Aortic pulse wave velocity (PWV) has been associated with cardiovascular risk in different clinical subsets. This subanalysis of the EDIVA project aimed to establish criteria for normality of PWV based on a statistical definition that considers the fundamental physiological role of aging in arterial stiffness.
MethodsA sample of 668 healthy subjects (412 male) enrolled in the EDIVA Project (a prospective, multicenter, observational study) were studied. Mean age was 40.00±13.42 years, body mass index was 25.90±4.21kg/m2, and systolic and diastolic blood pressure were respectively 125.47±11.18 and 75.75±9.27 mmHg. PWV was determined annually using a Complior device, and mean follow-up was 23.3±3.34 months. Personal and family history, physical examination, electrocardiogram and biochemical analysis were used to determine individual health.
ResultsIn the overall population PWV was 8.8±1.4m/sec, 8.7±1.6m/sec in men and 8.9±1.5m/sec in women (p=NS). Normal PWV was defined as the 95th percentile adjusted for age and gender, above which PWV was considered abnormal. Serial evaluation of PWV also enabled the annual age-dependent increase in PWV to be estimated at 5%, values above this cut-off being defined as abnormal vascular deterioration.
ConclusionThis study establishes criteria for normality based on a statistical definition that takes into account the fundamental physiological role of aging in arterial stiffness. Additionally, it provides a cut-off for the clinical interpretation of serial PWV measurements.
A velocidade da onda de pulso carotideo-femoral (VOP) tem constituído um importante marcador de risco cardiovascular, traduzindo o reflexo arterial subsequente a um conjunto de contextos clínicos em que o impacto cardiovascular é manifesto. Este trabalho visou estabelecer parâmetros de normalidade da VOP para a população portuguesa, com base numa definição estatística.
MétodoO presente trabalho corresponde a uma sub-análise do Projecto EDIVA, envolvendo 668 indivíduos saudáveis (412 do sexo masculino), com idade média 39,73±15,6 anos, índice de massa corporal 25,56±4,05kgm2, pressão arterial sistólica e diastólica respectivamente 125,47±11,18 e 75,75±9,27mmHg. Estes indivíduos foram submetidos a um follow-up médio de 23,3±3,34 meses, com avaliação anual da VOP. A normalidade foi definida em termos da história pessoal e familiar, da avaliação clínica, do ECG de superfície e da realização de exames analíticos de rotina.
ResultadosA VOP média na amostra foi de 8,8±1,4m/s, sendo de 8,7±1,6m/s e 8,9±1,5m/s, respectivamente no sexo feminino e masculino (p=ns). A normalidade foi definida a partir do percentil 95 para cada faixa etária, e por género. A avaliação sequencial permitiu ainda avaliar o contributo percentual de agravamento da VOP face ao envelhecimento (5%), definindo-se assim uma variação positiva da VOP (em avaliações sequenciais) inferior a 5% como normal.
ConclusãoOs resultados obtidos permitem: por um lado, estabelecer critérios de referência para a VOP tendo em consideração o papel determinante do envelhecimento na deterioração fisiológica da função das grandes artérias; por outro lado, estabelecer uma medida de valorização da variação longitudinal da VOP, aspecto que se reveste de grande importância face à adopção desta metodologia em programas integrados de seguimento de doentes com risco cardiovascular manifesto.
Cardiovascular disease has an extremely high incidence and prevalence worldwide, and accounts for a high percentage of overall mortality, particularly in western societies1.
Cardiovascular mortality is determined mainly by clinical conditions that involve the arterial system, and hence research into this system has become of prime importance. It is highly likely that a better understanding of the pathophysiology of arterial disease will have a significant positive impact in terms of public health.
Various methods have been developed to assess the arterial system using different approaches, but their usefulness in clinical practice is heavily dependent on operator- and technology-related variables.
Measurement of pulse wave velocity (PWV) is a rigorous method of assessing arterial stiffness2, with a solid experimental basis and with important contributions from physics3,4. From a clinical standpoint, several studies have shown that aortic PWV is an independent cardiovascular risk marker in various clinical contexts5–15. The 2007 joint guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC) recognize this parameter as a marker of subclinical target organ damage16.
