In patients with non-ST-elevation myocardial infarction (NSTEMI), the best timing for coronary angiography is not definitely established, although it is recognized that in high-risk patients it should be performed within the first 24 hours. The aim of this work was to describe the evolution over time of the use of an invasive strategy in the treatment of NSTEMI and in-hospital mortality.
MethodsWe performed a retrospective analysis of patients admitted with NSTEMI included in the Portuguese Registry on Acute Coronary Syndromes (ProACS) between 2002 and 2015. The annual proportion of patients undergoing coronary angiography and the time from admission to coronary angiography were assessed, as were changes in mortality and length of stay.
ResultsA total of 18639 patients with NSTEMI were included in the ProACS registry between 2002 and 2015. Over this period there were significant increases in the proportion of patients undergoing coronary angiography (from 52.0 to 83.6%) and angioplasty (from 23.3 to 53.0%), as well as in the proportion of patients who underwent coronary angiography within 24 hours of admission (from 21.0 to 48.1%). In-hospital mortality decreased in those aged over 74 years (from 9.5 to 3.7%) and in males.
ConclusionsThe progressive adoption of an invasive strategy, particularly an early one (within 24 hours), was accompanied by a reduction in in-hospital mortality. Since coronary angiography is performed late (>24 hours) in half of NSTEMI patients, these patients could benefit from initiatives similar to Stent for Life.
Nos doentes internados com enfarte agudo do miocárdio sem supradesnivelamento de ST (EAM-NST), o momento mais apropriado para a realização de coronariografia não está completamente definido, embora esteja estabelecido que, nos doentes de alto risco, se deverá realizar nas primeiras 24 horas. O objetivo deste trabalho é descrever a evolução temporal da utilização de uma estratégia invasiva. Adicionalmente, pretende-se discutir se haverá benefício em estabelecer sistema organizacional similar àquele que já existe para o enfarte com supra de ST.
MétodosAnálise retrospetiva dos doentes admitidos com EAM-NST, incluídos no Registo Nacional de Síndromas Coronárias Agudas, entre 2002-2015. Avaliou-se a percentagem de doentes submetidos a coronariografia e o tempo desde a admissão até à coronariografia, de acordo com o ano da admissão, género e idade, assim como a evolução da mortalidade e do tempo de internamento.
ResultadosA análise incluiu 18639 doentes. Entre 2002-2015, observou-se um significativo aumento percentual das coronariografias (52,0 versus 83,6%) e angioplastias (23,3 versus 53,0%), assim como nas coronariografias realizadas nas primeiras 24 horas (21,0 versus 48,1%). A mortalidade intra-hospitalar diminuiu ao longo do período de análise, particularmente nos doentes com mais de 74 anos (9,5 para 3,7%) e no género masculino.
ConclusõesA adoção progressiva da estratégia invasiva, em particular da estratégia invasiva precoce, foi acompanhada temporalmente por uma diminuição da mortalidade. Como metade dos doentes de alto risco continua a realizar a coronariografia tardiamente, considera-se que o EAM-NST poderia beneficiar com um sistema organizacional como a iniciativa Stent for Life.
Myocardial infarction (MI) is a clinical condition that has a considerable impact on public health. It is defined using clinical, laboratory and electrocardiographic criteria,1 the latter of which distinguish ST-elevation myocardial infarction (STEMI) from non-ST-elevation myocardial infarction (NSTEMI). For STEMI, the international guidelines state that the benefit of treatment is greater the shorter the time between symptom onset and reperfusion therapy.2 It has also been established that when performed promptly and by experienced teams, the best therapeutic option is primary percutaneous coronary intervention (PCI).3 On the basis of these findings, national and international programs have been established aimed at reducing delays between symptom onset and reperfusion.4 One international initiative promoting early revascularization with primary PCI is Stent for Life.5 Portugal joined this initiative in 2011,6 which coincided with a substantial rise in the number of primary PCIs performed annually, from 106 per million population in 2002 to 338 per million in 2013.7
NSTEMI is associated with high short- and medium-term risk of cardiovascular morbidity and mortality.8 Although most patients will benefit from an invasive approach with coronary angiography,9 the decision on which approach to adopt is more complex than in STEMI. One factor that influences prognosis is the timing of catheterization.10
The main aim of this work was to describe the evolution over time of the incidence, use of an invasive strategy, and in-hospital mortality in NSTEMI in Portugal, based on data from the Registry on Acute Coronary Syndromes (ProACS) of the Portuguese Society of Cardiology.
