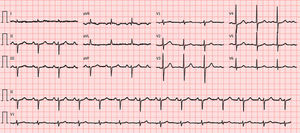
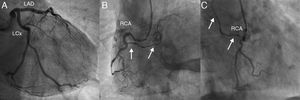
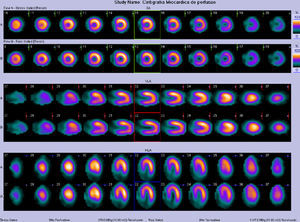
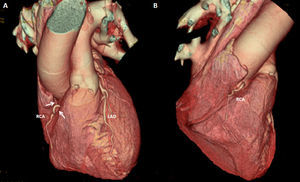
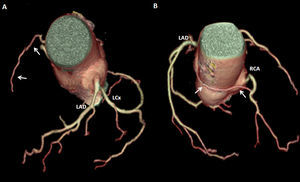
A 74-year-old man, with a history of heavy smoking, presented with unstable angina (Figure 1). Dobutamine stress echocardiography showed ischemia in the right coronary artery territory. Coronary angiography revealed no obstructive epicardial disease in the left dominant circulation (Figure 2A); the right coronary artery (RCA) was a small caliber and tortuous vessel, with only minor atheroma. However, an abnormal vessel arising from the proximal RCA was noted (Figure 2B and C), confirmed as a fistulous connection to the left atrium by multislice computed tomography, which also excluded other vascular anomalies (Figure 3). This was deemed to be causing a coronary steal phenomenon. Exercise myocardial perfusion imaging under anti-ischemic therapy excluded residual ischemia and the patient was successfully conservatively managed (Figure 4).
(A): coronary angiography depicting no obstructive epicardial disease in the left dominant coronary circulation. (B and C): the right coronary artery was a small caliber vessel, with significant tortuosity in its proximal segment, but with no obstructive disease. An abnormal vessel was noted (arrows) arising from its proximal course and heading left, toward a posterior-superiorly located structure. LAD: left anterior descending artery; LCx: left circumflex artery; RCA: right coronary artery.
Multislice computed tomography. (A): 2D multiplanar reformatted image revealing a fistulous connection (arrows) between the proximal right coronary artery (RCA) and the left atrium (LA). (B): 3D volume-rendered image showing the fistula (arrows) arising from the proximal right coronary artery with a retro-aortic course. RA: right atrium; RVOT: right ventricular outflow tract.
Coronary-pulmonary artery fistulas (CPAF) are rare, often incidental findings of coronary angiography, thought to be remnants of a vascular connection from the mediastinal mesoderm. Coronary steal has been reported even in small fistulas, due to runoff to a low-pressure system, with reduction of intracoronary diastolic perfusion pressure. Treatment should be based on the presence of symptoms and anatomy (number and size, nature of feeding vessel, draining site, quantification of myocardium at risk of ischemia and shunt), with catheter and surgical options being offered if technically feasible.
Given the fistula's small size, from a non-dominant coronary artery, and in the absence of right ventricular impairment or significant ischemic burden, a conservative approach was followed. We highlight the role of multimodality imaging to depict CPAF anatomy and their relationship with relevant cardiac structures, and the role of stress testing in guiding therapy.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Supplementary material associated with this article can be found in the online version available at doi:10.1016/j.repc.2012.06.013