Approval of a drug for clinical use requires production of data on efficacy and safety through submission of results from randomized controlled trials (RCTs), in which the new molecule is usually compared with placebo (or an active comparator) for a set of outcomes that will serve as the basis for the drug's indications. These indications are crucial, because drugs are approved on the basis of their net clinical benefit for specific and well-defined diseases and–importantly–only for these. Once the drug is available for use in tens or hundreds of thousands of patients, physicians may realize that some medications can be effective in diseases for which they were not approved, i.e., no studies have been presented to the regulatory authorities, and therefore they are not formally approved for those indications. Convinced of the benefits for their patients, some physicians prescribe them for unapproved indications–off-label prescription.
O processo de aprovação de medicamentos para uso clínico implica a produção de provas de eficácia e segurança através da submissão de resultados de ensaios clínicos, em que a nova molécula é comparada habitualmente ao placebo (ou a um comparador ativo) para um conjunto de resultados nos quais se baseará a determinação das indicações. As indicações são absolutamente cruciais, porque os fármacos são aprovados segundo o perfil de benefício/risco que apresentam para tratamento de patologias específicas, bem definidas e - um aspeto muito importante - apenas para estas. Uma vez estando o medicamento disponível para ser utilizado em dezenas ou centenas de milhares de doentes, acontece por vezes que, no decurso do seu uso regular e rotineiro, chega ao conhecimento dos médicos que certas moléculas podem ser eficazes em situações para as quais não foram aprovadas, isto é, em que não foram apresentados estudos de suporte às autoridades regulamentares e que portanto não estão legalmente aprovadas para essas indicações. Convictos dos benefícios para os seus doentes, alguns médicos vão receitar medicamentos para indicações não aprovadas - a chamada prescrição off-label.
Neste artigo discute-se a prevalência da prescrição off-label, assim como as suas vantagens e inconvenientes.
A drug is only used in clinical practice after a complex process of research and development that lasts on average 12-15 years, of which marketing authorization is the penultimate step. This is granted by the European Medicines Agency for all European countries. For such authorization to be given, evidence must be provided of efficacy and safety through submission of the results of phase 3 randomized controlled trials (RCTs), in which the new molecule is compared with placebo or an active comparator.
In most cases, the last step in the process is the adoption of the drug by national authorities for outpatient and/or hospital use. It is this step that, with rare exceptions, makes the drug available to patients. This decision is taken when the national authority (Infarmed in Portugal) makes a positive appraisal of the new drug's health and/or economic benefits (the latter through economic evaluation studies), compared to the alternative reference therapy used in clinical indications for the disease in question. Only if the new drug constitutes a therapeutic innovation – by filling a therapeutic gap when compared with placebo, no treatment or best supportive care – will it be adopted. A substance is not necessarily a therapeutic innovation simply because it is new.1
Central to this process is the definition of indications for the drug in question. These indications are crucial, because drugs are approved (or not) on the basis of their net clinical benefit for specific and well-defined diseases and – importantly – only for these.
Once the drug is granted marketing authorization, the manufacturer can only market it for the approved indication(s); it is illegal to promote, directly or indirectly, or even to suggest, its use for other diseases or other types of patients (although this does happen2). Pharmaceutical companies can add new indications to those already approved, but they rarely do, because the clinical trials required are lengthy and expensive and there is little incentive to conduct them, since the drug is already on the market. More common are extensions to the approved indications, such as to other age-groups or to different patient subtypes. Generic drug manufacturers are likewise reluctant to conduct the RCTs needed for new approvals, for the same financial reasons.
Once the drug is available for use in tens or hundreds of thousands of patients, physicians may realize that some medications can be effective in diseases for which they were not approved, i.e., no studies have been presented to the regulatory authorities, and therefore they are not formally approved for those indications. Convinced of the benefits for their patients, some physicians prescribe them for unapproved indications – off-label prescription.
