Ischemic stroke is the leading cause of mortality in Portugal, with around 30 to 50% of cases being of cardioembolic etiology. Transesophageal echocardiography (TEE) has assumed growing importance in the detection of cardiac sources of embolism. However, there is controversy regarding the implications of TEE findings for the therapeutic approach to patients with ischemic stroke.
ObjectivesTo analyze TEE findings in the diagnostic work-up of patients with ischemic cerebral events and to determine their infl uence on therapeutic strategy.
MethodsWe retrospectively studied patients with stroke or transient ischemic attack (TIA) before the age of 65, of no apparent cause after carotid ultrasound, electrocardiogram and transthoracic echocardiography, who underwent TEE between 1992 and 2009. The following diagnoses on TEE were considered as potential embolic sources: atrial septal defect; patent foramen ovale (PFO); atrial septal aneurysm (ASA); vegetations; tumors; intracavitary thrombi; and aortic plaques >2mm (ascending aorta and arch).
ResultsWe analyzed 294 patients, mean age 45 years, 56.8% men. TEE revealed a potential cardioembolic source in 36.7% of the patients, PFO and ASA being the most frequent. Throughout the period considered, there was an increase in the number of exams performed, as well as in diagnoses, mainly PFO and ASA. Comparison of patients with and without a diagnosis on TEE showed that the former were older and were more often prescribed oral anticoagulation. By multivariate analysis, the presence of a positive TEE finding was shown to be an independent predictor of treatment with oral anticoagulation (OR=2.48; CI 95%: 1.42-4.34; p=0.001).
ConclusionIn the population under analysis, TEE was useful in identifying potential cardioembolic sources and influenced the therapeutic strategy.
O acidente vascular cerebral (AVC) isquémico é a principal causa de morte em Portugal, estimando-se que cerca de 30 a 50% dos casos sejam de etiologia embólica cardíaca. O ecocardiograma transesofágico (ETE) tem assumido um papel cada vez mais importante na identificação de potenciais fontes cardíacas de embolização. No entanto, o seu papel na orientação terapêutica tem sido mais controverso.
ObjectivosAnalisar os dados obtidos pelo ETE na avaliação diagnóstica dos doentes internados com AVC, assim como a influência dos mesmos na orientação terapêutica.
MétodosEstudo retrospectivo de doentes com AVC ou acidente isquémico transitório (AIT) até aos 65 anos, sem diagnóstico após ecodoppler dos vasos do pescoço, electrocardiograma (ECG) e ecocardiograma transtorácico (ETT), submetidos à realização de ETE entre 1992 e 2009. Relativamente aos achados do ETE, foram considerados como potenciais fontes embólicas os seguintes diagnósticos: defeito do septo interauricular (SIA) ou comunicação interauricular; foramen ovale patente (FOP); aneurisma do SIA (ASIA); vegetação; trombo intracavitário; tumor; placas aórticas > 2 mm (aorta ascendente e arco).
ResultadosForam avaliados 294 doentes com idade média de 45 anos, sendo 56,8% do sexo masculino. O ETE diagnosticou potenciais fontes embólicas cardíacas em 36,7% dos casos, sendo o FOP e o ASIA os diagnósticos mais frequentes. Ao longo do período avaliado, verificou-se um aumento do número de exames realizados assim como do número de diagnósticos, principalmente de FOP e ASIA. Quando comparados os doentes com achado diagnóstico no ETE com os restantes, verificou-se que os primeiros eram mais idosos e mais frequentemente medicados com hipocoagulação oral. Através de análise multivariada, a presença de um achado diagnóstico no ETE foi confirmada como preditor independente da instituição de hipocoagulação oral (OR=2,48; IC 95%: 1,42-4,34; p=0,001).
ConclusãoNa população avaliada, o ETE revelou-se útil na pesquisa de potenciais fontes embólicas cardíacas e infl uenciou a subsequente orientação terapêutica.
Stroke is a major cause of morbidity and mortality worldwide1, and is the leading cause of mortality in Portugal, affecting two to three people every hour according to the Portuguese Stroke Society2.
Around 80 % of strokes are ischemic, of which 30-50 % are of cardioembolic etiology3–5.