At the same time, it is hoped that the results will shed light on the desirability, especially in high-risk groups, of adopting a similar organizational strategy to that developed for STEMI through the Stent for Life initiative.5,6
MethodsWe performed a retrospective observational analysis of patients admitted with NSTEMI included in ProACS between 2002 and 2015.
ProACS is a voluntary registry managed using CardioBase software (InforTUCANO SI) both for management of hospitalized patients’ medical records and for storing data from admission to discharge for the registry. ProACS covers the entire Portuguese territory and includes 44 active centers. Even so, not all centers record all patients, and a minority of centers are responsible for most of the patients included (nine centers included over 80% of its patients in 2011, 2012 and 2013). There have also been considerable annual variations in the numbers of patients included, with a maximum of 7453 in 2002, compared to 2453 in 2013.
Patients included have suffered MI according to the criteria of the third universal definition.1 Demographic and clinical data were recorded, including classical risk factors, length of hospital stay, and details of catheterization and revascularization (percutaneous or surgical).
For the purposes of this study, the main focus was on evolution over time of the annual proportion of patients with NSTEMI undergoing coronary angiography and of in-hospital mortality in this population.
Since this was an observational study, it also assessed the evolution over time of the relative proportions of NSTEMI and STEMI patients.
Statistical analysisThe sample and results were assessed using descriptive statistical methods according to the variables and their distribution. Continuous variables were expressed as median (interquartile range) or mean (standard deviation) and categorical variables as relative and absolute frequencies. Statistical inferences associated with comparisons of the same variable over time were analyzed with the Kruskal-Wallis test for continuous variables and the chi-square test for categorical variables. The analysis was carried out using IBM SPSS version 19 and a p-value of <0.05 was considered significant.
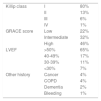
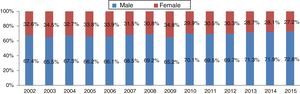
ResultsClinical and demographic characteristics of patients with non-ST-elevation myocardial infarction in the Portuguese Registry on Acute Coronary SyndromesBetween 2002 and 2015, a total of 42934 patients were included in the ProACS, 18639 of them with NSTEMI. Demographic data and clinical history of the patients included are presented in Table 1, while Table 2 shows their clinical presentation and comorbidities. Of note, a high proportion (80%) were in Killip class I, and risk stratification revealed a high GRACE score in 46%. Figure 1 reveals a significant increase in the number of included patients with a diagnosis of NSTEMI (p<0.001) as opposed to STEMI. During the study period mean and median hospital length of stay tended to decrease (Figure 2). Most patients were male (Figure 3), and the prevalence of cardiovascular risk factors (hypertension, dyslipidemia, diabetes and smoking, in decreasing proportions) presented the same pattern over time (Figure 4).
Demographic characteristics and clinical history of the study population.
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean age, years ± SD | 67±12 | 67±12 | 67±12 | 68±12 | 68±13 | 68±13 | 68±13 | 68±13 | 67±13 | 67±13 | 68±13 | 67±13 | 67±13 | 67±12 | NS |
| Female | 32.6% | 34.5% | 32.7% | 33.8% | 33.9% | 31.5% | 30.8% | 34.8% | 29.9% | 30.5% | 30.3% | 28.7% | 28.1% | 27.2% | <0.001 |
| History of diabetes | 29.3% | 28.7% | 31.5% | 33.5% | 32.6% | 29.4% | 29.9% | 35.2% | 32.6% | 31.1% | 36.0% | 35.2% | 35.3% | 34.3% | <0.001 |
| History of PCI | 5.8% | 6.8% | 7.2% | 7.9% | 7.5% | 9.0% | 11.3% | 12.2% | 14.6% | 16.2% | 16.3% | 17.7% | 16.0% | 17.7% | <0.001 |
| History of CABG | 4.6% | 4.2% | 5.3% | 5.1% | 6.8% | 6.2% | 6.3% | 4.7% | 7.1% | 5.2% | 6.8% | 8.1% | 7.9% | 6.9% | <0.001 |
| History of PAD | 4.7% | 3.6% | 3.5% | 3.8% | 4.5% | 3.2% | 4.7% | 3.1% | 5.7% | 6.5% | 6.8% | 7.7% | 7.6% | 7.4% | <0.001 |
| History of CKD | NA | NA | NA | NA | NA | NA | NA | NA | 8,6% | 8,6% | 8,4% | 7,9% | 6,9% | 6,2% | NS |
CABG: coronary artery bypass grafting; CKD: chronic kidney disease; NA: data not available; NS: non-significant; p: by chi-square test; PAD: peripheral arterial disease; PCI: percutaneous coronary intervention.