Despite the clinical importance of this measure of aortic stiffness, reference values for PWV have yet to be defined. The ESH/ESC guidelines suggest a cut-off of 12 m/s for aortic PWV to define vascular damage16, but this lacks an experimental foundation since only one prospective study in a highly selected population (patients with renal failure) suggests this value to define cardiovascular risk. At the same time, the nature of PWV is not conducive to an operational approach to defining normality, given that cardiovascular risk is continuous and that this parameter is highly age-dependent, as all studies have shown in this context, and so a given PWV value will have a different clinical significance depending on the age-group studied. We have therefore always considered that a statistical approach would be more suiTable for defining normal PWV values, with reference values adjusted for age and gender, an opinion recently adopted by an important research group in this area17.
The aim of the EDIVA project was to develop an approach to assessing global cardiovascular risk by quantifying individual risk using this methodology in a large population. It resulted in a prospective, multicenter, observational study involving 2200 individuals (of whom 668 were healthy), mean follow-up currently two years, with the aim of defining reference criteria for the Portuguese population (the scope of the present study), as well as improving understanding of the value of PWV measurement in predicting major adverse cardiovascular events (MACE)18.
MethodsDescription of the projectThe EDIVA project was established to raise awareness of PWV measurement, incorporating a training element and a monitoring structure and leading to the collection of data for statistical analysis.
TrainingBetween 2002 and 2004 a series of meetings were held in different locations, in which most of the participants were general practitioners (GPs). The meetings were aimed at providing a theoretical overview of the physiological and scientific bases of PWV measurement and at encouraging participants to use this parameter in their clinical practice.
Establishment of reference centersThe centers that agreed to participate in the EDIVA project were supplied with the equipment required for PWV measurement, and technical training in its use was also provided19,20. In this way, the exam was available to general clinicians working in the catchment area of each center, for both inpatients and outpatients. For outpatients, GPs were requested to fill out a short form listing pathologies, history and the results of routine exams for the patients in question. No exams were performed merely for the purposes of the study, the data used being those from the last measurement performed. The result of the PWV measurement was recorded in a brief quantitative and qualitative report for ease of clinical use. Therapeutic decisions regarding the patients observed were in all cases left to the attending physician. Three centers fulfilled the criteria for inclusion in the EDIVA project: two public (Hospital Pedro Hispano and Hospital Santo André) and one private primary care clinic (Clínica da Aveleira).
Study populationThe present study is a sub-analysis of the EDIVA project, which is an epidemiological study assessing cardiovascular risk through serial PWV measurement. From the 2200 Portuguese nationals (1290 men and 910 women), aged between 18 and 91 years (mean: 46.33±13.76), who made up the study cohort, a subgroup of 668 individuals with low cardiovascular risk was selected. Low-risk individuals were defined as those who had had no chronic disease or been prescribed long-term pharmacological therapy, and had normal physical exam, electrocardiogram, and blood and urine tests, these characteristics having remained unchanged for at least two annual assessments.
The study's aims were explained to all participants and their informed consent obtained. The methodology used to collect the data was approved by the Portuguese Data Protection Commission and the study was approved by the Ethics Committees of the hospitals involved. Mean follow-up was two years.
Study designThis was a prospective, multicenter, observational study monitoring the occurrence of MACE - death, stroke, transient ischemic attack, myocardial infarction, unsTable angina, peripheral arterial disease, revascularization or renal failure. Follow-up consisted of annual assessments including carotid-femoral PWV, blood pressure (BP), laboratory tests and clinical observation. At each consultation, the participants' weight and height were measured and body mass index (BMI) was calculated in kg/m2. BP was measured in a supine position after a 10-minute rest period, by an experienced operator using a clinically validated (class A) sphygmomanometer (Colson MAM BP 3AA1-2®; Colson, Paris)21.
Three measurements were taken, the arithmetic mean being used in the analysis. All participants underwent routine fasting laboratory tests. At the first consultation they filled out a questionnaire concerning relevant personal and family history, smoking habits, alcohol consumption, and medication.
Pulse wave velocityAortic stiffness was assessed annually in all individuals by determining carotid-femoral PWV using a Complior® device (Colson, Paris) in accordance with a previously described technique19. Briefly, PWV was based on the distance/time ratio (meters/second) with the pulse wave measured simultaneously in the right carotid and right femoral arteries, the distance used being that between the sites where the pressure waves were recorded (point-to-point). Measurements were performed by the same operator and the quality of the recordings was evaluated by two independent observers with considerable experience of the method. Normal PWV was defined statistically according to the 95th percentile adjusted for gender and age, calculated on the basis of a sample of 668 individuals with low cardiovascular risk, mean age of 39.73±15.6 years, BMI of 25.56±4.05 kg/m2, and systolic (SBP) and diastolic (DBP) blood pressure of 125.47±11.18 and 75.75±9.27 mmHg, respectively. The reproducibility of these estimates previously determined in our laboratory showed correlation coefficients better than 0.9 (0.98 and 0.95, respectively, for inter- and intra-observer differences)20.
