To evaluate in untreated subjects the reproducibility of mean values and four circadian patterns between two ambulatory blood pressure monitoring (ABPM) recordings separated by 1–11 months.
MethodsWe performed a retrospective analysis of 481 individuals (59% women) evaluated by ABPM on two occasions, visit 1 (V1) and 2 (V2), separated by 5.5+0.2 months. Four circadian patterns were defined by night/day systolic blood pressure (SBP) ratios: reverse dippers (RD), ratio >1.0; non-dippers (ND), ratio 0.9–1.0; dippers (D), ratio 0.8–<0.9; and extreme dippers (ED), ratio <0.8. Coefficients of correlation and concordance between the ABPM values at V1 and V2 and the reproducibility of the RD, ND, D and ED patterns were calculated by the percentage of the same profile from V1 to V2.
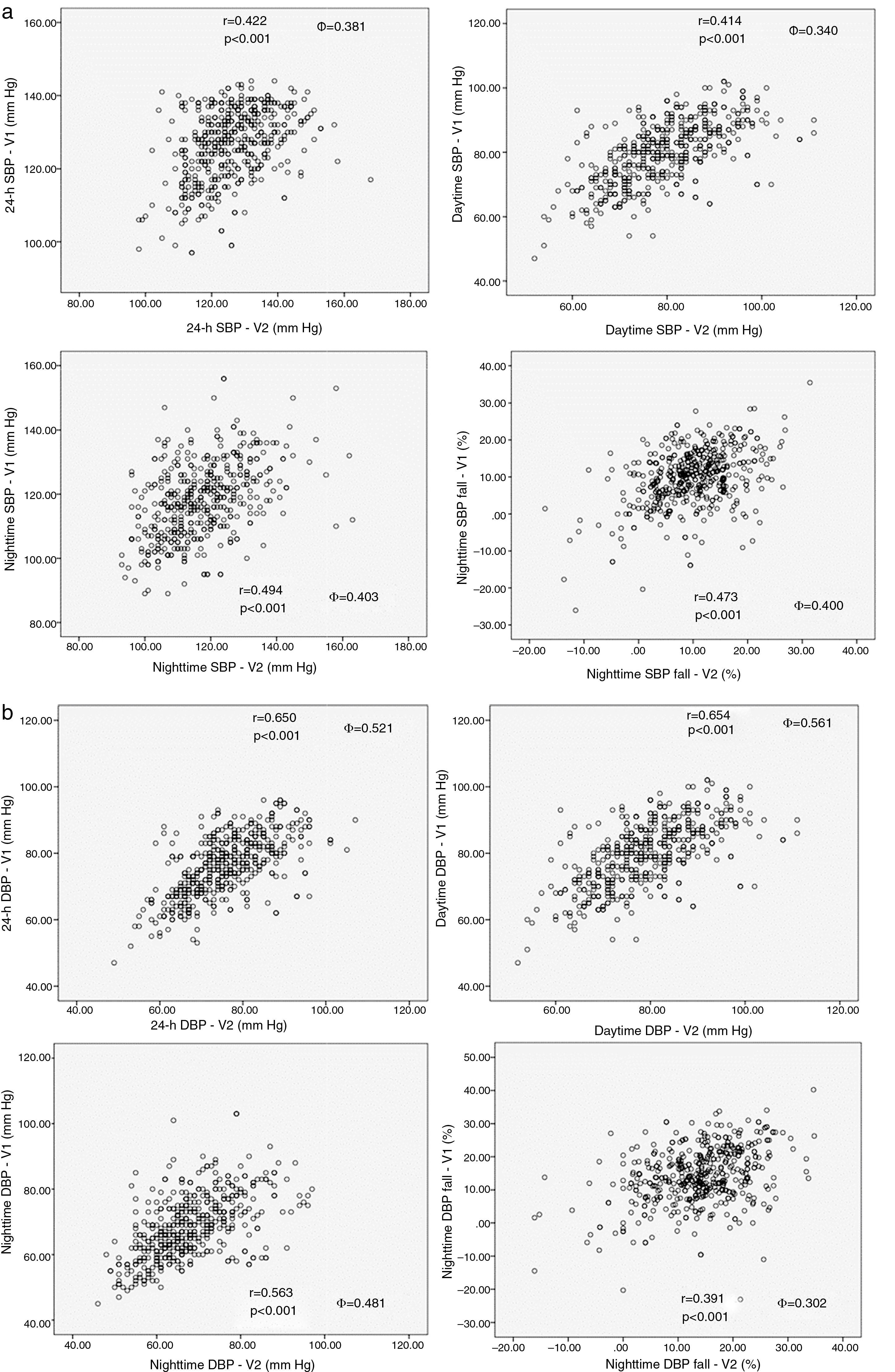
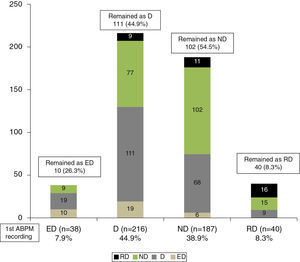
ResultsMean 24-h blood pressure (BP) at V1 and V2 was 126.8/75.9±0.5/0.5 vs. 126.5/75.7±0.5/0.4 mmHg (NS). Nighttime SBP fall was 9.8±0.4 (V1) and 9.6±0.3% (V2) (NS). The correlation coefficient of ABPM data at V1 vs. at V2 was 0.41–0.69 (p<0.001) and the concordance coefficient was 0.34–0.57 (p<0.01). At V1, 38 subjects were classified as ED (7.9%); D, n=216 (44.9%), 187 as ND (38.9%) and 40 as RD (8.3%). At V2 only 26.3% of ED, 44.9% of D, 54.5% of ND and 40% of RD maintained the same profile as at V1.
ConclusionIn untreated subjects ABPM has high reproducibility for mean values but only modest reproducibility for circadian profiles, thereby challenging the prognostic value of BP dipping patterns.