Off-label prescription is thus defined as prescription for an indication, disease, or patient outside the approved indications, or for populations that have not been studied (such as pediatric patients), or using methods of administration or dosages that have not been approved.3 The rationale for off-label prescription is that the official agencies do not regulate the practice of medicine, and that physicians are free to decide what they consider best for their patients.
There are two types of off-label prescription:
- •
the use of a drug that is indicated for a particular disease in a completely different condition, such as anti-epileptic agents for neuropathic pain;
- •
the use of a drug within its indications, but outside the approved specifications, such as sildenafil, approved for erectile dysfunction but used by patients without this condition in order to enhance sexual performance.
The spectrum of off-label use includes guideline-recommended practice (aspirin in diabetes for prophylaxis against cardiovascular disease), last-resort therapy (tacrolimus for autoimmune diseases, in addition to transplantation), and first-line therapy (gabapentin for painful diabetic neuropathy).
Certain types of off-label prescription are of particular concern and require careful scrutiny4:
- •
The off-label use of recently introduced drugs is a major problem, since not only will there be virtually no evidence of their benefit, but safety data from pharmacovigilance will also be scarce, obviously complicating their use.
- •
Novel off-label use – one that is different from usual clinical practice – has similar problems of lack of data on efficacy and especially on safety, even if the drug itself has been on the market for more than 3-5 years.
- •
When any drug with known serious or frequent adverse effects is prescribed off-label, this use merits close attention owing to concerns for patient safety.
- •
Finally, off-label prescription of high-cost drugs raises its own questions, since the financial penalty involved demands particular practical reflection.
In this paper we discuss some formal and practical aspects of off-label prescription, including its prevalence, advantages and disadvantages, and examine the nature of the evidence supporting its use.
The prevalence of off-label prescriptionSo long as drugs prescribed off-label are safe, well tolerated and inexpensive, the practice does not usually lead to major problems. However, as stated above, problems arise with high-cost drugs for specific diseases, a well-known example of which is new biological drugs for the treatment of cancer; in some studies, off-label administration of these drugs reaches 75%.5
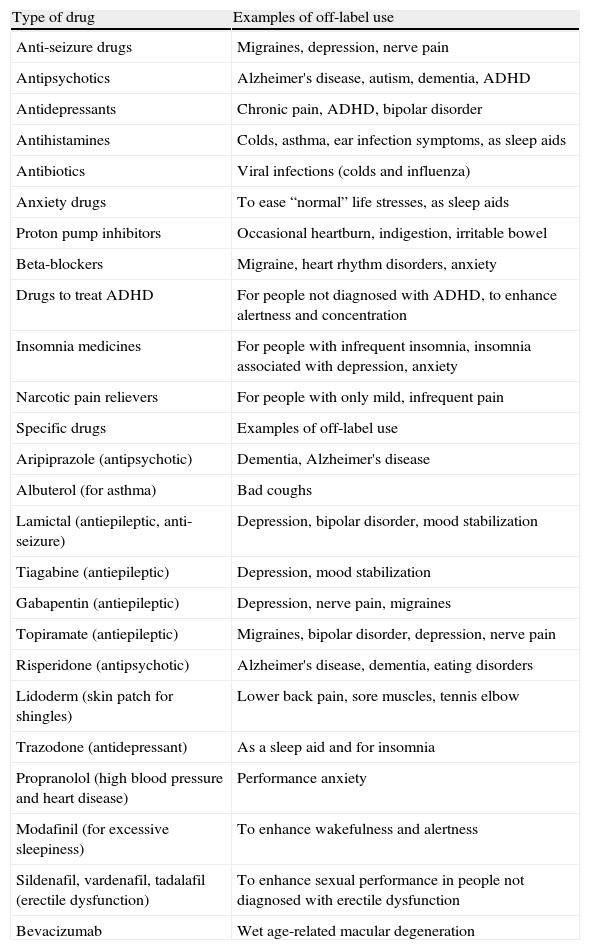
In any event, whether for outpatient or in-hospital use, off-label prescription occurs for almost all drug classes, with a particularly high prevalence for certain drugs (Table 1).
