Randomized controlled trials comparing stress cardiac magnetic resonance (CMR) and single-photon emission computed tomography (SPECT) suggest similar diagnostic accuracy for detecting obstructive coronary artery disease (CAD). There are few data on whether this remains true in routine clinical practice.
The aim of this study was to assess clinical and angiographic characteristics of patients undergoing invasive coronary angiography (ICA) after stress CMR or SPECT, and to compare their positive predictive value with published results from the CE-MARC trial.
MethodsIn this retrospective tertiary-center analysis, we included 429 patients undergoing ICA after a positive stress CMR or positive SPECT performed within the previous 12 months. Obstructive CAD was defined as any coronary artery stenosis ≥50% in a vessel compatible with the ischemic territory on stress testing.
ResultsOf the total 429 patients, 356 (83%) were referred after a positive SPECT, and 73 (17%) after a positive stress CMR. Patients did not differ according to age, cardiovascular risk factors, previous revascularization or left ventricular dysfunction, but patients with SPECT were more frequently male (p=0.046). The prevalence of obstructive CAD was similar in patients with positive SPECT vs. positive stress CMR (76.1% vs. 80.8%, respectively, p=0.385). The positive predictive values of both techniques were similar to those reported in the CE-MARC trial.
ConclusionIn this tertiary center analysis, stress CMR and SPECT showed similar positive predictive values, comparable to those reported in the CE-MARC trial. This finding supports the emerging adoption of CMR in clinical practice for the diagnosis and management of CAD.
Os ensaios randomizados que compararam a ressonância magnética cardíaca de stress (RMC) e a cintigrafia de perfusão miocárdica (SPECT) sugerem acuidade diagnóstica semelhante na avaliação da doença arterial coronária obstrutiva (DAC). Existem poucos dados acerca da sua reprodutibilidade na prática clínica diária. O objetivo deste estudo foi avaliar as características clínicas e angiográficas dos doentes submetidos a coronariografia invasiva (CAT) após RMC ou SPECT e comparar o seu valor preditivo positivo com os resultados publicados no estudo CE-MARC.
MétodosNesta análise retrospetiva de centro único, incluímos 429 doentes submetidos a CAT, após RMC positiva ou SPECT positiva, realizada nos últimos 12 meses. DAC obstrutiva foi definida como qualquer estenose superior ou igual a 50% num vaso compatível com o território isquémico.
ResultadosNum total de 429 pacientes, 356 (83%) foram encaminhados após SPECT positiva e 73 (17%) após RMC positiva. Os doentes não diferiram quanto à idade, fatores de risco cardiovascular, revascularização prévia ou disfunção ventricular esquerda, mas a percentagem de doentes do sexo masculino foi maior no grupo referenciado após SPECT (p=0,046). A prevalência de DAC obstrutiva foi semelhante nos doentes referenciados após SPECT positiva versus RMC positiva (76,1% versus 80,8%, respetivamente, p=0,385). Os valores preditivos positivos de ambas as técnicas foram semelhantes aos reportados no estudo CE-MARC.
ConclusãoNesta análise de centro terciário, a RMC de stress e a SPECT mostraram valores preditivos positivos semelhantes, comparáveis aos publicados no estudo CE-MARC. Estes dados apoiam a adoção emergente da RMC na prática clínica para o diagnóstico e tratamento da DAC.
Despite some controversy, testing for myocardial ischemia remains an important way to diagnose obstructive coronary artery disease (CAD), assess prognosis, and guide revascularization.1 Clinicians now have a wide gamut of ischemia tests to choose from, ranging from exercise ECG to sophisticated imaging tests such as positron emission tomography. For a number of reasons, single-photon emission computed tomography (SPECT) is the most commonly used imaging ischemia test in many countries, including Portugal.2 The availability and evidence supporting stress cardiac magnetic resonance (an alternative to SPECT that does not use ionizing radiation) have increased significantly in the last decade, but it is still far less used than SPECT.3–6 Randomized controlled trials comparing stress CMR and SPECT suggest similar diagnostic accuracy for detecting obstructive coronary artery disease (CAD).7–9 The CE-MARC (Clinical Evaluation of MAgnetic Resonance imaging in Coronary heart disease) study was the largest prospective study comparing CMR with SPECT, and demonstrated similar positive predictive value and confirmed the good diagnostic accuracy of CMR.9 However, there are few data on whether this remains true in routine clinical practice.
ObjectivesThe aim of this study was to assess the clinical and angiographic characteristics of patients undergoing invasive coronary angiography (ICA) after a positive stress CMR or positive SPECT, and to compare their positive predictive value with published results from the CE-MARC trial.
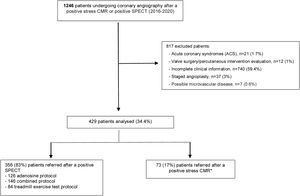
MethodsPatient selectionPatients with known or suspected chronic coronary syndrome undergoing ICA after a positive stress CMR or stress SPECT performed within the previous 12 months were identified in a single center cardiac catheterization laboratory registry (the ACROSS registry – Angioplasty and Coronary Revascularization on Santa Cruz Hospital), containing all ICA performed between 1 January 2016 and 31 December 2020.