Transesophageal echocardiography (TEE) has been shown to be superior to transthoracic echocardiography (TTE) in detecting cardioembolic sources, as it provides better visualization of posterior cardiac structures (left atrium and left atrial appendage) and the thoracic aorta, which are important sources of systemic embolism 6,7. Despite the recognition of TEE's diagnostic superiority, some authors still questioned its usefulness in the therapeutic management of patients with stroke or transient ischemic attack (TIA)8. However, more recent studies have shown that TEE findings influence therapeutic strategy4,9. Long-term treatment options following an ischemic cerebral event are anticoagulation or single or dual antiplatelet therapy. Given the different risk/benefit profiles of the available therapies, the selected treatment should provide the greatest possible protection with the lowest associated bleeding risk. However, there is still controversy as to the most appropriate treatment in certain situations, such as complex aortic atheromas and patent foramen ovale (PFO), for which there are as yet no evidence-based therapeutic strategies4. The significance of some diagnostic findings from TEE in terms of therapeutic management is thus unclear.
The results of two Portuguese studies, by Cabral et al. and Timoteo et al.10,11, on the role of TEE in the diagnostic assessment of patients with ischemic events are in agreement with those of other leading authors. However, neither study analyzed the influence of TEE findings on subsequent therapeutic management of the patients.
ObjectivesOur aim was to analyze patients with stroke and/or TIA before the age of 65 of no apparent cause after carotid ultrasound (or other exams assessing the carotid arteries), ECG and TTE, who underwent TEE for detection of a cardioembolic source. TEE findings (undetected or inconclusive by TTE) were characterized and their influence on subsequent therapeutic management was determined by comparing patients with and without potential embolic sources on TEE.
MethodsWe retrospectively analyzed 294 patients who underwent TEE in an 18-year period (1992 to 2009) in the echocardiographic laboratory at Braga Hospital for investigation of a cardioembolic source as the cause of stroke and/or TIA. Inclusion criteria were a confirmed diagnosis of stroke and/or TIA (by imaging study and/or clinical assessment) and age under 65. Exclusion criteria were atrial fibrillation (identified on ECG or Holter monitoring), >50 % carotid stenosis by carotid ultrasound, angiography or magnetic resonance angiography (all patients underwent at least one of these diagnostic exams), or a clear diagnostic finding on TTE. Certain findings on TTE (including suspected PFO or atrial septal aneurysm [ASA]) were not conclusive, thus prompting assessment by TEE.
Demographic, clinical, laboratory and echocardiographic data were obtained from computerized and/or paper-based medical records.
All TEE exams were performed in the echocardiographic laboratory of Braga Hospital's cardiology department. Various ultrasound systems were used during the period under analysis (1992-2009), in chronological order: Hewlett Packard Sonos 2000, Acuson Sequoia C256, and Philips iE33 (the latest, in use since 2007, equipped with a S7-2 Omni transducer).
All exams were performed after six hours’ fasting with the patient in left lateral decubitus. To reduce the discomfort of the exam, a 5 mg dose of diazepam was usually administered sublingually and lidocaine gel was applied to facilitate introduction of the probe into the oropharynx. Intracardiac shunts were investigated using intravenous injection of agitated saline solution during the Valsalva maneuver.
The following findings on TEE (together with definitions when appropriate) were considered potential embolic sources:
- •
Atrial septal defect (ASD) — any solution of continuity in the interatrial septum (IAS);
- •
Patent foramen ovale — interatrial shunt (flow) at the level of the fossa ovalis in the apparent absence of a solution of continuity at this level or the presence of a tunnel-like solution of continuity characteristic of PFO, documented by Doppler and/or agitated saline solution test (injected via an arm vein, ideally at the elbow, with passage of at least one bubble to the left atrium following the Valsalva maneuver within three cardiac cycles after opacification of the right atrium)12;
- •
Atrial septal aneurysm — excursion of the mid portion of the IAS by at least 10 mm beyond the septal plane (towards one or other of the atria depending on variations in atrial pressures during the cardiac cycle)13;
- •
Vegetations;
- •
Intracavitary thrombus;
- •
Tumor;
- •
Aortic plaques of >2 mm (ascending aorta and arch). This figure was used since it was not possible to accurately quantify plaques of >2 mm; however, while plaques of >4 mm are strongly associated with ischemic cerebral events, smaller plaques have also been linked to increased risk for stroke or TIA14.
