Dyspnea and hypoxemia are among the most common symptoms and signs that need to be assessed in clinical practice.
This case illustrates how simple steps in history taking and physical examination can be crucial for diagnosis.
We present a patient with intermittent hypoxemia, initially attributed to a pulmonary infection. However, the hypoxemia persisted even after successful treatment of the infection. Computed tomography angiography of the chest and ventilation/perfusion lung scan excluded pulmonary embolism.
We then observed that the hypoxemia and dyspnea were triggered by orthostatism. An echocardiogram with a bubble test showed a patent foramen ovale, with a right-to-left shunt, without pulmonary hypertension. After percutaneous closure of the foramen ovale, the symptoms completely resolved.
This is a case of platypnea-orthodeoxia syndrome, which is usually associated with patent foramen ovale or atrial septal defect and is typically observed in the elderly. The features and causes of this curious syndrome are discussed.
A dispneia e hipoxemia são dos sintomas e sinais mais comuns que avaliamos diariamente na prática clínica.
Este caso ilustra como uma avaliação simples da anamnese e exame físico podem ser cruciais para o diagnóstico.
Apresentamos um doente com hipoxemia intermitente, inicialmente atribuída a uma infeção respiratória. Contudo, a hipoxemia manteve-se apesar de tratamento eficaz da infeção. A angiotomografia computorizada do tórax e cintigrafia de ventilação-perfusão excluíram tromboembolismo pulmonar.
Verificámos posteriormente que a hipoxemia e dispneia eram despoletadas pelo ortostatismo. Um ecocardiograma com administração de soro agitado revelou a presença de foramen ovale patente, com fluxo espontâneo direito-esquerdo, sem hipertensão pulmonar. Após encerramento do forâmen ovale patente, os sintomas desapareceram.
Este é um caso de síndrome de platipneia-ortodeoxia, que geralmente se associa a foramen ovale patente ou comunicação interauricular, e é especialmente frequente em idosos. Discutimos as características e causas desta interessante síndrome.
We describe the case of an 83-year old man, independent, with a history of hypertension and multiple lacunar strokes in the past.
The patient was admitted after a syncopal episode; standing in the bathroom, he felt nauseated and lightheaded before losing consciousness.
On admission to the emergency department, he felt dyspneic. He denied chest pain, cough, fever, palpitations, orthopnea or other symptoms.
He had some ronchi in the right lung, fever, type 1 respiratory failure and slightly increased C-reactive protein levels. The chest X-ray revealed a discrete opacity in the right inferior lobe. He began treatment for a respiratory infection, resulting in sustained apyrexia and normalization of laboratory parameters. However, the hypoxia persisted, appearing to follow an intermittent pattern. We began to notice that his blood gases and need for oxygen changed almost every day, with no evident pattern, even when the infection was completely cured.
He had no history of coronary disease or arrhythmia, previous dyspnea, orthopnea, chest pain, edema or other signs of heart failure, and a recent echocardiogram showed no anomalies. He had no background of smoking or pulmonary disease.
A thoracic computed tomography angiogram was ordered, which was normal. Because the possibility of a chronic peripheral pulmonary embolism remained, a ventilation/perfusion scan was performed, which also showed no changes.
There was no apparent deterioration on exertion and when low oxygen saturation was recorded the patient's breathing pattern was normal. His pulse oximetry and blood gases were finally measured in different postural positions and it was found that the hypoxia occurred when he was sitting or standing, and did not resolve completely with oxygen (Table 1). Furthermore, he also complained of dyspnea on orthostatism.
The patient was then diagnosed with platypnea-orthodeoxia syndrome (POS) and we set out to clarify its etiology.
This syndrome is caused by a right-to-left shunt that can be due to an intracardiac shunt through a patent foramen ovale (PFO), atrial septal defect (ASD) or fenestrated atrial septal aneurysm (ASA), a pulmonary arteriovenous shunt, or pulmonary ventilation/perfusion mismatch.
Thromboembolic disease or arteriovenous malformations had been excluded, as had parenchymal lung disease. There were no abnormal liver function tests or lesions on abdominal ultrasound, so hepatopulmonary syndrome seemed unlikely. A transthoracic echocardiogram and bubble test, with administration of agitated saline through a peripheral vein, was therefore requested. The passage of microbubbles into the left atrium within the first three beats after right chamber opacification is considered diagnostic of PFO; the appearance of microbubbles following the third beat usually corresponds to intrapulmonary shunting.
The echocardiogram showed normal morphology of the cardiac chambers, an aneurysm of the interatrial septum with to-and-fro flow, preserved biventricular systolic function and dilatation of the ascending aorta, without pulmonary hypertension. When the agitated saline was administered, there was an immediate flow into the left atrium.
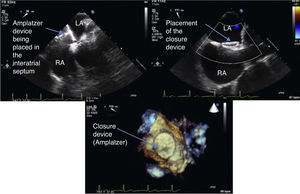
The transesophageal echocardiogram confirmed a right-to-left shunt and a PFO (Figure 1) with no other changes except for the ectatic aorta. Since the patient was clearly symptomatic and with functional limitations, we proposed percutaneous closure of the atrial septal defect, with which he agreed.