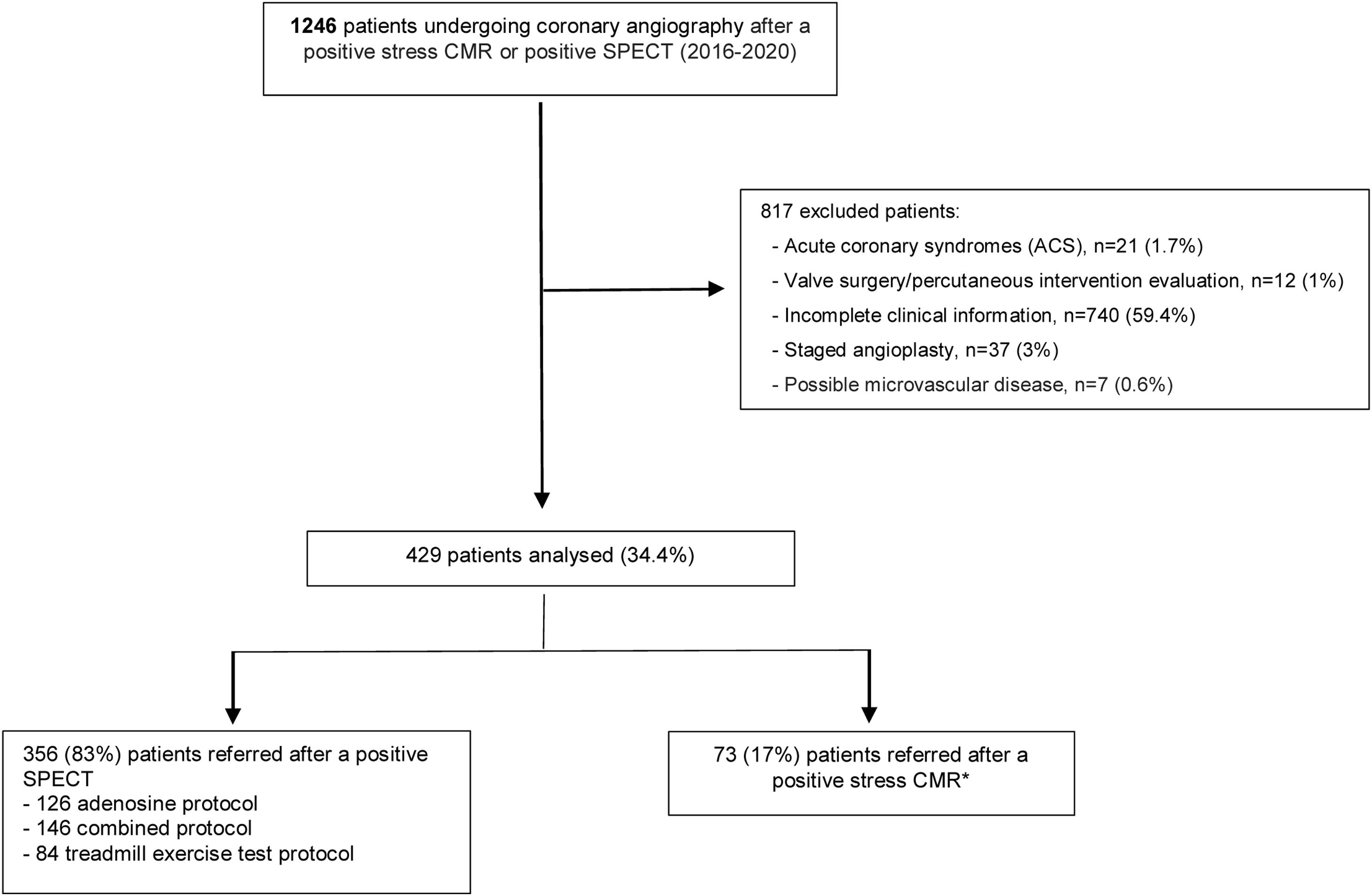
Exclusion criteria comprised suspected or confirmed acute coronary syndrome (ACS), possible microvascular disease as reported in the original stress test, staged angioplasty (performed later separate from the initial diagnostic ICA), moderate or severe heart valve disease and missing data on key variables (see Figure 1). A significant number of patients were excluded due to missing information, which in most cases was related to incomplete data from stress test reports performed outside our institution.
All patients were >18 years of age and gave written informed consent to be included in the registry, which was revised and approved by the local ethics committee. The study protocol complies with the ethical guidelines of the 1975 Declaration of Helsinki.
Clinical dataThe demographic and clinical characteristics of each patient were identified from their medical records. Procedural data were collected by the attending team at the time of the procedure. Stress test results, including ischemia location and severity, were classified as reported by their primary readers. Referral for invasive coronary angiography was left to the discretion of the referring physician.
Obstructive CAD was defined on ICA as any coronary artery stenosis ≥50% in an epicardial vessel (>2 mm). The grading of stenosis severity was assessed by the interventional cardiologist performing the procedure, who also decided on the need for revascularization using all available clinical data, including noninvasive test results.
