 2017 | Alexandra Antunes | Cardiologist |
| Centro Hospitalar de Trás-os-Montes e Alto Douro (Hospital de Vila Real) | Vila Real | 2018 | José Paulo Fontes | Cardiologist |
| Private centers | ||||
| Instituto do Coração | Lisbon | 1988 | Miguel MendesAna Adegas | CardiologistPhysiotherapist |
| Faculdade de Motricidade Humana (CORLIS) | Lisbon | 1991 | Miguel MendesHelena Santa-Clara | CardiologistExercise physiologist |
| Fisimaia | Maia | 1992 | José Paulo FontesEunice Vouga | CardiologistPhysiatrist |
| Diprofisio | Porto | 1993 | Madalena TeixeiraAna Ramalhão | CardiologistPhysiotherapist |
| SAMS | Lisbon | 2004 | Ana AbreuCecília Vaz Pinto | CardiologistPhysiatrist |
| Clínica Fisiatria MCCB Drª. Maria do Carmo Aguiar Branco | Vila Nova de Gaia | 2007 | Marlene FonsecaCatarina Aguiar Branco | CardiologistPhysiatrist |
| Clínica das Conchas | Lisbon | 2007 | Jorge Ruivo | Internist |
| Hospital da Luz | Lisbon | 2010 | Daniel FerreiraPaloma Valdívia | CardiologistPhysiatrist |
| Instituto CUF | Porto | 2019 | Afonso Rocha | Physiatrist |
An increase in the number of CR centers was seen compared to previous data, with progressive growth since the first survey8,21–23 (Figure 1). Although asymmetries between regions persisted, unlike in the previous report the Central region now had one CR center (Centro Hospitalar de Leiria) (Table 1).
Team composition and program coordinationAs in the previous survey, all centers reported multidisciplinary teams, all of which included a cardiologist (Table 2). In the present survey, physiatrists were involved in 80% of CR programs (an increase of 6% compared to the previous survey) (Table 2).8 A total of 68% of CR programs reported the involvement of other healthcare professionals (among them pulmonologists, endocrinologists, internists, vascular surgeons, and social care workers).
Joint coordination by both a cardiologist and a physiatrist was most frequent (40%), followed by coordination by a cardiologist (24%). Other combinations of coordinators are depicted in Table 1.
Program phases and componentsAccording to the present survey, 12 centers (all public) provided phase I programs, and 22 provided phase II programs, as compared to nine and 21, respectively, in 2014.8 Analyzing only centers that provided formal ET sessions as part of their design, a total of 13 centers provided phase III programs (a comparable figure to the previous survey).8 It should be noted that although for the present analysis only programs providing formal ET sessions as part of phase III CR were described, other centers reported providing overall clinical assessment (of varying types) and lifestyle guidance (including exercise) as part of the long-term maintenance phase, similar to the results in the previous survey.8
Program design and duration varied in terms of the number of ET sessions per week and total program duration, although most phase II CR programs included two to three sessions per week, for 24-36 sessions (Table 3). For phase III CR programs (including only those with formal ET sessions), designs ranged from one to three sessions per week, with the option for long-term maintenance in some programs (Table 3).
Design of exercise training sessions for phases II and III of cardiac rehabilitation programs.