Clinical presentation and comorbidities of the study population.
| Killip class | I | 80% |
| II | 13% | |
| III | 6% | |
| IV | 1% | |
| GRACE score | Low | 22% |
| Intermediate | 32% | |
| High | 46% | |
| LVEF | >50% | 65% |
| 40-49% | 17% | |
| 30-39% | 11% | |
| <30% | 7% | |
| Other history | Cancer | 4% |
| COPD | 4% | |
| Dementia | 2% | |
| Bleeding | 1% |
COPD: chronic obstructive pulmonary disease; LVEF: left ventricular ejection fraction.
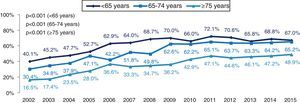
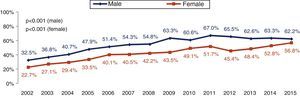
Analysis of the diagnostic and therapeutic approach to NSTEMI shows that the proportion of patients undergoing coronary angiography increased significantly, from 52% in 2002 to 84% in 2015 (p<0.001), and the proportion undergoing primary PCI rose from 23% in 2002 to 52% in 2015 (p<0.001) (Figure 5). This resulted in a significant increase from 29% to 61% in the total number of patients revascularized, overall (p<0.001) and for all age-groups (p<0.001 for each, Figure 6) and for both genders (p<0.001, Figure 7).
Over the 13-year period in which patients in the ProACS were studied, the proportion who underwent early coronary angiography (<24 hours) rose from 21% to 48% (Figure 8).
The proportion of NSTEMI patients undergoing coronary angiography more than 72 hours after admission (late invasive strategy) was 49% in 2002 but fell significantly to 12% in 2015 (p<0.001).
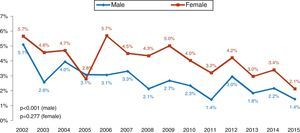
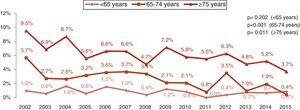
In-hospital mortalityThere was an overall trend for lower in-hospital mortality over the period of inclusion in the registry (p<0.01) (Figure 9), although this was significant only in males (p<0.001 vs. p=0.277 in females). This fall was most marked in the group aged over 74 years (from 9.5% to 3.7%, p<0.001), and was also significant in the 65-74 year age-group (p=0.011). In-hospital mortality remained low in younger patients throughout the study period (Figure 10).
DiscussionThe main findings of this study were that over time, the proportion of NSTEMI patients undergoing catheterization (particularly within 24 hours) followed by revascularization when indicated has risen, while in-hospital mortality has fallen. Although a causal relationship cannot be established between increased use of an early invasive strategy and a decrease in in-hospital mortality, our ecological approach, documenting change in opposite directions, suggests that one may exist.
Over the last 13 years there has been a significant evolution in the treatment of NSTEMI in the Portuguese population, with more patients undergoing increasingly early coronary angiography and PCI. The impact of the timing of revascularization has been the subject of considerable debate. The FRISC II11 and RITA 312 trials, and data from the pre-revascularization phase of ISAR-COOL,13 as well as meta-analyses by O’Donoghue et al.9 and Fox et al.,14 all indicate the benefits of an invasive compared to a conservative strategy in patients with non-ST-elevation acute coronary syndrome (NSTE-ACS).