The chi-square test was used to compare categorical variables (expressed in percentages). Continuous variables (expressed as means ± standard deviation) were compared using the Student's t test when they presented a normal distribution, and the Mann-Whitney test otherwise. Multivariate logistic regression analysis was used to identify the variables independently associated with treatment with oral anticoagulation. A value of p <0.05 was considered statistically significant.
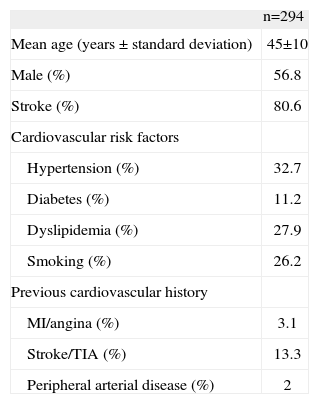
ResultsThe baseline characteristics of the patients undergoing TEE are shown in Tabla 1.
Baseline characteristics of patients undergoing transesophageal echocardiography
| n=294 | |
| Mean age (years ± standard deviation) | 45±10 |
| Male (%) | 56.8 |
| Stroke (%) | 80.6 |
| Cardiovascular risk factors | |
| Hypertension (%) | 32.7 |
| Diabetes (%) | 11.2 |
| Dyslipidemia (%) | 27.9 |
| Smoking (%) | 26.2 |
| Previous cardiovascular history | |
| MI/angina (%) | 3.1 |
| Stroke/TIA (%) | 13.3 |
| Peripheral arterial disease (%) | 2 |
MI: myocardial infarction; TIA: transient ischemic attack.
Mean age was 45±10 years, and 56.8 % were male. The ischemic event was stroke in 80.6 % of the patients. With regard to cardiovascular risk factors (diabetes, hypertension, dyslipidemia and smoking), 61.2 % had at least one risk factor, hypertension being the most common (in 32.7 %).
TEE findings are listed in Tabla 2, which shows that a potential cardioembolic source was detected in 36.7 % of the patients, the most common being PFO (20.1 %) and ASA (16.7 %), while 10.5 % had both.
Embolic sources detected on transesophageal echocardiography
| Diagnosis | % of total population (n=294) |
| Atrial septal defect | 7.8 |
| Patent foramen ovale | 20.1 |
| Atrial septal aneurysm | 16.7 |
| Vegetations | 0.7 |
| Tumor | 0 |
| Thrombus | 2.4 |
| Aortic plaques | 10.5 |
| Diagnosis of potential embolic source | 36.7 |
| More than one diagnosis | 13.9 |
There was a significant increase in the number of exams performed (85 vs. 209) in the second half of the study period, as well as in the percentage of exams detecting a potential embolic source, mainly cases of PFO and ASA.
Of the patients with PFO (n=59), 52.5 % also presented ASA, and 13.6 % were referred for percutaneous PFO closure; three-quarters of the latter also had ASA and most were referred in the last five years of the study period.
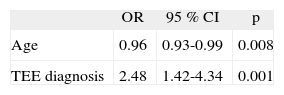
Comparison of patients with and without a positive TEE finding (undetected or inconclusive by TTE) (Tabla 3) showed that the former were older, with no significant differences in other baseline characteristics. Patients with positive TEE were more often treated with oral anticoagulation. Multivariate logistic regression analysis, adjusted for possible confounding variables, showed that the presence of a positive TEE finding was an independent predictor of treatment with oral anticoagulation (Tabla 4). Only one patient was contraindicated for this treatment, due to a history of intracranial hemorrhage.
Baseline characteristics and therapeutic management according to transesophageal echocardiographic findings
| TEE diagnosis | No TEE diagnosis | p | |
| (n=108) | (n=186) | ||
| Stroke (%) | 84.3 % | 78.5 % | 0.28 |
| Male (%) | 56.5 | 57 | 1 |
| Age (years ± standard deviation) | 47±10 | 43±10 | 0.008 |
| Cardiovascular risk factors | |||
| Hypertension (%) | 38.3 | 30.2 | 0.2 |
| Diabetes (%) | 11.2 | 11.5 | 1 |
| Dyslipidemia (%) | 26.2 | 29.7 | 0.6 |
| Smoking (%) | 26.2 | 26.9 | 1 |
| <1 risk factor (%) | 67.3 | 59.3 | 0.2 |
| Previous cardiovascular history | |||
| MI/angina (%) | 2.9 | 3.3 | 1 |
| Stroke/TIA (%) | 17 | 11.4 | 0.2 |
| Therapeutic management | |||
| Oral anticoagulation (%) | 37.4 | 20.4 | 0.002 |
| Antiplatelet therapy (%) | 63.4 | 80.4 | 0.002 |
| Dual antiplatelet therapy (%) | 10.3 | 6 | 0.25 |
MI: myocardial infarction; TEE: transesophageal echocardiography; TIA: transient ischemic attack.