| Center | Phase II design (number of ET sessions) | Phase III design (number of ET sessions) |
|---|---|---|
| Hospital das Forças Armadas, Pólo de Lisboa | 3 times/week; 36 sessions | – |
| Centro Hospitalar de Vila Nova de Gaia/Espinho (Hospital de Gaia) | 2-3 times/week; 24-36 sessions | – |
| Centro Hospitalar de Vila Nova de Gaia/Espinho (Centro de Reabilitação do Norte) | 2 times/week; 8-24 sessions | 2 times/week; 8-24 sessions |
| Centro Hospitalar Universitário do Porto (Hospital de Santo António) | 2 times/week; 12-24 sessions | – |
| Centro Hospitalar Entre Douro e Vouga (Hospital de São Sebastião) | 2-3 times/week; 24-48 sessions | 1-2 times/week; 4-24 sessions |
| Unidade Local de Saúde de Matosinhos (Hospital de Pedro Hispano) | 2 times/week; 12-24 sessions | – |
| Centro Hospitalar Universitário de Lisboa Central (Hospital de Santa Marta) | 2 times/week; 32 sessions | 2 times/week; 48 sessions |
| Centro Hospitalar Universitário de São João | 2 times/week; 16-24 sessions | – |
| Centro Hospitalar Universitário do Algarve(Hospital de Faro) | 3 times/week; 24-36 sessions | – |
| Hospital Beatriz Ângelo | 2-3 times/week; 16-48 sessions | – |
| Centro Hospitalar Universitário de Lisboa Norte/Faculdade de Medicina da Universidade de Lisboaa | 2-3 times/week; 24-36 sessions | – |
| Centro de Reabilitação Cardiovascular da Universidade de Lisboa (CRECUL) | – | 3 times/week |
| Hospital Garcia de Orta | 3 times/week; 32 sessions | NS |
| Centro Hospitalar de Lisboa Ocidental (Hospital de Santa Cruz) | 2-3 times/week; 20-40 sessions | <1 time/week; 8-10 sessions |
| Centro Hospitalar de Leiria | 2 times/week; 24 sessions | – |
| Centro Hospitalar de Trás-os-Montes e Alto Douro (Hospital de Vila Real) | 3 times/week; 24 sessions | – |
| Instituto do Coração | 3 times/week; 24-36 sessions | ≤3 times/week |
| Faculdade de Motricidade Humana – CORLIS | – | 3 times/week |
| Fisimaia | 2 times/week; 24 sessions | 2 times/week |
| Diprofisio | 2-3 times/week; 24-36 sessions | 2 times/week |
| SAMS | 3 times/week; 36 sessions | – |
| Clínica Fisiatria MCCB Drª. Maria do Carmo Aguiar Branco | 2 times/week; 24-48 sessions | 1-2 times/week; 4-24 sessions |
| Clínica das Conchas | – | 2 times/week; 48 sessions |
| Hospital da Luz | 3 times/week; 36 sessions | – |
| Instituto CUF | 2 times/week; 12 sessions | 2 times week; 12 sessions |
ET: exercise training; NS: not specified.
Other program components in addition to ET (present in all CR programs) are reported in Table 4.
Components of cardiac rehabilitation programs.
| Component | Percentage of CR programs |
|---|---|
| Exercise | 100% |
| Nutritional counseling | 100% |
| Specific program | 52%; 16% NS |
| Appointment with a dietitian/nutritionist | 32% all patients; 52% some patients; 12% NS |
| CV risk factor management | |
| Dyslipidemia management | 92%; 4% NS |
| Hypertension management | 96%; 4% NS |
| Smoking cessation counseling | 88%; 8% NS |
| Specific program | 36%; 12% NS |
| Specific appointment with a specialist | 8% all patients; 64% some patients; 24% NS |
| Psychosocial assessment | 68%; 8% NS |
| Specific program | 56%; 16% NS |
| Appointment with a psychiatrist/psychologist | 16% all patients; 52% some patients; 28% NS |
| Vocational counseling | 48%; 8% NS |
| Sexual counseling | 48%; 8% NS |
CR: cardiac rehabilitation; CV: cardiovascular; NS: not specified.
In 2019, a total of 2182 patients were included in phase II CR programs (Table 5). The number of patients included increased by 13% compared to the previous survey. Of these, 93% (2031 patients) attended public centers. Assessment of previous surveys8,23 shows that the number of patients participating in phase II CR programs in public centers presented an increasing trend (71% in 2007, 86% in 2013, and 93% in the present survey).
Numbers of participants in cardiac rehabilitation programs in Portugal, 2019.