Drugs commonly prescribed off-label (Consumer Reports Best Buy Drugs, www.CRBestBuyDrugs.org, accessed August 2012).20
| Type of drug | Examples of off-label use |
| Anti-seizure drugs | Migraines, depression, nerve pain |
| Antipsychotics | Alzheimer's disease, autism, dementia, ADHD |
| Antidepressants | Chronic pain, ADHD, bipolar disorder |
| Antihistamines | Colds, asthma, ear infection symptoms, as sleep aids |
| Antibiotics | Viral infections (colds and influenza) |
| Anxiety drugs | To ease “normal” life stresses, as sleep aids |
| Proton pump inhibitors | Occasional heartburn, indigestion, irritable bowel |
| Beta-blockers | Migraine, heart rhythm disorders, anxiety |
| Drugs to treat ADHD | For people not diagnosed with ADHD, to enhance alertness and concentration |
| Insomnia medicines | For people with infrequent insomnia, insomnia associated with depression, anxiety |
| Narcotic pain relievers | For people with only mild, infrequent pain |
| Specific drugs | Examples of off-label use |
| Aripiprazole (antipsychotic) | Dementia, Alzheimer's disease |
| Albuterol (for asthma) | Bad coughs |
| Lamictal (antiepileptic, anti-seizure) | Depression, bipolar disorder, mood stabilization |
| Tiagabine (antiepileptic) | Depression, mood stabilization |
| Gabapentin (antiepileptic) | Depression, nerve pain, migraines |
| Topiramate (antiepileptic) | Migraines, bipolar disorder, depression, nerve pain |
| Risperidone (antipsychotic) | Alzheimer's disease, dementia, eating disorders |
| Lidoderm (skin patch for shingles) | Lower back pain, sore muscles, tennis elbow |
| Trazodone (antidepressant) | As a sleep aid and for insomnia |
| Propranolol (high blood pressure and heart disease) | Performance anxiety |
| Modafinil (for excessive sleepiness) | To enhance wakefulness and alertness |
| Sildenafil, vardenafil, tadalafil (erectile dysfunction) | To enhance sexual performance in people not diagnosed with erectile dysfunction |
| Bevacizumab | Wet age-related macular degeneration |
ADHD: attention deficit/hyperactivity disorder.
In cardiology, a typical example of off-label prescription is the use of new anticoagulants – dabigatran, rivaroxaban, apixaban – in situations in which warfarin is the first-line drug. A recent analysis examined other off-label uses of cardiological drugs, including thrombin and factor Xa inhibitors6; other common examples are the use of aspirin for cardiological prevention in diabetic patients and of beta-blockers for essential tremor.
For some drugs, of course, good evidence is available for their use in particular conditions (such as beta-blockers for essential tremor, as mentioned above7) but no formal indication has been approved; it should be borne in mind that only the holder of the marketing authorization has the legal right to alter or add to a drug's indications, and that the authorities cannot do so.
One well-publicized case of the existence of evidence for an unapproved indication is of bevacizumab (Avastin®) for age-related macular degeneration, for which the only drug with formal indication is ranibizumab (Lucentis®). A non-inferiority clinical trial comparing the two, the CATT trial,8 concluded that ranibizumab and bevacizumab had equivalent effects on visual acuity at one year and that differences in rates of serious adverse events require further study.
Another example of off-label prescription is the use of recombinant factor VIIa.9 Initially approved only for the treatment of hemophilia, especially in patients who have developed factor VII inhibitors, recombinant factor VIIa is used as a hemostatic agent in cardiac surgery, trauma and intracranial hemorrhage, to the point that prescription for approved indications accounts for only 3% of cases.10
The prevalence of off-label prescription has not received the attention that it warrants. Various numbers appear in the literature, ranging from 20%11 to 50% (Pharmaceutical Executive 2012) of prescriptions in the US, 60% in some Australian hospitals (Discussion Paper Working Group of NSW TAG, 2003), 30% in outpatients in the UK (NICE 2012) and 23% in Europe.12 The most frequently cited study,13 based on a US survey of outpatient prescriptions, reports an overall rate of 21% of off-label prescription, rising to 46% of cardiac medications (excluding lipid-lowering and antihypertensive medications) and of anticonvulsants. Gabapentin had the highest proportion of off-label prescription (83%), followed by amitriptyline (81%). In most cases (73%) there was no evidence to back up the use of these drugs outside their approved indications.