Statistical analysisData from the sample subjects were processed using SPSS for Windows, version 15.0. The distribution of the variables was tested for normality using the Kolmogorov-Smirnov test, and for homogeneity of variance by Levene's test. Simple descriptive statistics were used to characterize the sample and the distribution of variables.
A Table of normal PWV values was constructed based on the 95th percentile adjusted for gender and age.
Groups were compared using the chi-square test for categorical variables and the Student's t test (two groups) for quantitative variables. Simple and multiple linear regression analyses were repeatedly performed to assess the determinants of PWV. A value of p ≤0.05 was taken as the criterion of statistical significance for a 95% confidence interval.
ResultsGeneral characteristicsThe general characteristics of the study population are summarized in Table 1. Mean age was 40.00±13.42 years, with a higher proportion of men (60% vs. 40%, p=0.001). All individuals had normal laboratory and clinical parameters, with women presenting older mean age (43.26±13.19 vs. 37.72±13.12, p=0.001), and higher cholesterol (170.14±20.70 vs. 163.56±22.61, p=0.001), heart rate (69.45±10.75 vs. 67.44±13.45, p=0.04) and BMI (26.66±4.93 vs. 25.40±3.58, p=0.001). By contrast, men presented higher values for waist circumference (89.60±9.15 vs. 84.67±10.65, p=0.001) and pulse pressure (52.52±11.03 vs. 50.52±13.09, p=0.036). PWV was slightly higher in men than women (respectively 9.28±1.71 m/s vs. 9.04±1.74 m/s, p=0.079). Smoking was reported by 22% of participants, with a higher prevalence among men (31% vs. 8% in women, p=0.001), and 8% reported a family history of cardiovascular events.
Characteristics of the study population
| Total | Men | Women | p | |
| n, % | 668 | 60% | 40% | 0.001 |
| Age, years | 40.00±13.42 | 37.72.±13.12 | 43.26±13.19 | 0.001 |
| Body mass index, kg/m2 | 25.90±4.21 | 25.40±3.58 | 26.66±4.93 | 0.001 |
| Waist circumference, cm | 86.83±10.30 | 89.60±9.15 | 84.67±10.65 | 0.001 |
| Family history, no:yes* | 92:8 | 92:8 | 93:7 | 0.912 |
| Smoking, no:yes* | 78:22 | 69:31 | 92:8 | 0.001 |
| SBP, mmHg | 129.17±14.33 | 129.89±9.56 | 128.02±8.70 | 0.125 |
| DBP, mmHg | 77.43±10.11 | 77.39±9.54 | 77.42±10.88 | 0.969 |
| PP, mmHg | 51.74±11.90 | 52.52±11.03 | 50.52±13.09 | 0.036 |
| Mean BP, mmHg | 94.68±1.26 | 94.89±9.29 | 94.34±11.63 | 0.520 |
| HR, bpm | 68.21±12.58 | 67.44±13.45 | 69.45±10.75 | 0.040 |
| PWV, m/s | 9.18±1.72 | 9.28±1.71 | 9.04±1.74 | 0.079 |
| Total cholesterol, mg/dl | 167.47±21.52 | 163.56±22.61 | 170.14±20.70 | 0.001 |
| Blood glucose, mg/dl | 82.86±9.16 | 82.92±10.75 | 84.99±9.64 | 0.149 |
| Triglycerides, mg/dl | 96.43±19.01 | 88.50±20.32 | 115.79±18.21 | 0.106 |
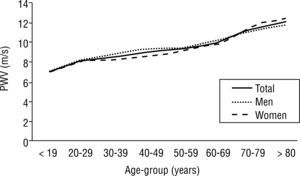
A cross-sectional analysis of the correlation between PWV and various clinical parameters showed a significant correlation with age (r=0.425, p <0.001), BMI (r=0,189, p <0.001), waist circumference (r=0.229, p <0.001), SBP (r=0.276, p <0.001), DBP (r=0.266, p <0.001), mean BP (r=0.293, p <0.001), pulse pressure (r=0.103, p=0.008), heart rate (r=0.230, p <0.001) and blood glucose (r=0.103, p=0.008). Figure 1 shows the behavior of PWV according to age and gender, with a linear increase in arterial stiffness with aging, and men presenting higher PWV up to the 6th decade of life, after which PWV is higher in women.