Avaliar em indivíduos não medicados a reprodutibilidade dos valores médios e dos quatro perfis circadiários entre dois registos de pressurometria ambulatória de 24 horas (MAPA) separados de 1-11 meses.
MétodosAnálise retrospetiva de 481 indivíduos (59% mulheres) avaliados por MAPA em dois dias, visita um (V1) e visita dois (V2) separados por 5,5 + 0,2 meses. Perfis circadiários definidos pelos ratios noite/dia da pressão sistólica (PAS) em: reverted dippers, RD se ratio > 1,0, non-dippers, ND se ratio 0,9- < 1,0, dippers, D se ratio 0,8- < 0,9 e extreme dippers, ED se ratio < 0,8. Cálculo dos coeficientes de correlação (CCc) e de concordância (Φ) entre os valores da MAPA nas V1-V2 e a reprodutibilidade dos perfis RD, ND, D e ED em V1 pela proporção de indivíduos que permaneceram no mesmo perfil em V2.
ResultadosAs médias de 24 horas foram 126,8/75,9 ± 0,5/0,5 (V1) versus 126,5/75,7 ± 0,5/0,4 mm Hg (V2) (n.s.). A descida noturna da PAS foi 9,8 ± 0,4 (V1) e 9,6 ± 0,3% (V2) (n.s.). Entre os vários parâmetros da MAPA, os CC oscilaram 0,41-0,69 (p < 0,001) e os ΦC entre 0,34-0,57 (p < 0,01). Em V1, ED foram n = 38 (7,9%), D n = 216 (44,9%), ND n = 187 (38,9%) e RD n = 40 (8,3%). Em V2 somente mantiveram o perfil de V1, 26,3% dos ED, 44,9% dos D, 54,5% dos ND e 40% dos RD.
ConclusãoEm indivíduos não tratados, a reprodutibilidade a menos de um ano da MAPA é elevada para os valores médios mas modesta relativamente aos perfis circadiários, sugerindo baixa preditibilidade de risco cardiovascular dos perfis de descida noturna da pressão arterial.