ProceduresSingle-photon emission computed tomographyTwo-hundred and forty-five patients (68.8%) underwent stress SPECT at our center, while 111 (31.2%) patients underwent the test at other centers. Despite being performed in different institutions, several features of SPECT testing remained constant: all patients received 99mTc tetrofosmin at a dose of 400 MBq adjusted by weight to a maximum 600 MBq per examination (effective dose 6–9 mSv) as recommended in current guidelines10; all patients underwent stress/rest gated SPECT (unless stress imaging was considered normal), using either treadmill exercise testing, adenosine perfusion (140 mcg/kg/min during 6 minutes), or a combined adenosine/low intensity treadmill protocol; CT attenuation correction was applied in all studies. In all cases, reporting was based on visual qualitative analysis performed by a cardiologist and/or a nuclear medicine physician with level III-equivalent experience. The segmentation model used by the primary readers was the American Heart Association 17-segment model. The results were classified as reported by their primary readers. Transient ischemic dilation of the left ventricle, right ventricular uptake, and transient ischemic dysfunction were not reported in any of the SPECT studies. The effective radiation dose was converted to mSv in accordance with current literature.11 Briefly, a factor of 0.0080 mSv/MBq−10 (after exercise) and 0.0069 mSv/MBq−10 (at rest) were used for the conversion of injected activity in SPECT.
Cardiac magnetic resonance perfusion imagingStress CMR was performed at our center in 56 patients (76.7%) using a 1.5 T scanner and at others centers in 17 patients (23.3%), using 1.5 T or 3.0 T scanners. All CMR protocols included saturation-recovery imaging with balanced steady state free precision and single-shot and gradient-echo sequences in three short-axis slices. Regarding stress test, an adenosine protocol was performed in all stress CMR (adenosine perfusion 140 mcg/kg/min increased up to 210 mcg/kg/min if insufficient chronotropic response). Patients were instructed not to consume caffeinated beverages in the 12 hours prior. Visual qualitative analysis was performed; CMR images were reviewed by one level three cardiologist. The segmentation model used by the primary readers was the AHA 17-segment model. Stress test results, including ischemia location and severity, were classified as reported by their primary readers.
Statistical analysisContinuous variables are expressed as mean±SD or median (interquartile range) and were compared with the use of an unpaired t-test or the Mann–Whitney U test. Categorical variables are expressed as proportions (%) and were compared with the use of the chi-square test. Corresponding 95% confidence intervals were calculated with the Wilson score method. A two-sided p value of <0.05 was considered to indicate statistical significance. Statistical analysis was performed with the use of SPSS Statistics Version 21.0.
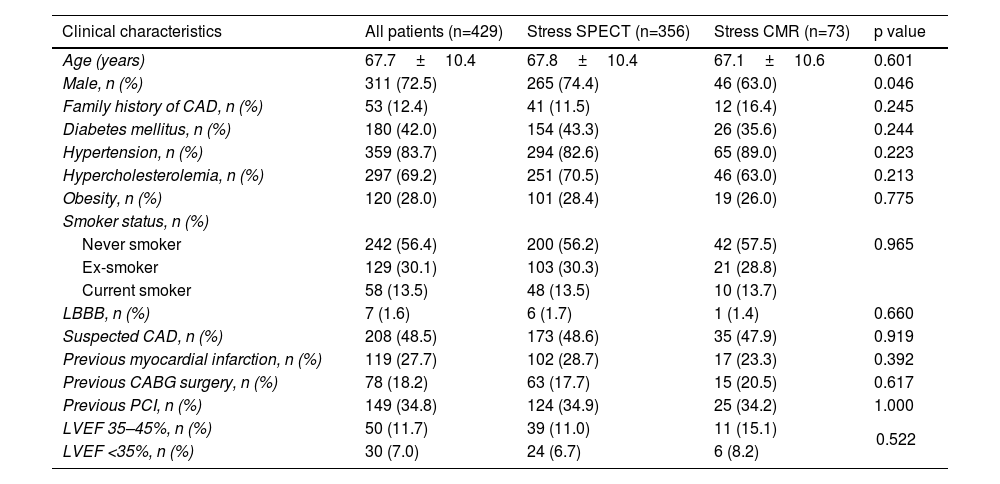
ResultsFrom a total of 1246 patients undergoing ICA after a positive stress SPECT or stress CMR during the study period, 429 were included in the analysis: 356 patients (83%) were referred after a positive stress SPECT, and 73 (17%) after a positive stress CMR (Figure 1). The clinical characteristics of the study population are presented in Table 1. Apart from a different gender distribution, there were no significant differences between patients referred after SPECT and after CMR regarding age, cardiovascular risk factors, previous revascularization, left ventricular dysfunction, or left bundle branch block.
Clinical characteristics.