PWV values were similar in smokers and non-smokers (respectively 9.06±0.22 m/s vs. 9.16±0.12 m/s, p=0.656) and in individuals with and without a family history of cardiovascular events (respectively 9.08±0.20 m/s vs. 9.19±0.06 m/s, p=0.574), after adjustment for SBP, DBP and age.
Reference values for normality for PWV are proposed in Table 2, constructed on the basis of the 95th percentile by age-group (10-year intervals) and gender (taking account of differences in PWV behavior between the sexes).
Reference criteria for normality for pulse wave velocity
| Age-group | Mean (SD) | Range of variation | 95th percentile | |
| Men | 10-19 | 7.0 (1.01) | 4.8-8.8 | 8.8 |
| 20-29 | 8.3 (1.18) | 4.6-11.1 | 10.5 | |
| 30-39 | 8.9 (1.02) | 6.7-11.1 | 10.9 | |
| 40-49 | 9.4 (1.07) | 7.4-11.2 | 11.1 | |
| 50-59 | 9.5 (1.01) | 7.8-11.3 | 11.1 | |
| 60-69 | 10.3 (1.87) | 7.5-12.3 | 12.3 | |
| 70-79 | 11.2 (1.06) | 9.4-13.1 | 13.1 | |
| > 80 | 11.8 (1.39) | 10.3-13.5 | 13.5 | |
| Women | 10-19 | 7.1 (1.26) | 5.3-8.8 | 8.8 |
| 20-29 | 8.2 (1.01) | 5.4-11.2 | 10.0 | |
| 30-39 | 8.2 (1.12) | 5.4-11.2 | 10.1 | |
| 40-49 | 8.6 (1.11) | 6.2-11.0 | 10.5 | |
| 50-59 | 9.2 (1.20) | 6.5-11.0 | 10.9 | |
| 60-69 | 9.8 (1.22) | 8.2-12.0 | 12.0 | |
| 70-79 | 11.7 (0.70) | 11.1-13.1 | 13.1 | |
| >80 | 12.4 (1.10) | 10.2-14.2 | 14.0 |
SD: standard deviation.
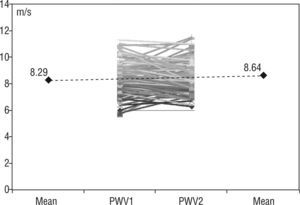
In the context of adapting this methodology to serial assessment of PWV in clinical practice, it was also important to establish a criterion for the percentage of annual increase in PWV that has clinical significance, which could help in integrated cardiovascular risk assessment. To this end, and given that these individuals have had their aortic PWV measured over a mean follow-up of 23.30±3.34 months, it was possible to estimate the percentage increase in PWV with aging (Figure 2). The 95th percentile of the mean annual rise was used as a clinical indicator of age-dependent variation, an increase of less than 5% per year being defined as normal. The slope of the regression line for annual PWV variation in serial assessments was: y=0.3528x + 7.938, with r2=0.02.
DiscussionArterial stiffness is an important area in cardiovascular research, particularly because of its value for risk stratification in various clinical situations. Carotid-femoral pulse wave velocity is without doubt the best indicator of aortic stiffness2, and is unequivocally related to cardiovascular mortality and morbidity in patients with diabetes, hypertension or renal failure, in the elderly, and in the general population5–15. Over the last two decades, our group has focused on this subject, investigating the importance of PWV in conditions such as hypertension22–25 and atherosclerotic disease25, as well as its pathophysiological26–28 and therapeutic29,30 aspects. We have now embarked upon a more ambitious project, which sets out to study prospectively the importance of PWV as a cardiovascular risk marker in what is an unusually large population in this area of research. The inclusion of a large group of low cardiovascular risk individuals posed the greatest challenge but is at the same time the project's most innovative aspect. Although well aware that there is no universally accepted definition of normality, we were able to select a group that is highly representative of the healthy Portuguese population, and to use their characteristics as an objective reference for PWV assessment. We therefore opted for a statistical definition of normality, based on the 95th percentile of PWV, adjusted for age and gender, which is an intuitive and simple measure for use in clinical practice. We were thus able to establish different PWV cut-offs indexed to age and gender, which constitute the reference values for the methodology used to assess arterial stiffness in the study population.