Ambulatory blood pressure (BP) monitoring (ABPM) is the gold standard for assessment of overall BP load. ABPM has high predictive value for cardiovascular events and target organ damage, provides information on circadian BP patterns, and can be used to monitor the effects of various antihypertensive therapies.1–4
Several studies have shown that compared to a dipper pattern (nighttime BP fall of >10% or ratio of nighttime to daytime BP <0.9), the absence of the usual nighttime BP fall – non-dipper pattern – is associated with greater target organ damage,2,5 higher albuminuria levels,6 left ventricular hypertrophy,2 renal dysfunction7 and cerebrovascular lesions.8–11 However, an issue with ABPM is its reproducibility12–21 in two or more recordings separated in time with regard to mean 24-h, daytime and nighttime BP values and to dipper vs. non-dipper patterns. In a recent review of 12 studies,22 the reproducibility of circadian BP patterns in normotensive, hypertensive and diabetic individuals ranged between 29% and 92%. Furthermore, in most if not all of these studies only dipper and non-dipper patterns were analyzed, not other patterns such as extreme dipper or reverse dipper, the prognostic value of which differs from that of the classic patterns.23–25 Another little-studied question is the reproducibility of mean 24-h BP and circadian patterns by ABPM in individuals for whom the European guidelines1 recommend postponing initiation of antihypertensive medication in favor of monitoring BP by repeat ABPM after some months.
The aim of the present study is to evaluate the reproducibility of ABPM values and the four principal circadian patterns in untreated subjects undergoing two ABPM recordings separated by less than 12 months.
MethodsThe data for the study were taken from our database of ABPM records, a total of 21000 ABPM recordings. We selected only recordings from individuals aged over 18, with no cardiovascular events, not taking antihypertensive medication, not diabetic, and with office BP <150/95 mmHg, for whom ABPM had been requested by their attending physician. All subjects were at low or moderate to low cardiovascular risk according to the table in the European guidelines1 based on BP values and other cardiovascular risk factors. Only individuals whose attending physicians had requested a second ABPM recording within 12 months were included; those who took any antihypertensive medication or whose weight changed by more than 5% between the two recordings, and those with any cardiovascular complication, including arrhythmias, were excluded.
24-hour ambulatory blood pressure monitoringAll subjects underwent two 25-hour ABPM recordings using a SpaceLabs 90207 monitor (SpaceLabs Inc., Redmond, WA), measured on two normal working days or equivalent every 20 min during the day and every 30 min during the night. The device was fitted between 8.00 and 10.00 am. Data from the first hour of recording were excluded from the analysis, the following 24 h being used to calculate daytime and nighttime BP according to the individual's daily schedule of rising and going to bed, but fixed between 7.00 and 9.00 am and 11.00 pm and 1.00 am, respectively. Only records with more than 85% of valid recordings were analyzed. All procedures for fitting and recording have been described in detail in previous works by our group.26–28 Mean 24-h heart rate and 24-h, daytime and nighttime BP were calculated for each ABPM recording. Four circadian BP patterns were defined according to the guidelines1 by the ratio of nighttime to daytime systolic blood pressure (SBP) or the percentage of nighttime BP fall compared to daytime as reverse dippers (RD), ratio >1.0 (or nighttime fall >0%); non-dippers (ND), ratio 0.9–1.0 (or nighttime fall 9.9–0%); dippers (D), ratio 0.8–<0.9 (or nighttime fall 10–19.9%); and extreme dippers (ED), ratio <0.8 (or nighttime fall ≥20%).
No significant differences were observed between genders in the parameters analyzed.