| Center | Phase II: number of patients referred due to ACS/total number of patients | Phase III: total number of patients |
|---|---|---|
| Hospital das Forças Armadas, Pólo de Lisboa | 6/8 | – |
| Centro Hospitalar de Vila Nova de Gaia/Espinho (Hospital de Gaia) | 160/252 | – |
| Centro Hospitalar de Vila Nova de Gaia/Espinho (Centro de Reabilitação do Norte) | 16/77 | 9 |
| Centro Hospitalar Universitário do Porto (Hospital de Santo António) | 164/282 | – |
| Centro Hospitalar Entre Douro e Vouga (Hospital de São Sebastião) | 130/645 | 254 |
| Unidade Local de Saúde de Matosinhos (Hospital de Pedro Hispano) | 57/104 | – |
| Centro Hospitalar Universitário de Lisboa Central (Hospital de Santa Marta) | 34/47 | 3 |
| Centro Hospitalar Universitário de São João | 121/188 | – |
| Centro Hospitalar Universitário do Algarve (Hospital de Faro) | 28/29 | – |
| Hospital Beatriz Ângelo | 43/66 | – |
| Centro Hospitalar Universitário de Lisboa Norte/Faculdade de Medicina da Universidade de Lisboaa | 58/79 | – |
| Centro de Reabilitação Cardiovascular da Universidade de Lisboa (CRECUL)b | – | 87 |
| Hospital Garcia de Orta | 79/85 | NS |
| Centro Hospitalar de Lisboa Ocidental (Hospital de Santa Cruz) | 46/100 | 102 |
| Centro Hospitalar de Leiria | 34/36 | – |
| Centro Hospitalar de Trás-os-Montes e Alto Douro (Hospital de Vila Real) | 33/33 | – |
| Instituto do Coração | 7/22 | 14 |
| Faculdade de Motricidade Humana – CORLIS | – | 25 |
| Fisimaia | 4/10 | 31 |
| Diprofisio | 4/6 | 19 |
| SAMS | 19/20 | – |
| Clínica Fisiatria MCCB Drª. Maria do Carmo Aguiar Branco | 20/59 | 59 |
| Clínica das Conchas | – | 3 |
| Hospital da Luz | 6/14 | – |
| Instituto CUF | 7/20 | – |
| Total | 1076/2182 | 606 |
ACS: acute coronary syndromes; NS: not specified.
A total of 606 patients were included in phase III CR programs (Table 5). A decrease of 37% in the number of patients undergoing these programs was seen compared to the previous survey.8 Most patients were treated in public centers (75%), similarly to the previous survey (75% in 2013).8
Twenty-three centers reported data on drop-out rates, which ranged from 0% to 68%. Notably, 91% of CR programs presented drop-out rates of less than 25%. Among the motives reported for lack of adherence to the program were difficulties with transportation, distance between the center and the patient's residence, financial constraints, lack of family support, lack of interest or motivation, fear of ET and unawareness of its benefits, comorbidities and work-related issues. Some of the major difficulties reported by the centers concerning CR entry and maintenance were the center's limited capacity to include more patients (especially due to limitations in terms of facilities and/or healthcare professionals) and low referral rates, as well as the motives described above for lack of adherence (with the exception of fear of ET and unawareness of its benefits).
IHD was the most common referral indication for phase II CR programs (Tables 5 and 6). This was responsible for 67.2% of referrals for phase II CR programs when acute coronary syndromes (ACS), elective percutaneous coronary interventions, coronary surgery, and chronic coronary syndromes were pooled (Table 5). Specifically, ACS were responsible for 49.3% of phase II CR referrals, similarly to the previous two surveys, in which myocardial infarction (MI) was reported in 51.8% of patients in 2013, and 50% in 2007.8,23 HF was the second most common referral indication, and the primary reason for referral in 14.5% of cases, thus continuing the increasing trend reported in the previous survey, in which it represented 12.7% of referrals.8,23
Distribution of participants by diagnosis in phases II and III cardiac rehabilitation programs.
| Main indication for referral | Phase II | Phase III |
|---|---|---|
| ACS | 49.3% | 28.5% |
| Elective PCI | 2.9% | 0.8% |
| CABG | 10.2% | 11.7% |
| Chronic coronary syndrome | 4.8% | 14.4% |
| Heart valve surgery/percutaneous valvular intervention | 5.6% | 4.6% |
| Heart failure | 14.5% | 19.8% |
| Heart transplantation | 0.1% | 0.5% |
| CV factor management | 2.8% | 6.9% |
| PAD/peripheral intervention (surgical/percutaneous) | 5.0% | 6.4% |
| ICD/CRT | 4.2% | 5.3% |
| Other indications | 0.6% | 1.0% |
ACS: acute coronary syndrome; CABG: coronary artery bypass grafting; CRT: cardiac resynchronization therapy; CV: cardiovascular; ICD; implantable cardioverter-defibrillator; PAD: peripheral artery disease; PCI: percutaneous coronary intervention.
IHD was also the most common referral indication for phase III CR programs, representing (when different definitions were pooled, as above) 55.4% of referrals (Table 6). HF was also the second most common reason for referral for phase II, accounting for 19.8% of patients participating in phase III CR programs.