| Clinical characteristics | All patients (n=429) | Stress SPECT (n=356) | Stress CMR (n=73) | p value |
|---|---|---|---|---|
| Age (years) | 67.7±10.4 | 67.8±10.4 | 67.1±10.6 | 0.601 |
| Male, n (%) | 311 (72.5) | 265 (74.4) | 46 (63.0) | 0.046 |
| Family history of CAD, n (%) | 53 (12.4) | 41 (11.5) | 12 (16.4) | 0.245 |
| Diabetes mellitus, n (%) | 180 (42.0) | 154 (43.3) | 26 (35.6) | 0.244 |
| Hypertension, n (%) | 359 (83.7) | 294 (82.6) | 65 (89.0) | 0.223 |
| Hypercholesterolemia, n (%) | 297 (69.2) | 251 (70.5) | 46 (63.0) | 0.213 |
| Obesity, n (%) | 120 (28.0) | 101 (28.4) | 19 (26.0) | 0.775 |
| Smoker status, n (%) | ||||
| Never smoker | 242 (56.4) | 200 (56.2) | 42 (57.5) | 0.965 |
| Ex-smoker | 129 (30.1) | 103 (30.3) | 21 (28.8) | |
| Current smoker | 58 (13.5) | 48 (13.5) | 10 (13.7) | |
| LBBB, n (%) | 7 (1.6) | 6 (1.7) | 1 (1.4) | 0.660 |
| Suspected CAD, n (%) | 208 (48.5) | 173 (48.6) | 35 (47.9) | 0.919 |
| Previous myocardial infarction, n (%) | 119 (27.7) | 102 (28.7) | 17 (23.3) | 0.392 |
| Previous CABG surgery, n (%) | 78 (18.2) | 63 (17.7) | 15 (20.5) | 0.617 |
| Previous PCI, n (%) | 149 (34.8) | 124 (34.9) | 25 (34.2) | 1.000 |
| LVEF 35–45%, n (%) | 50 (11.7) | 39 (11.0) | 11 (15.1) | 0.522 |
| LVEF <35%, n (%) | 30 (7.0) | 24 (6.7) | 6 (8.2) | |
CABG: coronary artery bypass graft; CAD: coronary artery disease; LBBB: left bundle branch block; LVEF: left ventricular ejection fraction; PCI: percutaneous coronary intervention.
Among the 356 patients referred after a positive SPECT, 84 (24%) underwent a treadmill exercise protocol, 126 (35%) an adenosine stress test, and 146 (41%) a combined protocol using both adenosine and exercise. The mean radiation exposure in the SPECT protocol (stress and rest) was 10.3±1.7 mSv.
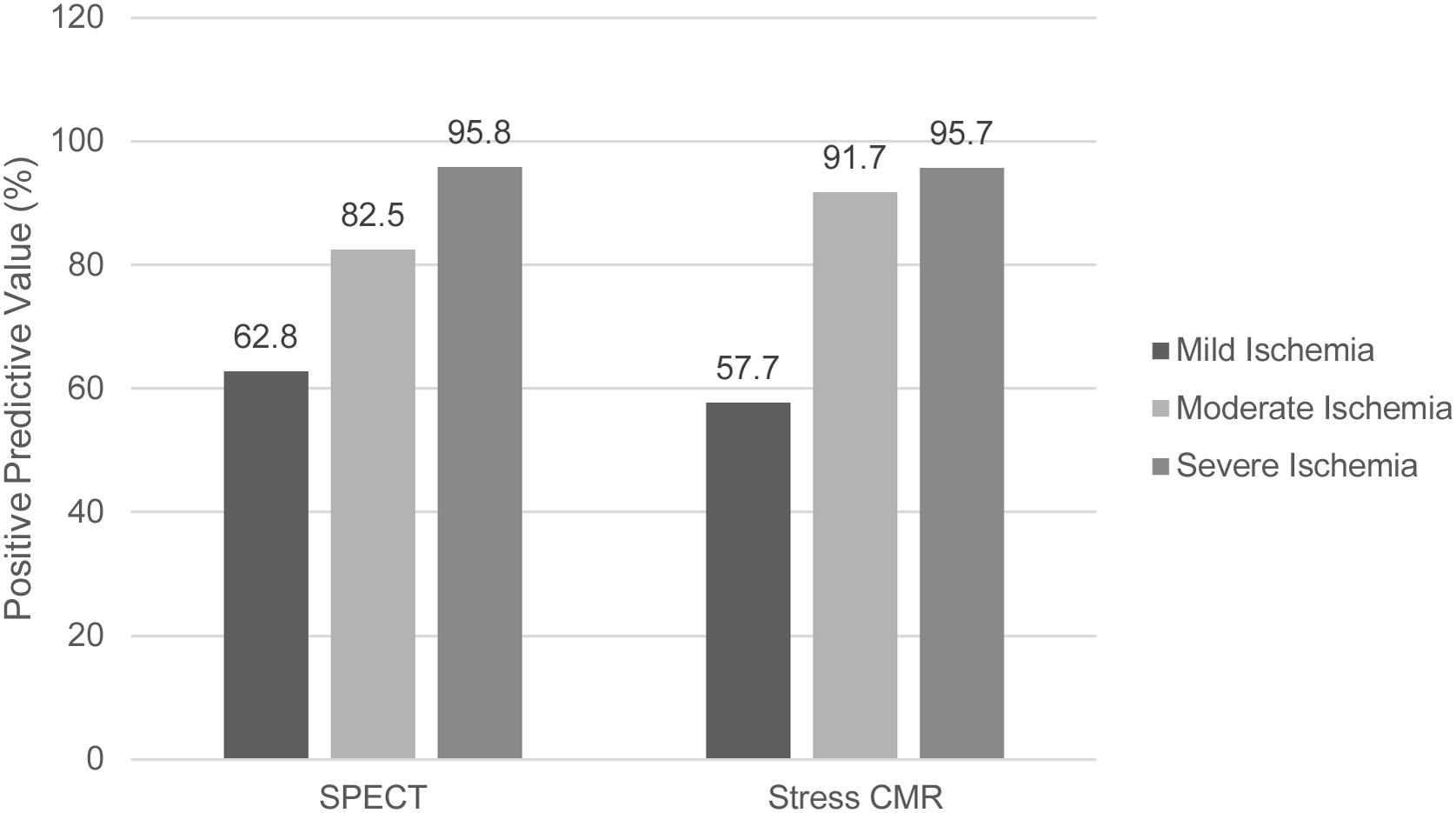
Ischemia severity in SPECT was reported as mild, moderate, and severe in 50.6%, 22.5%, and 27.0% of patients, respectively. In patients undergoing stress CMR, the corresponding distribution of ischemia severity was 35.6%, 32.9%, and 31.5%, respectively.