Statistical analysisThe data are presented as means ± standard error of the mean if normally distributed or as percentages. Continuous variables were compared by analysis of variance with the Bonferroni correction for multiple comparisons, while categorical variables were compared using the chi-square test or Fisher's exact test. The following tests were used to assess the reproducibility of mean 24-h, daytime and nighttime BP values and the differences between the first and second ABPM recordings: (a) Pearson's correlation coefficient between the same data from the first and second ABPBM recordings; (b) the concordance coefficient (Φc)=2RΘxΘy/Θx2+Θy2+(μx−μy)2, where μx and μy are the means for the two variables and Θx2 and Θy2 are the corresponding variances29 (concordance coefficients are more suitable for assessing reproducibility, since they represent the dispersion of values around the line of identity, while correlation coefficients compare these values as a function of a regression line); and (c) standard deviations (SD) of the differences and coefficients of variation.14 The reproducibility of different dipping patterns was assessed by calculating the proportion of subjects who were in the same category at the second ABPM recording.30 Bland–Altman31 plots were used to provide a graphical comparison of the differences between the night/day ratios on the two recordings with the mean ratios for each subject; the differences were used to calculate the coefficient of reproducibility of the observed values. Values of p<0.05 were considered statistically significant.
ResultsA total of 481 individuals met the criteria and were included in the analysis. The mean interval between the two ABPM recordings was 5.5 months (1–11). The characteristics of the population are summarized in Table 1. The differences between the two recordings were 0.38 mmHg for 24-h SBP (95% confidence interval [CI]: −0.61–1.39, p=0.455) and 0.26 mmHg for 24-h diastolic blood pressure (DBP) (95% CI: −0.43–0.96, p=0.457). There were no significant differences between the two recordings in daytime or nighttime BP values or nighttime fall, although values tended to be lower on the second recording.
Characteristics of the study population (n=481) and comparison of absolute values, differences and coefficients of correlation and concordance in 24 h, daytime and nighttime blood pressure between the two recordings.
| V1 | V2 | Diff. | SD of Diff. | COV (%) | COR* | CoC* | |
|---|---|---|---|---|---|---|---|
| Age (years) | 49±1 | ||||||
| BMI (kg/m2) | 27.6±0.3 | ||||||
| Women (%) | 59% | ||||||
| V1–V2 interval (months) | 5.5±0.2 | ||||||
| Office SBP (mmHg) | 131.9±0.5 | 130.5±0.5 | 1.11±0.38 | 10.9±0.3 | 9.7±0.4 | 0.38 | 0.21 |
| Office DBP (mmHg) | 80.2±0.5 | 79.1±0.4 | 0.10±0.39 | 7.8±0.3 | 7.5±0.4 | 0.44 | 0.33 |
| 24-h SBP (mmHg) | 126.8±0.4 | 126.5±0.5 | 0.38±0.50 | 8.8±0.4 | 6.8±0.3 | 0.42 | 0.38 |
| 24-h DBP (mmHg) | 75.9±0.4 | 75.7±0.4 | 0.26±0.35 | 5.7±0.3 | 7.1±0.2 | 0.65 | 0.52 |
| 24-h HR | 73.2±0.5 | 72.9±0.5 | 0.70±0.38 | 6.7±0.2 | 7.7±0.3 | 0.69 | 0.57 |
| Daytime SBP (mmHg) | 131.2±0.5 | 130.6±0.6 | 0.55±0.54 | 9.9±0.4 | 7.6±0.3 | 0.41 | 0.34 |
| Daytime DBP (mmHg) | 79.8±0.4 | 79.2±0.5 | 0.52±0.39 | 6.4±0.3 | 8.1±0.4 | 0.65 | 0.56 |
| Nighttime SBP (mmHg) | 118.1±0.5 | 117.7±0.6 | 0.32±0.56 | 11.0±0.4 | 9.6±0.3 | 0.49 | 0.40 |
| Nighttime DBP (mmHg) | 68.4±0.4 | 68.2±0.4 | 0.10±0.41 | 6.5±0.3 | 9.1±0.2 | 0.56 | 0.48 |
| Nighttime SBP fall, % | 9.8±0.4 | 9.6±0.3 | 0.07±0.36 | 5.9±0.4 | 69.3±5.3 | 0.47 | 0.40 |
| Night/day SBP ratio | 0.900±0.004 | 0.902±0.003 | 0.002±0.002 | ||||
| Night/day DBP ratio | 0.858±0.004 | 0.862±0.004 | 0.012±0.013 | ||||
CoC: coefficient of concordance; COR: coefficient of correlation; COV: coefficient of variation; DBP: diastolic blood pressure; Diff.: difference; HR: heart rate; SBP: systolic blood pressure; SD: standard deviation; V1: first ABPM visit; V2: second ABMP visit.