To our knowledge, data on the total number of patients suffering and surviving an ACS in 2019 were still not available at the time of data collection and analysis. Based on the last published data by the Directorate-General for Health (DGS), reporting a total of 11510 admissions (episodes) for MI in 2016,24 the CR coverage was estimated to be 9.3%.
DiscussionThe present study reports on a pragmatic and contemporary survey on the state of CR in Portugal. Overall, 25 centers provided structured CR programs in 2019. Of these, 12 provided phase I, 22 phase II and 13 phase III interventions. A total of 2182 patients were included in phase II CR programs (1076 in the setting of ACS), while 606 were included in phase III programs.
This study provides important data on the current state of CR in Portugal. Compared to the 2014 data, there was an increase of 33% in the number of centers providing phase I and of 5% in the number of centers providing phase II programs.8 For phase II programs, there was an increase of 13% in the total number of patients included, which translates to an estimated 9.3% coverage of ACS survivors.24 These results are in agreement with the previously reported progressive increase in CR uptake, a finding which is supported by the rise in the number of centers providing these structured interventions and the improvements in terms of the geographical area covered (Table 1).8,21–23 In addition, the Portuguese Registry on ACS (ProACS) showed an increase in the referral rate for phase II programs (scheduled or planned at discharge), which may also be related to this increase (although published data only cover the period up to 2016).25 Nevertheless, overall coverage was still not at an ideal level. Moreover, both the variation in the number of centers (compared to the estimated number expected to provide a broad coverage for the Portuguese population)6 and the reduction in phase III participation should be stressed. Indeed, for structured phase III programs, there was a 37% decrease in the number of patients represented compared to the previous survey.8 These findings should be acknowledged and explored, in order to help develop strategies to promote increases in CR uptake in this setting. Of note, some centers, while not offering structured phase III programs (those including formal ET sessions), nonetheless focused on counseling, especially relating to CV risk factors, thus reinforcing the importance of long-term follow-up and optimization in this patient population.3
Worldwide, the availability and characteristics of CR programs present significant differences.19,26–28 Data from a seminal study by Bjarnason-Wehrens et al., based on the European Cardiac Rehabilitation Inventory Survey, illustrate these variations in different European countries.28 In this study, the proportion of eligible patients included in phase II interventions ranged from <3% to 90%, but was ≤30% in 54% of countries.28 Recent data from the EUROASPIRE V registry further stressed this notion, reporting on 46% of patients advised to undergo CR.29 In the US, studies report participation rates of 20-30%, also with differences among regions and subgroups.30,31 The present survey confirms the sustained increase in the number of centers and patients treated (from 638 in 2007 to 1927 in 2013, and to 2182 in 2019) for phase II programs (Figure 1), which translates into an increased (estimated – see below) coverage after ACS.8,23 Although this improvement should be acknowledged, the 9.3% estimated coverage is still below the optimal value for this intervention.5,6,8,25,28 Several factors have been reported as influencing suboptimal patient representation.6,8,19,20,28,32,33 These include lack of specific facilities and limited capacity to accommodate the number of patients, distance to CR centers, lack of knowledge concerning the intervention (on the part of both healthcare professionals – thus affecting referral rates – and patients), financial constraints, and differences in legislation.6,8,19,20,28,32,33 As expected, several of these were reported by the centers responding to this survey as being associated with lower adherence, as well as affecting patient entry in CR programs (see Results). The present survey thus reinforces the need to address these diverse issues, related to different factors, as tackling some of these challenges could assist in optimizing the uptake of this pivotal intervention. Notably, although drop-out rates ranged from 0 to 68%, most centers (91%) had rates under 25%, which is a proposed quality indicator in a recent statement by the European Association of Preventive Cardiology (EAPC).5 In this context, as the number of CR centers continues to rise (although it is still insufficient given the overall needs, as clearly indicated in previous reports),6,19,34 other parameters should also be recognized as potential obstacles to optimal patient enrollment and adherence.