Willum-Hansen et al.14 and Shokawa et al.13 proposed different but useful methods for the clinical interpretation of PWV in the general population, assessing cardiovascular risk in terms of increasing levels of arterial stiffness or defining risk according to PWV thresholds, the latter being well documented in other studies in different clinical contexts.
The present study was designed to explore an alternative method of interpreting PWV values in clinical practice. This was based on recognition of the importance of age as the main factor affecting arterial stiffness. The same PWV value will reflect different pathophysiological contexts in a young or elderly individual, and should therefore be interpreted differently from a clinical standpoint.
Assessment of cardiovascular risk based on the reference values proposed has been shown to have high discriminatory power18, with an adjusted hazard ratio (HR) of 5.252 for the primary endpoint (MACE), and approximate adjusted HRs for cerebrovascular (HR=5.142, confidence interval [CI]: 1.92-17.80) and coronary (HR=3.681, CI: 1.22-11.16) risk. Subgroup analysis provided data that reinforce the validity of the methodology used: the HR for each 1 m/s increment in PWV was 1.748 (CI: 1.470-2.078) for those aged under 50, higher than in the 50–60 age-group (HR=1.514, CI: 1.187-1.933) and in those aged over 60 (HR=1.182, CI: 0.902-1.849). At the same time, the discriminatory power of PWV tended to be stronger in individuals without hypertension or diabetes. While this finding should be interpreted with caution in view of the small number of events recorded to date, they should not be disregarded given the possible clinical implications. If this trend means that PWV measurement is particularly useful in primary prevention, by indicating very early vascular involvement prior to any clinical manifestation of diseases such as hypertension, diabetes or atherosclerosis, then assessment of this parameter based on levels of normality will be of considerable importance.
Comparison of our data with those from joint research in various European centers17 shows a tendency for higher PWV values in the Portuguese population for all the age-groups under analysis. This may be related to specific ethnic characteristics, although certain factors well-documented in the Portuguese population that are known modulators of arterial stiffness, such as high salt intake, cannot be discounted31. Nevertheless, methodological differences may affect linear comparison of PWV values. Our study was based on PWV measurement using a strict and consistent methodology, all assessments being performed by the same operator. In the study referred to above17, PWV measurement was performed using a variety of methods and by a large number of operators, and it is questionable whether the conversion algorithms used would have succeeded in harmonizing the results from the different centers involved. At the same time, the rigor of our definition of normal values is considerably greater than that proposed by this research group.
Another aim achieved in the present study, which has important practical implications, is the establishment of a measure for clinical evaluation of increasing PWV in serial assessments. Studies have demonstrated that patients showing progressive deterioration in PWV present a higher risk for cardiovascular events, but up to now there has been no indication of the percentage of annual PWV increase that exceeds what would be expected physiologically due to aging and that should thus be considered abnormal. The proposed Figure of 5% may prove to be an additional tool for the dynamic evaluation of patients' general state of arterial distensibility, although the implications for cardiovascular risk stratification require confirmation.
However, the project has other aims, in particular to contribute to raising awareness of the concept of arterial distensibility, as well as to demonstrate its suitability for day-to-day clinical practice. In order to achieve these aims, considerable effort has gone into training and into convincing physicians that, if they can obtain PWV assessment for their patients, it should be included in their overall therapeutic approach.
In conclusion, analysis of aortic PWV based on the 95th percentile for age and gender appears to be a simple, intuitive way to broaden use of the concept of arterial stiffness and adapt it to day-to-day clinical practice. At the same time, the establishment of a measure to assess PWV variation over time is crucial to the adoption of this parameter in integrated follow-up programs for patients at cardiovascular risk. This sub-analysis of the EDIVA project, based on the overall results of that epidemiological study, suggests a method of estimating arterial distensibility in clinical practice that represents a significant contribution to improving assessment of cardiovascular risk.
Conflicts of interestThe authors have no conflicts of interest to declare.
The EDIVA Project was supported and sponsored by Clínica da Aveleira and Medinfar Farmacéutica, SA. We are grateful to this company for the integrity and commitment they have shown in an exemplary collaboration between the pharmaceutical industry and postgraduate medical training.