The European8 and American15 guidelines recommend risk stratification for patients with NSTE-ACS and state that those with NSTEMI (with significant rises in troponin, the main criterion for high risk) should be referred for an early invasive strategy, in agreement with the data from the TIMACS16 and ACUITY17 trials and the meta-analysis by Katritsis et al.18 These recommendations, together with the resulting fall in in-hospital mortality, have led to improvements in the standards of treatment for patients in the ProACS registry, especially due to the more widespread and increasingly early use of coronary angiography.
The results documented here are comparable to those of Khera et al.19 in a contemporary (2002-2011) registry on the US population, in which a significant increase in the use of an early invasive strategy was observed across all age-groups, accompanied by decreases in length of stay and in-hospital mortality. One finding in our study that deserves attention is the higher in-hospital mortality in females, which may be due to more advanced age, non-specific symptoms, and delays in beginning appropriate treatment.20 This observation has previously been reported in Portuguese21 and international20 registries, but it should be noted that in both cases, the higher mortality associated with female gender disappeared when adjusted for age.
In the Stent for Life initiative, there is much in common between the strategies used to optimize treatment for STEMI and NSTEMI. One stage of the initiative, organizing campaigns to raise public awareness of the symptoms of MI,6 benefits both groups. However, the next step – provision of care – is very different: in cases of STEMI, if detected on the electrocardiogram at first medical contact, the patient must be transported immediately to a center with primary PCI facilities.5 When ST elevation is not detected, there is disagreement as to which approach to adopt. A minority of very high-risk patients, with sustained pain or electrical or hemodynamic instability, should benefit from the same treatment. A British registry from 2008,22 in which individuals with NSTEMI referred for primary PCI had a comparable frequency of acute coronary occlusion to those with STEMI, suggests that the coronary fast-track system should be activated in this context.
The fact that half of the patients with NSTEMI in our study were not treated by an invasive strategy within 24 hours raises important organizational questions. How can care be improved for high-risk patients,8 i.e. those with repolarization abnormalities, ST-T segment changes and a GRACE score over 140? A study currently under way23 aims to develop a pre-hospital algorithm for the triage of patients with chest pain that will select those with a high probability of NSTEMI for urgent transportation to a PCI-capable center within 24 hours. In the emergency department, patients with NSTEMI are subject to significant delays in diagnosis and in administration of antiplatelet therapy.24
In our opinion, these patients would benefit from the adoption of an organizational model with the following components: primary transportation to a hospital that can perform revascularization within 24 hours; familiarity with the criteria of severity for NSTEMI in the emergency department; and increased awareness on the part of interventional cardiology teams of the benefits of an early invasive strategy.
Although we suggest consideration of changes in the organizational model for NSTEMI, it is important to emphasize that standardization of care should not be allowed to stand in the way of individual clinical assessment. Thus, NSTEMI patients who have not been considered for an invasive strategy, or those with type 2 MI (imbalance between oxygen supply and myocardial demand), may not be included in the target population for such organizational changes.
Since its implementation in 2002, the purpose of the ProACS registry has been to document real-world practice in detail and to monitor adherence to the guidelines.25–27 However, certain limitations must be acknowledged. As a voluntary registry, it may not be immune to a degree of selection bias. Furthermore, although increased revascularization rates have coincided with reductions in in-hospital mortality and length of stay, a causal relation cannot be definitely established, since other factors, such as improvements in pharmacological therapy, technological advances in interventional cardiology, and changes in hospital policies, may also have played a part in these results.
ConclusionsBetween 2002 and 2013 there was a significant increase in the proportion of NSTEMI patients treated by an invasive strategy, and a significant reduction in in-hospital mortality and length of hospital stay.
However, the proportion of patients undergoing early coronary angiography is still less than 50%.
We therefore consider that NSTEMI patients could benefit from the implementation of an organizational model like the Stent for Life initiative, in order to improve health care and reduce the time between admission and revascularization.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank Dr. Adriana Belo, biostatistician at the Portuguese National Center for Data Collection in Cardiology (CNCDC), for her help in processing the data of the ProACS registry.
Please cite this article as: Morgado G, Pereira H, Caldeira D, em nome dos investigadores do Registo Nacional de Síndromas Coronárias Agudas. Adoção da estratégia invasiva precoce no enfarte agudo do miocárdio sem supra de ST: análise dos resultados do Registo Nacional de Síndromas Coronárias Agudas. Rev Port Cardiol. 2018;37:53–61.