Carotid artery angioplasty with stenting is an effective treatment for carotid artery stenosis, but is frequently associated with acute transient hemodynamic changes. We present the case of a 73-year-old female patient with long-standing refractory hypertension who remained normotensive during a three-year follow-up after undergoing staged bilateral carotid angioplasty.
A angioplastia carotídea constitui uma opção terapêutica eficaz para o tratamento da doença carotídea aterosclerótica significativa, estando por vezes associada a alterações hemodinâmicas transitórias que influenciam a pressão arterial. Apresenta-se o caso clínico de uma mulher de 73 anos de idade com hipertensão arterial crónica refractária, que após ser submetida a angioplastia carotídea bilateral permaneceu normotensa durante um follow up de três anos.
According to recently published clinical evidence, carotid angioplasty with stenting is an effective and safe alternative to endarterectomy for the treatment of significant carotid disease 1. However, both therapeutic options are associated with episodes of hemodynamic instability (increase or decrease in blood pressure [BP] and bradycardia) during and after the procedures, due to transient dysfunction of the baroreflex system, which in the case of carotid artery stenting results from mechanical distension of carotid sinus (CS) baroreceptors 2-5.
The baroreflex is the most important mechanism in short-term regulation of blood pressure and heart rate (HR). It acts via the autonomic nervous system, with baroreceptors in the CS being triggered by stretching, modulating blood pressure through reciprocal changes in sympathetic and vagal activity (increasing parasympathetic and decreasing sympathetic stimulation). Although the role of carotid baroreceptors in acute blood pressure regulation is well documented, their involvement in long-term regulation remains unclear. The potential benefit of chronic CS baroreceptor stimulation to treat hypertension is currently being investigated 6.
Case reportA 73-year-old female patient, obese (body mass index: 29), with dyslipidemia and known coronary artery disease (CAD) (angioplasty of the circumflex artery with implantation of a bare-metal stent performed in 2000), was referred to cardiology consultation for refractory hypertension. She presented Canadian Cardiovascular Society (CCS) class II effort angina, and was under therapy with atenolol 100mg id, nifedipine 30mg id, irbesartan 300mg id, isosorbide mononitrate 60mg id, rosuvastatin 20mg id, and aspirin 100mg id. Despite the patient's assurance of compliance with the prescribed therapy, her BP remained above recommended levels (systolic BP 150-160mmHg and diastolic BP 80-90mmHg).
Following detection of a bilateral carotid murmur on physical examination, Doppler ultrasound was performed which revealed significant stenosis of both internal carotid arteries (ICAs). Peak systolic velocities measured by Doppler indicated 85 % and 80 % stenosis of the right and left ICA, respectively. Carotid angiography during hospitalization confirmed the above lesions, and coronary angiography excluded stent restenosis or CAD progression.
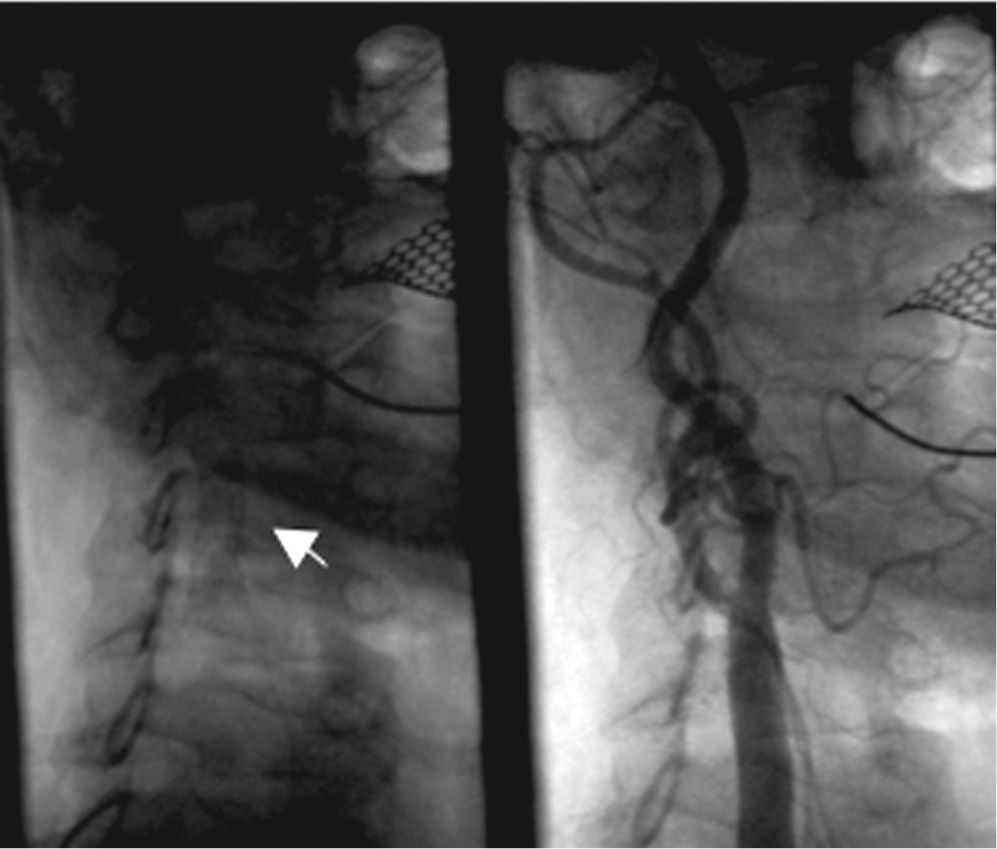
The patient then underwent staged carotid angioplasty (right ICA in February 2007 and left ICA three months later), with implantation of PRECISE® self-expandable metal stents - 7 × 30mm in the right carotid (Figure 1) and 6 × 30mm in the left carotid (Figure 2). The first intervention was uneventful, but during the second procedure the patient developed severe hypotension (65/40mmHg), which responded to volume loading and the Trendelenburg position. She was discharged three days later with normal BP (120/80mmHg), and all antihypertensive medication was discontinued.