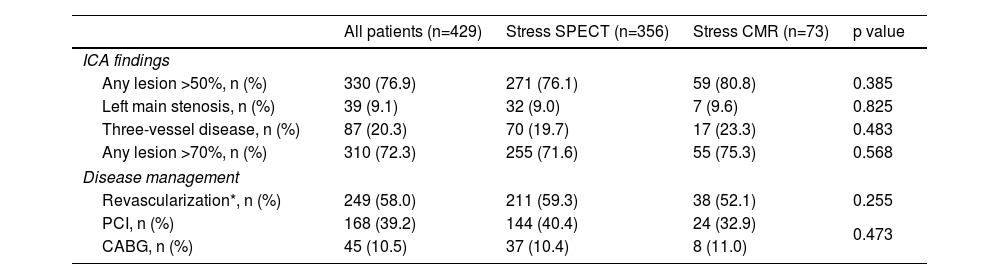
The median time between stress imaging and ICA was 100 days (interquartile range (IQR) 59–173) for SPECT, and 87 days (IQR 40–155) for CMR. Overall, 330 patients (76.9%) had obstructive CAD on ICA. The prevalence of obstructive CAD was similar in patients with positive SPECT vs. positive stress CMR (76.1% vs. 80.8%, respectively, p=0.385). There were also no significant differences in the prevalence of left main or 3-vessel disease – 9.0% vs. 9.6%, p=0.871, and 19.7% vs. 23.3% p=0.483, respectively (Table 2).
Angiographic characteristics.
| All patients (n=429) | Stress SPECT (n=356) | Stress CMR (n=73) | p value | |
|---|---|---|---|---|
| ICA findings | ||||
| Any lesion >50%, n (%) | 330 (76.9) | 271 (76.1) | 59 (80.8) | 0.385 |
| Left main stenosis, n (%) | 39 (9.1) | 32 (9.0) | 7 (9.6) | 0.825 |