TEE revealed a potential cardioembolic source in 36.7 % of the study population, PFO and ASA being the most common (20.1 and 16.7 %, respectively), the two anomalies often being associated (in 10.5 % of patients). These results are in agreement with those of other studies, including recent ones2,15.
There was a significant increase throughout the study period in the number of exams performed as well as in diagnoses of potential cardioembolic sources (in both relative and absolute terms), mainly cases of PFO and ASA. These results are in agreement with those of Timoteo et al.10, reflecting both more widespread availability of TEE as a method to screen for potential cardiac sources for systemic embolism and greater diagnostic accuracy for detection of certain anomalies, particularly PFO and ASA, due to improvements in scanner and transducer technology and in techniques.
There is controversy concerning the significance of many TEE findings (particularly PFO, ASA and aortic plaques) as a cause of stroke or TIA9,15-17, and the ideal treatment for secondary prevention in these patients, particularly those with PFO or aortic atheromas, has been debated at length. Although recent guidelines favor antiplatelet therapy over oral anticoagulation in patients with cryptogenic stroke and PFO, this is a suggestion rather than a strong recommendation in view of the conflicting evidence 18. Similarly, there have been no randomized trials assessing antithrombotic therapy in patients with aortic plaques, and current guidelines generally favor antiplatelet therapy, with oral anticoagulation being reserved for patients with mobile aortic arch thrombi18.
In our study, the presence of any one of the findings defined as a potential embolic source was shown to be an independent predictor of treatment with oral anticoagulation (OR=2.48; 95 % CI: 1.42-4.34; p=0.001). This is in agreement with other authors who found that TEE findings influenced the therapeutic strategy adopted, particularly in younger patients4,19.
In our population, TEE findings also led to percutaneous PFO closure in eight patients (13.6 % of those with PFO). Although the number of such procedures is increasing, evidence to support an invasive strategy is sparse18. The results of the CLOSURE I trial, the first randomized study to compare percutaneous PFO closure with medical therapy for secondary prevention of stroke and TIA, were recently presented and showed that percutaneous closure was not superior to medical therapy20. Other randomized studies on this subject are currently in progress, namely the CLOSE, PC, RESPECT and REDUCE trials, and will no doubt provide new insights.
It should be borne in mind that since the present study covers a period of 18 years (1992-2009), the therapies described are not necessarily those currently recommended but rather a combination of the different therapies that were considered appropriate at particular times for particular patients. There have been various changes over this period in the light of available evidence and guidelines for the therapeutic management of these patients, which has been the subject of considerable debate for the last 20 years.
However, despite the uncertainty and controversy surrounding the most appropriate treatment for certain anomalies, it was found that TEE findings influenced the therapeutic strategy in the period under analysis, confirming the important role of TEE in stroke and TIA in younger patients.
Study limitationsCertain limitations should be borne in mind when interpreting this study. Since it was a retrospective, non-randomized study conducted in a single center, the results may have been influenced by known and unknown confounding factors. Due to the impossibility of accurately quantifying aortic plaque size from the medical records, the figure used in the analysis (>2 mm) differs from the size generally accepted as representing a significant embolic risk14,21. Nevertheless, our results in this respect do not differ from the findings of other authors10.
ConclusionsIn the present study of patients aged under 65 with stroke or TIA of no apparent cause after ECG, carotid ultrasound and TTE, transesophageal echocardiography identified potential cardioembolic sources in a large number of patients.
It was also found that TEE findings had an independent influence on choice of therapeutic strategy (oral anticoagulation or antiplatelet therapy), supporting the role of TEE in the assessment of younger patients with stroke or TIA of no apparent cause after ECG and carotid ultrasound.
Conflicts of interestThe authors have no conflicts of interest to declare.
- Home
- All contents
- Publish your article
- About the journal
- Metrics
- Open access