Before the PFO was closed, right-sided catheterization confirmed that the right chamber pressures were not increased. A percutaneous closure device (25-mm Amplatzer) was then implanted, guided by transesophageal echocardiography (Figure 2).
After the intervention, the patient no longer had hypoxia on recumbency or orthostatism. The echocardiogram showed that the closure device was correctly placed, with no residual shunt (Figure 3).
The patient returned to his normal life and required no additional nursing care; his mood and quality of life also improved significantly. He is currently doing well, three years after the intervention.
DiscussionPOS is relatively rare; the majority of cases are caused by an intracardiac shunt, which occurs when a structural component, such as an interatrial communication (PFO, ASD or ASD), coexists with a functional component that favors a right-to-left shunt through the defect, particularly in the upright position.
PFO is usually the underlying defect, probably because it is also the most common congenital heart defect in the general population, present in 25% of individuals. Although PFOs are usually asymptomatic, they can be associated with stroke, paradoxical embolism, transient global amnesia, migraine headache, high-altitude pulmonary edema, decompression sickness and, of course, POS.1
What is most interesting is that, in most cases, this shunt occurs without increased pressures in the right cardiac chambers, as in this patient.2,3 The explanation for this puzzling fact appears to reside in conditions that cause a transient increase of pressure in the right atrium or in anatomic changes that affect the position and anatomy of the heart, favoring the direction of flow from the inferior vena cava directly through the septal defect into the left atrium.4,5 The changes associated with this phenomenon include aortic dilatation compressing the right atrium (one of the most common associated structural changes5–8), diaphragmatic paralysis or post-pneumonectomy syndrome, kyphoscoliosis, prominent Eustachian valve or Chiari network, lipomatous interatrial septum, pericardial disease or other conditions that can change the position of the heart, favoring the passage of blood from the right to the left atrium.
Once there is clinical suspicion, diagnosis is usually confirmed by an echocardiogram, preferably transesophageal, complemented by the intravenous injection of agitated saline solution. If the exam can be performed on a tilt table, this can more accurately reveal the right-to-left shunt that occurs with orthostatism. Transthoracic echocardiography and transcranial Doppler, also with bubble tests, are alternatives. This example also highlights the importance and simplicity of performing a bubble test, which greatly increases the sensitivity of detecting a right-to-left shunt.
Treatment of these patients consists of closure of the atrial defect with a device, usually by a percutaneous approach or, if more complex repairs are required, surgically.9–11
One of the first questions that arise concerning this case is “why now?” The patient had probably had the PFO since birth and had so far been asymptomatic. This is also the case with most patients with POS. However, even though the structural defect was already present, some functional change had probably occurred, causing flow from right to left atrium, with hypoxemia and dyspnea in the orthostatic position.
Most cases of POS present in the elderly; aging may affect the size of PFO and is also linked to aortic root dilation, kyphoscoliosis, distortion of the interatrial septum and stiffness of the right ventricle.12–14
In this case, the patient had an intracardiac shunt, without increased right chamber pressures. He also had an enlarged aorta, one of the conditions most often associated with POS, which could cause the heart to rotate, stretching the interatrial septum and directing flow from the vena cava directly into the PFO.7,8 However, the relatively acute onset is not completely explained, although it could be speculated that the pneumonia, trauma after syncope, and perhaps a more violent or sustained Valsalva maneuver could have aggravated the problem. On the other hand, once POS is established, there are no reports of spontaneous resolution of the signs and symptoms.
Considering the patient's previous strokes, it is possible that the PFO may have also contributed to cardioemboli and cerebral ischemia. The prevalence of PFO among ischemic cryptogenic stroke patients is 40–50%, twice its prevalence in the general population.15 Furthermore, individuals with PFO have a 2–3-fold increased risk of migraine and cerebrovascular events.
Percutaneous ASD closure has already become a routine procedure. In this patient, although he had other conditions and old age, we considered it important to close the ASD, because of the severity of his symptoms and impact on his quality of life, limiting his daily activities and leading to total dependence as well as need for supplementary oxygen.
ConclusionsPOS is rare, but is also probably underdiagnosed and can significantly decrease patients’ quality of life.
Most cases of POS caused by an intracardiac shunt occur in the elderly and dilation of the ascending aorta seems to be one of the most common coexisting conditions.
However, the exact mechanisms underlying this intriguing condition are not yet completely understood.
Simple signs and symptoms, like orthostatic hypoxemia and dyspnea, point towards the diagnosis. A simple clinical exam and documentation of the patient's position when pulse oximetry is recorded can lead to this diagnosis.
We therefore recommend testing oxygenation in the orthostatic and supine positions in every patient presenting with unexplained hypoxemia.
Finally, there is a curative treatment for this condition, so diagnosis can have a significant effect on the patient's daily life.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.