| Three-vessel disease, n (%) | 87 (20.3) | 70 (19.7) | 17 (23.3) | 0.483 |
| Any lesion >70%, n (%) | 310 (72.3) | 255 (71.6) | 55 (75.3) | 0.568 |
| Disease management | ||||
| Revascularization*, n (%) | 249 (58.0) | 211 (59.3) | 38 (52.1) | 0.255 |
| PCI, n (%) | 168 (39.2) | 144 (40.4) | 24 (32.9) | 0.473 |
| CABG, n (%) | 45 (10.5) | 37 (10.4) | 8 (11.0) | |
CABG: coronary artery bypass graft; CAD: coronary artery disease; LVEF: left ventricular ejection fraction; PCI: percutaneous coronary intervention.
Regarding ischemia results in patients with left main or/and 3-vessel disease, moderate or severe ischemia was reported in 70.1% and in 75% of patients who underwent SPECT and CMR, respectively (p=0.786). Revascularization was performed or planned in 59.3% of patients in the SPECT group, and 52.1% of those in the stress CMR group (p=0.255). A sub-analysis comparing SPECT performed with pharmacologic test and CMR revealed similar results (Supplemental Table 1).
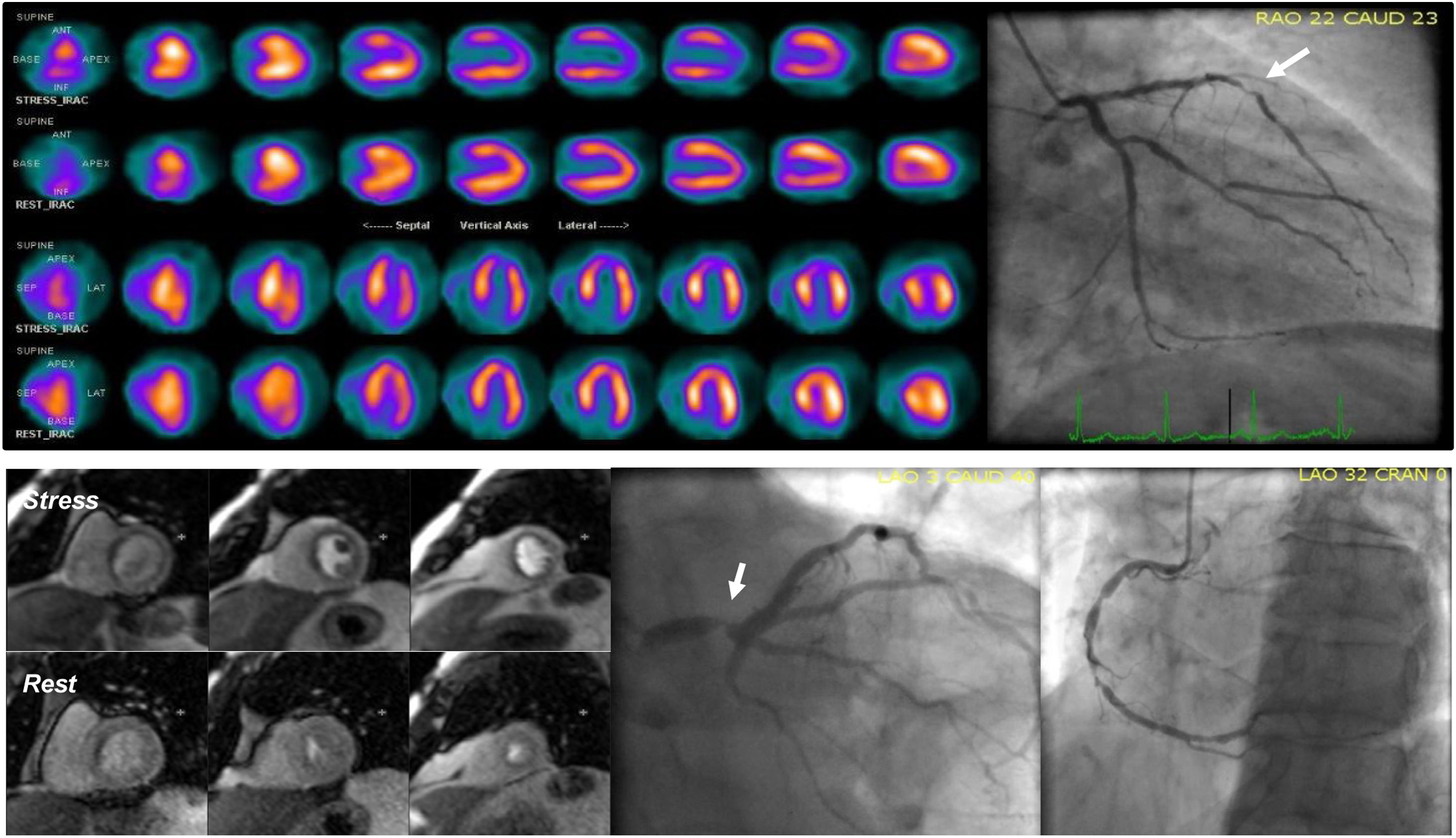
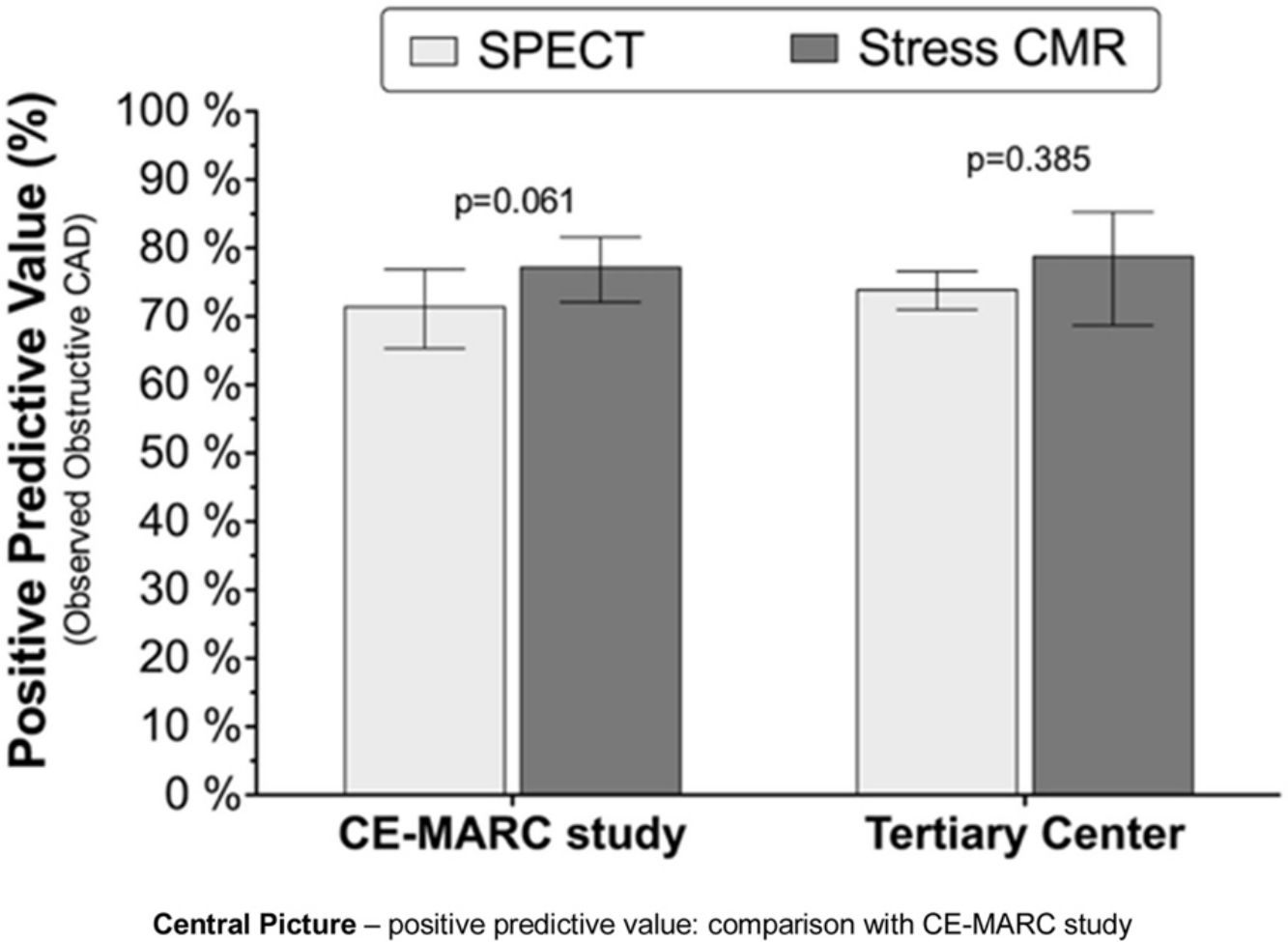
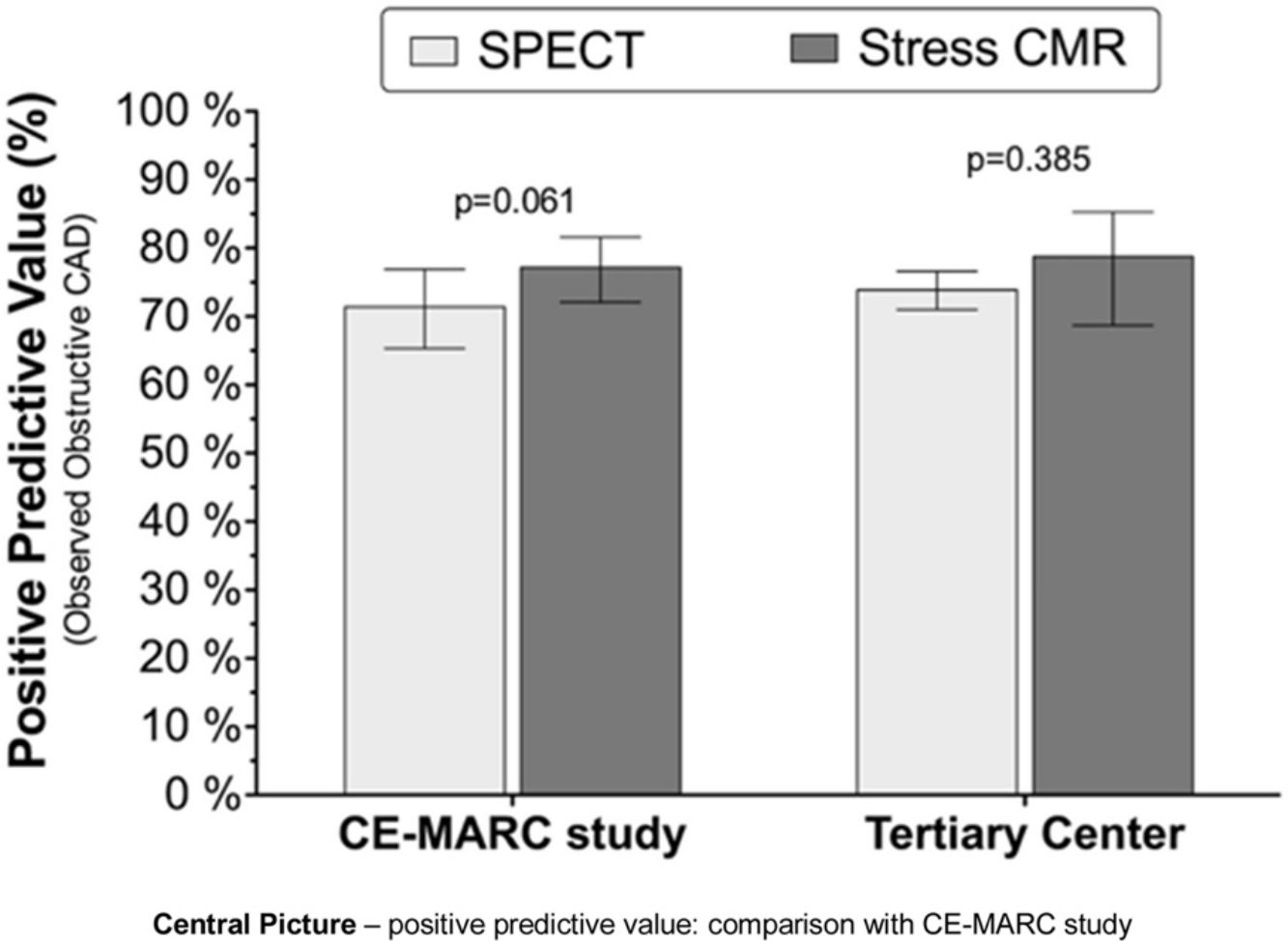
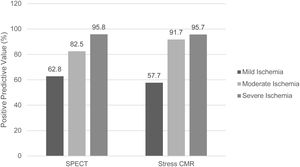
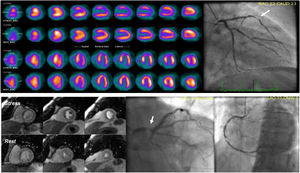
The positive predictive value (PPV) for obstructive CAD was 76.1% (95% CI 71.4–80.3) for SPECT and 80.8% (95% CI 70.3–88.2) for stress CMR, respectively (p=0.385). These figures would increase to 89.8% (95% CI 84.4–93.4) and 93.6% (95% CI 82.8–97.8), respectively, if patients reported as having only mild ischemia were excluded (Figure 2). The positive predictive values of both techniques were similar to those reported in the CE-MARC trial (Central Picture). Figure 3 shows examples of SPECT and CMR and respective ICA.