As seen in Table 1 and Figure 1, the coefficient of correlation between 24-h, daytime and nighttime BP and nighttime fall ranged between 0.41 and 0.69 (p<0.001), with higher values for DBP than for SBP. The concordance coefficients were generally lower than the correlation coefficients, but still statistically significant (p<0.001). Table 1 also shows the SDs of the differences in 24-h, daytime and nighttime BP and the coefficient of variation from the first recording. Comparing the two recordings, the SDs of the differences varied between 5.7 and 11.0 mmHg, and the coefficient of variation ranged between 6.8% and 9.6%.
Based only on nighttime fall in SBP on the first recording, 38 individuals (7.9%) were classified as ED, 216 (44.9%) as D, 187 (38.9%) as ND and 40 (8.3%) as RD. As shown in Figure 2, between the first and second visits 26.3% of ED, 51.4% of D, 54.5% of ND and 40% of RD maintained the same pattern. In multivariate analysis, these rates of persistence remained after adjustment for age, gender, body mass index (BMI) and baseline 24-h SBP. Of those classified as D on the first recording, 77 (35.6%) changed to ND, 19 to ED and nine to RD, while of those classified as ND on the first recording, 68 (36.4%) changed to D, 11 to RD and six to ED. The individuals classified as D on the first recording who remained as D on the second (n=111) had significantly (p<0.01) lower night/day SBP (0.854±0.003) and DBP (0.807±0.005) ratios than those initially classified as D who changed to ND (night/day SBP and DBP ratios of 0.865±0.003 and 0.823±0.005, respectively).
Distribution of circadian blood pressure patterns on the first ABPM recording and analysis of reproducibility based on percentages of persistence or change in patterns between first and second recordings. Rates of persistence of circadian patterns were independent of age, gender, body mass index and 24-h blood pressure on the first recording. ABPM: ambulatory blood pressure monitoring; D: dippers; ED: extreme dippers; ND: non-dippers; RD: reverse dippers.
No differences were observed between genders in mean 24-h BP values in the two recordings: in women (n=260), 24-h SBP was 126.9/75.7±0.6/0.5 vs. 126.3/75.5±0.6/0.5 mmHg (NS) on first and second recordings, respectively, and in men (n=221), 24-h SBP was 127.0/76.1±0.5/0.5 vs. 126.8/75.9±0.6/0.5 mmHg (NS) on the first and second recordings, respectively. There was also no significant difference in the percentage of women whose circadian pattern did not change between the two recordings (127/239, 53.1%) and whose pattern did change (133/242, 54.9%).
On the basis of data in the ABPM reports, BMI could be calculated for 178/239 (74%) of those whose circadian pattern did not change and for 192/242 (79%) of those whose pattern did change. In the former, mean BMI changed from 27.8±0.5 to 27.7±0.4 kg/m2 (NS) between the two recordings, and from 27.6±0.4 to 27.7±0.4 kg/m2 (NS) in the latter.