To summarize, off-label prescription is very common, and the drug classes involved are generally the more complex ones.
The advantages of off-label prescriptionOff-label prescription may occur for a variety of different reasons6:
- 1.
a class effect, by which drugs of the same class are presumed have similar effects in a particular disease (for example, the use of a statin for primary prevention that has only been studied for secondary prevention);
- 2.
extension of therapies approved for severe clinical situations to milder forms, such as the use of spironolactone, approved for patients in NYHA classes III and IV, for patients in classes I and II14,15;
- 3.
extension to related conditions (use of the antiasthmatic montelukast for chronic obstructive pulmonary disease);
- 4.
expansion to distinct conditions sharing a physiological link (use of the antidiabetic drug metformin to treat polycystic ovarian syndrome); and
- 5.
extension to conditions whose symptoms overlap with those of an approved indication, in the belief that the off-label treatment will be equally effective (gabapentin for non-neuropathic pain syndromes).
Besides these justifications for off-label prescription, there are other arguments in its favor6,11: it enables new indications to be discovered, particularly when approved treatments have failed; it can dispense with the lengthy and costly drug approval process via official agencies, offering earlier access to drugs and adoption of new practices based on emerging evidence (and thereby enabling physicians to accumulate evidence prior to official approval); and experimentation with new drugs can be justified for many less common diseases for which there are no effective approved treatments.
Furthermore, there are some circumstances in which there is no alternative to off-label prescription. The most obvious example of this is pediatrics. Since very few clinical trials are performed in children, most drugs used in pediatric populations do not have approved indications. Another example is in certain rare diseases that also lack approved treatments due to the impossibility of carrying out effective clinical trials; here also the only possible treatment may be with drugs approved for other conditions. But off-label prescription for common conditions also occurs in clinical practice; for example, the use of beta-blockers in congestive heart failure began before there were clinical trials to support this indication.
Problems with off-label prescriptionGiven the complex and painstaking process of approval and introduction that new drugs must go through, which is intended to ensure both their efficacy and safety, any use outside the indications for which they were evaluated naturally raises important questions.
Prescription of a drug outside its approved indications will increase the individual physician's civil and criminal responsibility. It has been suggested that physicians should in some cases be obliged to provide patients with information on the risks of off-label prescription and to obtain their consent – a similar process to the informed consent process.11 In times of economic constraints other considerations come into play, since health authorities – whether local (hospitals and family health centers), regional or national – are under increasing pressure to audit and monitor drug prescriptions and to take measures, individually and collectively, to rationalize their use.
Unlike physicians, the drug manufacturers have little legal liability with regard to off-label prescription, since they can only be held responsible for problems that arise when their product is used within its approved indications. Furthermore, off-label prescription may in fact discourage the pharmaceutical industry from conducting clinical trials for new or different indications (thereby reducing public confidence in the drug evaluation process), encourage ever wider use in unstudied populations such as children and the elderly, and, when the drugs in question are expensive, increase health care costs.
One of the main concerns with off-label prescription is the lack of effective pharmacovigilance due to a low level of reporting, which may obscure safety issues. It should be recalled that drugs with a good safety profile for a specific use, prescribed for the studied population and with the approved indications, may not be safe with unapproved use and/or in unstudied patient groups.