As in the previous survey, HF presented the second most frequent indication for both phase II (with an increase of 1.8%) and phase III CR programs.8 This is in line with current epidemiological data demonstrating the healthcare burden associated with HF.17,35 Interestingly, referrals after implantation of cardiac resynchronization therapy devices and/or implantable cardioverter-defibrillators also increased (by 3.1%). While the improvement in the number of patients undergoing CR in the setting of HF, albeit small, is encouraging, given the estimated prevalence of this entity efforts should be undertaken to improve referrals.17,35,36 Importantly, different studies have highlighted the cost-effectiveness of this intervention in different patient populations.10,37–39 Given the figures for phase III programs, with fewer patients (Table 5), this is also relevant in this setting.28,40 Of note, the European Cardiac Rehabilitation Inventory Survey has also reported on the broad range of enrollment for these programs, and some of the factors that can hamper their optimization.28
All centers reported having multidisciplinary teams, although frameworks varied (Tables 2 and 4). In this regard, all programs included nutritional counseling, while most offered CV risk factor management, and a large proportion included smoking cessation counseling and psychosocial assessments. Furthermore, access to consultations with different healthcare professionals was also reported for most programs. Although improvements should be made in order to increase the number of programs including these components, the present results reinforce the current notion of CR as a comprehensive and cohesive intervention.5,6 Importantly, recent guidance from both the SPC and EAPC on the components comprising structured CR programs provide a benchmark for the design and tailoring of this intervention.5,6 In this regard, the present results highlight some of the areas where improvement is most needed, as well as presenting some of the potential barriers to their application. Also, the possibility of a national CR registry (as proposed in the current guidelines from the SPC) could further build on the legacy of the present survey, to improve benchmarking concerning various domains of CR.6
As discussed above, the central role of CR programs in CVD has been extensively discussed, and is presently consensual.3–5,9,11,41,42 Although questions concerning the optimal design of such programs, in terms of both efficacy and cost-effectiveness, have still not been fully addressed,4,5,37,43–46 their overall beneficial effects are well established, as supported by the current guidelines.3/4/16-18 The present results are in line with these concepts, with most patients undergoing CR due to IHD and HF, two of the classical indications for these programs.3,17 Although, as previously discussed, efforts should be made to increase the number of patients undergoing CR in the setting of these two entities, as well as improving and streamlining the operative framework (design and scope) of these interventions, future prospects should also be the focus of further research. In this context, the potential role of home-based CR programs should be assessed, particularly given some of the challenges associated with patient adherence and enrollment.5,6,45,47,48 Furthermore, careful consideration should be given to the optimal framework of these programs in the setting of other indications, such as patients with cancer (encompassing the frontier field of cardio-oncology rehabilitation) or left ventricular assist devices.49,50
LimitationsSeveral limitations of the present study should be acknowledged. Firstly, this was a voluntary survey conducted with a pragmatic design. Several variables which could have been of interest, such as patient age and gender, time between discharge and program initiation (for phase II programs), medication adherence and control of CV risk factors (including specific values for the different CV risk factors, in accordance with the current guidelines), and differences in functional capacity, were not available for the present analysis.3–6,41,42 Secondly, an important limitation is the fact that specific data on the total number of ACS in 2019 were, to the best of our knowledge, not available at the time of data assessment. An estimate was accordingly provided based on the latest available data.24 Moreover, the questionnaire sent to centers in the present survey specified as an indication “acute myocardial infarction/ACS (with or without percutaneous coronary intervention)” (in order to provide a description that reflected the guidelines).3,51,52 Hence, when 2019 data were compared to those of the previous survey (reporting on MI) and to the DGS data (also on MI), it is possible that some cases of unstable angina were categorized in this section. Finally, some of the data (as specified in the above tables) were not available for all centers. Although these caveats should be borne in mind when assessing the present results, they should not hinder the overall interpretation of the data, which provide a comprehensive report on the state of CR in Portugal in 2019.
ConclusionThe present survey shows an overall increase in the number of CR centers and of patients participating in phase II CR programs, with an estimated coverage of 9.3% after an ACS. Although these results are significant, they still highlight an important unmet need in terms of CR enrollment and overall patient participation. Furthermore, the reduction in the number of patients enrolled in phase III CR programs should also prompt reflection, in order to improve patient referral and uptake.
As personalized medicine evolves against the background of increasingly sophisticated diagnostic and therapeutic interventions, bringing about major advances while also leading to new challenges, the pivotal and time-tested role of CR as a holistic framework able to provide major improvements in overall health status across different stages of the cardiovascular continuum should be seen as an integral component of the optimal contemporary standard of care.
Conflicts of interestThe author has no conflicts of interest to declare.
The authors would like to express their special thanks to the coordinators of the CR programs for their crucial cooperation in providing the data for the current survey, without which this study would not have been possible, and for their commitment to improving CR in Portugal.