The patient was monitored regularly during a three-year follow-up, and remained normotensive, with no BP-lowering medication except atenolol 50mg (reintroduced to prevent effort angina), and with baseline HR of 70-80bpm.
DiscussionCarotid stenosis is usually the result of accumulation of calcified atheromatous plaques in the bifurcation of the common carotid artery, affecting the origin of the internal carotid artery. This region is anatomically close to the CS baroreceptors, which are sensitive to pressure exerted on the vessel wall and control blood pressure by regulatory centers through counter-regulatory mechanisms. Impulses originating in the CS are transmitted via the glossopharyngeal nerve to the nucleus of the solitary tract (NST) located in the medulla oblongata. CS stimulation inhibits sympathetic neurons of the NST, thus reducing sympathetic vascular tone and hence BP. Simultaneous activation of the nucleus ambiguus and the dorsal nucleus of the vagus nerve increases vagal stimulation, resulting in a reduction in HR.
The presence of calcified atheromatous plaques in the CS leads to chronic baroreceptor stimulation in response to small variations in pressure, since the thicker and more calcified the wall, the more rapid and efficient the transmission of pressure changes. Endoluminal distension of the arterial wall during balloon inflation and stent expansion can thus produce a hypotensive response 2.
Numerous studies have demonstrated that acute hemodynamic changes during and after carotid artery stenting increase the risk of mortality and stroke in the perioperative period 3. However, no long-term beneficial effect has been reported following unilateral or bilateral carotid angioplasty with stenting, particularly in patients with refractory hypertension.
Attempts have been made to reduce BP through afferent CS stimulation since the 1960s, when research began into baroreflex modulation as a treatment for refractory hypertension and angina 4. There is now evidence to suggest that BP can be reduced effectively through electrical stimulation of the CS 5, and a clinical trial is currently underway to assess the efficacy of an implantable device for the treatment of refractory hypertension 7. Experimental studies have demonstrated that carotid angioplasty in hypertensive dogs can cause chronic hypotension 8.
The case presented raises the possibility that mechanical distension of both carotid sinuses by metal stent implantation, resulting in sustained baroreflex stimulation, can lead to chronic BP lowering. The varying contribution of the baroreflex and sympathetic nervous systems to long-term BP modulation, as well as differences in the anatomical and functional properties of the CS, may explain the variability of BP response following this type of procedure 9. In contrast to the changes in BP in this patient, there was no significant reduction in HR following carotid angioplasty. Baseline HR and its variability depend primarily on regulation by the parasympathetic nervous system, whose function appears to decline with age, particularly in hypertensives 9. This may explain the limited influence of the baroreflex on HR in our patient.
ConclusionCarotid disease arises from an underlying chronic atherosclerotic process and is therefore frequently associated with hypertension. Carotid angioplasty is an effective treatment for significant carotid artery stenosis, but while safe, it is frequently associated with transient bradycardia and hypotension. However, the case described shows the potential long-term hemodynamic effect induced by sustained bilateral CS stimulation. Although this is an uncommon clinical response, it may be beneficial in patients with severe hypertension undergoing bilateral carotid angioplasty, leading to improvement in long-term BP control.
Conflicts of interestThe authors have no conflicts of interest to declare.