An example of this is the CATT trial referred to above, which compared ranibizumab (the approved drug) and bevacizumab (unapproved) for the treatment of age-related macular degeneration, and which revealed differences in serious adverse effects between the two.8,16 Although the differences did not permit firm conclusions to be drawn, the authors stated that further studies were required to assess the safety of the two drugs, particularly bevacizumab. This led to a recent systematic review directly comparing three RCTs, including the CATT trial, with a total of 1333 patients, that assessed the safety of off-label use of bevacizumab vs. ranibizumab for the same indications.17 The results showed that bevacizumab has a significantly higher rate of ocular adverse effects (risk ratio [RR] 2.8; 95% confidence interval [CI] 1.2-6.5) and serious infections and gastrointestinal disorders (RR 1.3; 95% CI 1.0-1.7). In indirect comparisons with a variety of controls (5 RCTs, 4054 patients), and based on the two-year results of three landmark trials, the risk of ocular adverse effects was higher for bevacizumab (RR 3.1; 95% CI 1.1-8.9), even though the absolute baseline risk for these patients was low (2.1%). A significant increase in nonocular hemorrhage was observed with ranibizumab (RR 1.7; 95% CI 1.1-2.7), while no difference was detected in the incidence of arterial thromboembolic events.
As well as providing a better characterization of the safety of off-label bevacizumab, this review included several studies and was thus better able to find differences between the drugs, thereby partly overcoming the limitations of individual trials to identify safety issues. The consequence in this case has been a change in the Summary of Product Characteristics for bevacizumab, which now include the risk of ocular adverse reactions following unapproved intravitreal use of bevacizumab under the heading “Special warnings and precautions for use” (http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000582/WC500029271.pdf, accessed October 31, 2012).
Besides the potential safety issues with off-label bevacizumab, the results of the CATT trial are a classic example of the limited ability of clinical trials to characterize the safety and tolerability of drug therapies, particularly when adverse events are uncommon (though serious) and/or occur late, due to the limited number of patients and duration of the trial. A well-known recent example was the cardiovascular risk of cyclooxygenase inhibitors.18 Most clinical trials now have open extensions, during which patients are treated for a specific period (usually until the new drug is licensed). The main aim of such extensions is to evaluate safety and tolerability.
The evidence for off-label prescriptionAs stated above, the evidence produced by the original investigation is mainly intended for the regulatory approval process of new drugs with a view to their introduction to the market. However, there may be evidence that could serve as the basis for the drug to be used outside its approved indications. In this case, the question is whether the physician can justify off-label prescription if there is good evidence to support the practice.
In our opinion, routine off-label use of drugs may be justified if there is high-quality (real-world) evidence that they are effective and safe, and that their overall risk/benefit ratio is acceptable for a specific context (such as data on long-term use in chronic diseases).3
One proposed classification of evidence that could support off-label prescription divides it into supported evidence (with a moderate to high level of certainty of net health benefits), suppositional evidence (a low level of certainty), and investigational evidence (unknown level).4
One of the more complicated problems with evidence that may support off-label prescription is that it can be presented in a variety of ways, some of which lack rigor. A recent study of compendia of indications for off-label oncology treatments19 found that they cited little of the available evidence, often neither the most recent nor that of highest methodological quality, and were analyzed on a completely random basis. For the 14 off-label indications studied, the compendia differed in the indications included and whether and how they recommended particular agents for particular types of cancer.
To summarize, off-label use of a drug may be justified if there is high-quality evidence to support such use, bearing in mind that the results may differ markedly from those obtained when the drug is used within its approved indications.
ConclusionsOff-label prescription is an inescapable aspect of modern health care systems.
In this paper we set out to examine the need to obtain evidence to support the use of drugs outside their approved indications and thereby to promote rational and evidence-based prescription. Such use should always be an exception, to reduce inappropriate use and to ensure patients’ safety.
When prescribing, the physician should pay particular attention to the adverse effects of off-label use and whenever possible should obtain supporting evidence.
Although we recognize that in certain areas, such as pediatrics and oncology, off-label prescription is inevitable, we argue that it should always be an exception and should be supported by high-quality evidence that the physician must be able to explain.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Vaz Carneiro A, Costa J. A prescrição fora das indicações aprovadas (off-label): prática e problemas. Rev Port Cardiol. 2013;32:681–686.