DiscussionThe diagnostic and prognostic value of 24-h ABPM for the assessment of BP and its circadian variation has been clearly demonstrated and its use is recommended in the guidelines.1 However, questions remain concerning the reproducibility of BP levels and circadian patterns by ABPM.32 Most studies have been limited to analysis of dipper and non-dipper patterns only,22 in particular the known relationship between a non-dipper pattern and increased cardiovascular risk and target organ damage.5,25,33–37 One of the most important elements of the present study is its analysis of the reproducibility of ABPM over two recordings separated by less than 12 months in untreated individuals, considering not only dipper and non-dipper patterns22 but also extreme dipper and reverse dipper patterns, which are independently associated with various aspects of cardiovascular risk.2,11,38–40
Our results confirm those of other studies showing good reproducibility of mean 24-h BP values even when ABPM recordings are separated by weeks20,41,42 or months.15,19,43 In the present study mean 24-h, daytime and nighttime BP levels did not differ significantly between the two recordings, and the coefficients of correlation and concordance between the equivalent BP values on the two recordings were also significant. The SDs of the differences in 24-h BP ranged between 5.7 and 8.8 mmHg, with coefficients of variation of 6.8%–7.1%, which is within the limits observed in other studies of ABPM recordings separated by weeks20,41,42 or months.15,19,43 Although better indices of reproducibility can be obtained by using shorter intervals between recordings32 or longer (48-h) recordings,30,44 these methods are not in common clinical practice, and may be difficult to implement as patients may be reluctant to undergo more frequent or longer continuous BP recordings. Our study, on the other hand, set out to examine this question from the standpoint of everyday clinical practice, in which repeat ABPM recordings are requested as part of a diagnostic algorithm and used to guide appropriate clinical decisions.
We found no significant differences between genders in ABPM parameters, unlike other authors14,45 who reported greater BP variability in women than in men, but in agreement with others.15,42,43 The fact that we excluded the first hour of each ABPM recording from the analysis may have eliminated the alerting reaction that according to some authors14,45 may explain some of the differences observed between genders.
In the first ABPM recording in our study, around 45% of individuals were classified as D, 39% as ND, 8% as ED and 8% as RD. This distribution is similar to that seen in other studies.40 However, no more than 55% of D and ND maintained the same pattern on the second recording, and the percentage was even lower for those initially classified as ED or RD. Studies with similar sample sizes to ours22,46,47 found higher rates of persistence of dipper patterns, but in these studies only dipper and non-dipper patterns were analyzed, while our study extends this relatively low reproducibility to extreme and reverse dippers. This is important, because the division between dippers and non-dippers is too simplistic. Most of the studies cited above2,5,7,12–15,19–24,29,30,32,35–37,41–43,46 included extreme dippers among dippers and reverse dippers in non-dippers, but not only does each pattern represent a different level of cardiovascular risk, this simplification may overestimate the true reproducibility of dipper and non-dipper patterns. Our study shows that the overall low reproducibility of all circadian patterns must be taken into account if they are to be used as predictors of cardiovascular risk.
As in other studies,30 we found that the night/day BP ratio was lower in dippers who were still classified as such on the second recording than in those who changed from dipper to non-dipper. This suggests that analyzing the night/day ratio can help identify individuals who are likely to change from a dipper to a non-dipper pattern.
The present study has certain limitations. Although efforts were made to ensure that each subject experienced similar conditions for both ABPM recordings, it is not possible to exclude differences in ambient temperature, physical activity or quality of sleep, or changes in lifestyle or diet or other variables that could influence BP levels and circadian patterns in the medium term. However, the fact that BMI did not change significantly between the two recordings reduces, but does not eliminate, the risk that these variables influenced the results.
Several studies39,48–50 have shown that in terms of the predictive value of ABPM for assessing cardiovascular risk, the absolute value of nighttime BP, taken as a continuous variable, is a much stronger and more reliable predictor than any change in circadian pattern. This may be due to the low reproducibility of circadian patterns, in contrast to the excellent reproducibility of mean BP levels taken from ABPM recordings.
In conclusion, our study shows that in untreated subjects at low or moderate cardiovascular risk, ABPM has high reproducibility for mean values but not for circadian patterns between two ABPM recordings separated by less than 12 months. These findings, based on clinical practice, support the good reproducibility of mean ABPM values at an interval of up to one year. However, they also highlight the unreliability of predicting cardiovascular risk on the basis of circadian BP patterns.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Monte M, Cambão M, Mesquita Bastos JM, et al. Reprodutibilidade dos valores da pressurometria ambulatória de 24 horas e dos perfis circadiários de descida noturna registados com intervalo 1-11 meses em indivíduos não medicados. Rev Port Cardiol. 2015;34:643–650.