Examples of SPECT and CMR and respective ICA. Top panel – sixty-five-year-old male with anterior and apical ischemia in SPECT; ICA shows a severe stenosis in left anterior descending artery (white arrow). Bottom panel – seventy-nine-year-old male, CMR shows a global defect perfusion, in relation with severe three-vessel ischemia; ICA revealed severe stenosis of left main, and obstructive lesions in right coronary artery.
Significant incidental findings were identified in seven patients undergoing stress CMR: intraventricular thrombus (three patients), hypertrophic cardiomyopathy (one patient), myopericarditis (two patients), and significant aortic regurgitation (one patient).
DiscussionIn this retrospective, real-world study, we assessed the clinical and angiographic characteristics of patients undergoing ICA after a positive stress CMR or positive SPECT and compared their PPV for angiographically significant CAD. These two populations of patients did not differ in clinical characteristics, except for a higher proportion of men in those referred after SPECT. Regarding angiographic characteristics, the prevalence of obstructive CAD and left main or three-vessel disease was similar in both groups.
Several previously published papers, including single-center12–16 and multi-center studies,7–9 have validated the high accuracy of stress CMR to detect CAD. Meta-analyses have confirmed the high accuracy of stress CMR in CAD diagnosis,17 and some of them have shown differences in specificity with better results for stress CMR compared with SPECT.18–20 The CE-MARC study9 was the largest prospective evaluation to date of CMR versus SPECT, demonstrating a higher diagnostic accuracy of CMR (sensitivity and negative predictive value), but similar specificity and positive predictive value. In our real-world study, the positive predictive value of SPECT and stress CMR was similar to that reported in the CE-MARC trial (Central Picture). Several differences between our cohort and the CE-MARC study cohort are worth noting. In the CE-MARC study, patients with CABG were excluded, and only 11% of patients had previous history of revascularization or acute coronary syndrome. In our cohort, patients with previous CABG were included (comprising 18.2% of the total population), and as many as 53% had previous revascularization. The presumably more complex CAD is probably more representative of the reality of a tertiary center.
Previous SPECT studies with a higher prevalence of CAD and 3-vessel disease revealed a lower diagnostic performance in these patients, whereas CMR studies showed a better performance.18 In our study there was no significant difference in PPV between these two imaging modalities. Moreover, ischemia burden was similar in patients with left main or/and three-vessel disease referred after positive stress CMR or SPECT.
Despite the validated performance of stress CMR and its recognition in international guidelines,1 the use of stress CMR in our country has increased only slightly in recent years, while stress ECG and SPECT continue to be the most frequently used tests.2 Possible explanations include wider accessibility of stress ECG and SPECT, less familiarity of practicing physicians with this imaging modality21 and the erroneous idea that CMR is an expensive technique, despite growing evidence of cost-effectiveness of this test.22,23 In our study, only 17% of the patients were referred after a positive stress CMR, reflecting its use in present clinical practice. Possibly, differences between techniques could become clearer if more patients were referred for stress CMR.
Both techniques have some limitations. For SPECT, these include the exposure to ionizing radiation, limited spatial resolution, and attenuation artifacts. For CMR, limitations include dark rim artifacts, claustrophobia, end-stage kidney disease under dialysis, and some implanted electronic medical devices. One of the potential advantages of CMR relies on its ability to simultaneously assess for valvular function, cardiomyopathy, and aortic disease, among others. As seen in this study, incidental cardiac findings at CMR with potential implications for patient management (such as intraventricular thrombus) are not uncommon in these patients.
Several limitations of this study should be acknowledged. First, since this was a retrospective, single-center study, data were extracted from a clinical database of patients who underwent ICA, resulting in selection bias. Second, there was no core lab interpretation of angiography, SPECT or CMR images, and different SPECT stress modes and protocols were used. Third, since accurate information about pain characteristics was not available in our registry, it was not possible to ascertain the pretest probability of obstructive CAD and the appropriateness of stress imaging. This may have influenced the results since the predictive power of noninvasive testing is affected by the pretest probability. Fourth, obstructive CAD was established using an exclusively anatomic criterion, since invasive fractional flow reserve was only performed in a minority of cases. Fifth, it should be noted that this was not a head-to-head comparison between stress SPECT and CMR (patients only underwent one of these tests, not both), and that all patients undergoing ICA had a positive stress test. Finally, roughly two thirds of the surveyed patients (most of them with tests performed at other institutions) had to be excluded due to missing clinical data, leading to an inevitable referral bias. So, even though this was a “real-word” study, it may not be representative of the reality at a national level, since the vast majority of these tests were performed in a tertiary high-volume University Hospital. This study design does not allow for the assessment of other measures of diagnostic accuracy such as sensitivity, specificity, and negative predictive values since these would require all patients to undergo ICA irrespective of the non-invasive test result.
ConclusionIn this single tertiary center analysis, stress CMR and SPECT showed similar positive predictive values, comparable to those reported in the CE-MARC trial. This finding supports the emerging adoption of CMR in clinical practice for the diagnosis and management of CAD.
Conflicts of interestThe authors have no conflicts of interest to declare.